Description of the Efficacy and Safety of Three New Biologics in the Treatment of Rheumatoid Arthritis
Article information
Abstract
English articles on abatacept, golimumab, and tocilizumab in rheumatoid arthritis published between 2002 and 2009 were reviewed systematically. All randomized clinical trials, open-label extensions, meta-analyses, and reviews were examined. There were thirteen articles on abatacept, four on golimumab, and seven on tocilizumab. All three drugs were effective in methotrexate-naïve, methotrexate-incomplete responders, and tumor-necrosis-factor-failure rheumatoid arthritis patients. Of the three, only abatacept has been tested in a head-to-head trial with infliximab, in which it was found to be equivalent to infliximab. Golimumab resulted in a more modest improvement than the others in methotrexate-naïve patients, although no direct comparisons among the three drugs were possible or appropriate. Descriptive analysis of adverse events showed that patients receiving abatacept, golimumab, and tocilizumab were subject to more adverse events than controls overall, as expected. In the abatacept studies, a few cases of tuberculosis, more cardiovascular events and gastrointestinal bleedings and more basal cell carcinoma were seen. Golimumab was associated with more skin rashes and pneumonia, while tocilizumab was associated with increased lipids, more liver-function abnormalities, and neutropenia. These new medications are useful additions to the rheumatologic armamentarium and represent greater convenience (golimumab) or different mechanisms of action (abatacept and tocilizumab) than tumor-necrosis-factor inhibitors for treating rheumatoid arthritis. As expected, some adverse events occur when using these drugs and patients need to be watched carefully.
INTRODUCTION
Rheumatoid arthritis (RA) is an autoimmune disease characterized by chronic joint inflammation, which, if left untreated, may lead to bony erosions, deformity, joint destruction and disability. The therapies currently used to treat RA include non-steroidal anti-inflammatory drugs to manage pain and inflammation, disease-modifying anti-rheumaticdrugs (DMARDs) as a "first-line" therapy for newly diagnosed cases of RA, and biological-response modifiers, which are selective agents that specifically inhibit targeted molecules of the immune system. Glucocorticoids and other anti-rheumatic drugs are also used to treat RA. DMARDs include sulfasalazine, hydroxychloroquine, sulfasalazine, leflunomide, and methotrexate. Although DMARDs are effective, the goal of therapy should be remission (achieved in only 30 to 40%); therefore, development of new therapies is still needed.
Researchers are making a concerted effort to develop new immunomodulatory agents, specifically biological agents, which block the pro-inflammatory cytokines present in RA. These biological-response modifiers include inhibitors of tumor necrosis factor-alpha (TNF-α) (adalimumab, etanercept, and infliximab) [1,2], a recombinant inhibitor of interleukin (IL)-1 (anakinra) [3], a chimeric anti-CD20 monoclonal antibody (rituximab) [4], and a costimulation blocker (abatacept). Additional therapies for RA under current investigation include new TNF-α inhibitors, anti-IL-6-receptor monoclonal antibodies, and antibodies targeting proteins involved in B-cell function and survival.
We have chosen to examine three new biologics that have shown promise and play important roles in the treatment of RA. These new biologics include abatacept, golimumab, and tocilizumab. Abatacept, which is currently Food and Drug Administration (FDA) approved for RA treatment, functions by selectively modulating the CD80/CD86:CD28 co-stimulatory signal required for complete T-cell activation [5]. Golimumab, a full human anti-TNF-α monoclonal antibody, is also approved for the treatment of RA [6]. Finally, tocilizumab, the first anti-IL-6-receptor monoclonal antibody, has completed phase III clinical trials for RA and is awaiting FDA approval [7]. Abatacept, golimumab, and tocilizumab may be beneficial for treating RA in patients who do not respond to methotrexate or other disease-modifying anti-rheumatic drugs.
METHODS
The evidence for the efficacy and safety of abatacept, golimumab, and tocilizumab in the treatment of RA patients has been reviewed systematically. In this review, we focus primarily on a 28 joint disease activity score (DAS28) remission and 20% response on the American College of Rheumatology criteria (ACR20) as measures of efficacy, though other measures are also examined. To assess the tolerability of these new biologics, we include information regarding discontinuation, adverse events, serious adverse events, deaths, infections, cancers, acute infusion reactions, and special interest items for each of the three drugs. English language articles published from 2002 to July 2009 using PubMed were analyzed. Studies were included if they were randomized-control or open-label extension trials evaluating abatacept, golimumab, or tocilizumab alone or in combination with DMARDs, as compared with placebo or DMARDs alone. When available, systematic reviews or meta-analyses from randomized controlled trials were also included. Data were extracted on the effects of abatacept, golimumab, and tocilizumab on clinical outcomes. Results of this data extraction are summarized in tables and then synthesized.
The percentages included in the adverse effect tables (see Results section on safety) were derived from combining information found in the text, tables, and graphs of their respective cited articles. For some of the data found in the adverse effect tables, we used figures taken from the listed references to approximate the number and percentage of patients experiencing particular adverse events. This was especially important when evaluating lipid and liver enzyme changes among patients receiving golimumab and tocilizumab. Additionally, if a reference table did not list a particular adverse event, but the adverse event was addressed within the text of the reference, we added it to the total "n" for that particular adverse event subgroup and then calculated the percentages shown. If there were two different subgroups because different doses or routes of administration were used, these were added together and the percentages were calculated from the combined group. Furthermore, if there were two time periods in a drug study (e.g., an initial and crossover period), the initial period was used. For some non-serious infections, only the infections that were mentioned in the reference text or tables were incorporated into adverse effect tables, and a percentage was calculated from the total "n". We have categorized systemic disorders into life threatening and non-serious disorders for some systems. In those studies in which no such classification was available, we only included combined percentages. Adverse effect tables also group related laboratory abnormalities together into single categories; for example, liver function tests include transaminase and bilirubin values (this seemed reasonable as changes in bilirubin were extremely rare). Similarly, for lipid abnormalities, we included total cholesterol, low density lipoprotein (LDL), and triglycerides, solely for space reasons. "N/A" indicates that the data was not available. "N" is the total number of patients in all studies, and the percentages in parentheses represent the ranges encountered in individual studies.
RESULTS
Study characteristics
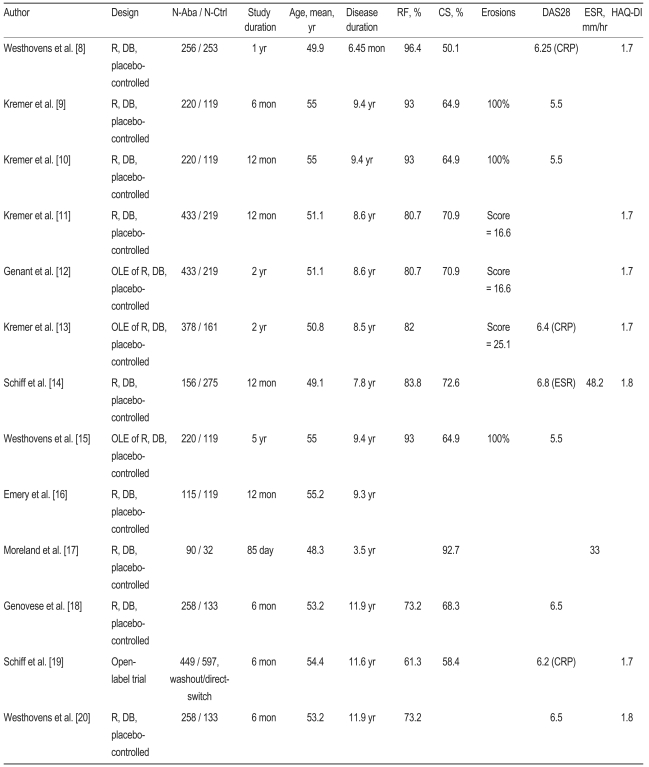
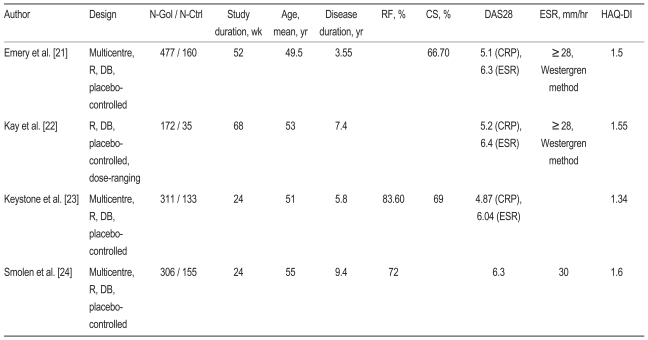
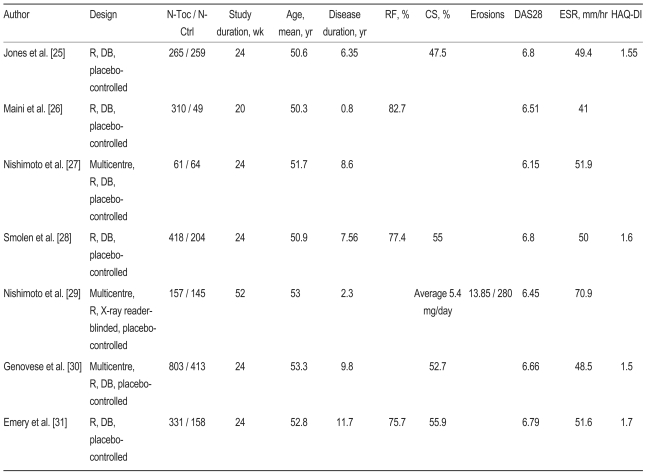
A total of 24 studies, four of which were open-label, met our inclusion criteria and examined abatacept (n = 13) [8-20], golimumab (n = 4) [21-24] and tocilizumab (n = 7) [25-31]. Within the abatacept studies, study durations ranged from 85 days to 5 years, with disease durations ranging from 6.45 months to 11.9 years (Table 1). The golimumab studies ranged from 24 to 68 weeks in duration, and participants in these trials had shorter disease durations than those in the abatacept trials, with a spread of 3.55 to 9.4 years (Table 2). Finally, the tocilizumab study durations ranged from 20 to 52 weeks, with disease durations ranging from 9.6 months to 11.7 years (Table 3). The mean age ranges of the study participants was 48.3 to 55.2 years in the abatacept studies, 49.5 to 55 years in the golimumab studies, and 50.3 to 53.3 years in the tocilizumab studies. Patients participating in the abatacept studies had similar baseline disease profiles overall, though some studies included a high percentage of rheumatoid factor positive patients [8-10,15], while others included a fairly high number of patients taking concomitant corticosteroids [11,12,14,17]. Patients in some abatacept studies also presented with fairly high baseline DAS28 scores [8,13,14,18-20]. At least two of the four golimumab studies included a fairly high percentage of patients using corticosteroids [21,23], and three of the four studies included patients with moderately high baseline DAS28 scores [21,22,24]. Similarly, almost all of the tocilizumab studies contained patients with high baseline DAS28 scores [25,26,28-31]. Most studies reported ACR20, 50, and 70 response rates as well as DAS28 response and remission rates, and safety data were generally adequately described.
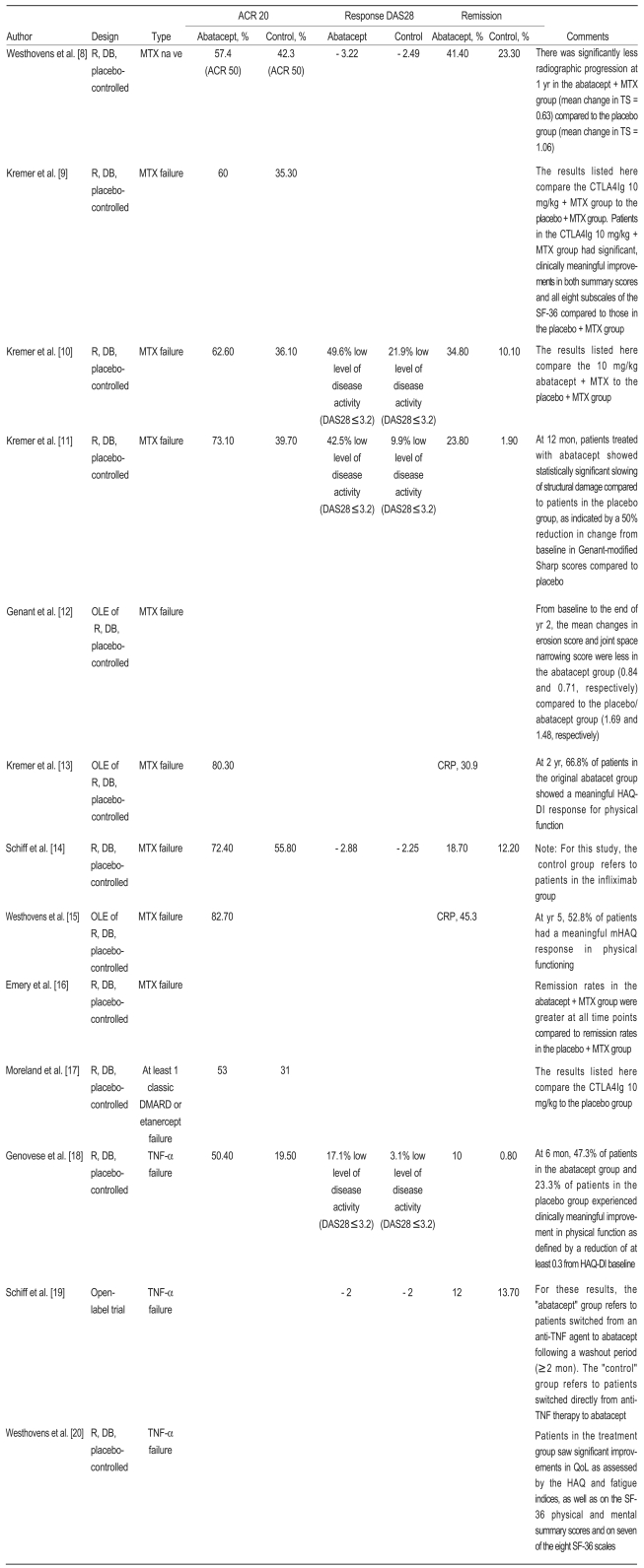
Efficacy: abatacept (Table 4)
Methotrexate (MTX) naïve
One of the 13 abatacept studies examined the efficacy of abatacept in MTX-naïve patients with early RA and poor prognostic factors [8]. In that study, Westhovens et al. [8] randomized participants 1 : 1 to receive either ~10 mg/kg abatacept plus MTX or a placebo plus MTX. In the abatacept group, 57.4% of patients achieved an ACR50 by the end of the study, compared to 42.3% in the placebo group. There was also a greater reduction in DAS28 in the abatacept group (- 3.22 vs. - 2.49), and 41.4% of patients in the abatacept group reached DAS-defined remission by the end of the study, compared to just 23.3% in theplacebo group. Of note, there was significantly less radiographic progression at 1 year in the abatacept plus MTX group (mean change in TS = 0.63), as compared to the placebo group (mean change in TS = 1.06).
MTX failure
Abatacept also shows promising efficacy in patients who have responded inadequately to MTX. Of the 13 abatacept studies examined, eight patients with active RA were enrolled despite MTX therapy [9-16]. Across studies, a significantly greater proportion of study participants in the abatacept groups achieved an ACR20 than did those in the placebo groups (Table 4) [9-11,14]. This ACR20 response appears to be maintained over time, as both a 2-year and a 5-year open-label extension study reported that over 80% of patients in the abatacept group achieved an ACR20 by the end of the study [13,15]. According to a 2002 study by Moreland et al. [17], patients who failed at least one classic DMARD (including MTX, gold, sufasalazine, chloroquine, D-penicillamine, azathioprine, leflunomide, or cyclosporine) or etanercept could also benefit from abatacept, as 53% of patients in the abatacept group achieved an ACR20, compared to 31% in the placebo group. Inadequate MTX responders receiving abatacept also appear to achieve DAS-defined remission at greater rates than do those not receiving abatacept. In the 2005 and 2006 studies conducted by Kremer et al. [10,11], 34.8% (2005) and 23.8% (2006) of patients in the abatacept groups achieved remission, compared to just 10.1%(2005) and 1.9% (2006) in the placebo groups. Similarly, Emery et al. [16] reported that remission rates in the abatacept group were greater than in the placebo group at all times during their study [16]. Of note, Schiff et al. [14] determined that, in inadequate responders to MTX, a greater proportion of patients receiving abatacept (18.7%) reached remission than did patients receiving infliximab (12.2%). As illustrated in Table 4, studies have shown that inadequate responders to MTX receiving abatacept rather than placebo also experience clinically meaningful improvements in both summary scores and all eight SF-36 subscales [9], statistically significant slowing of joint structural damage [11,12], meaningful Health Assessment Questionnaire-Disability Index (HAQ-DI) responses for physical functioning [13], and meaningful mHAQ responses for physical functioning [15].
TNF-α failure
In a 2005 study conducted by Genovese et al. [18], the investigators determined that patients who responded inadequately to TNF-α inhibitors could benefit from taking abatacept. In that study, 50.4% of patients in the abatacept group and only 19.5% of patients in the placebo group achieved an ACR20 by the end of the 6-month study. Additionally, 10% of patients in the abatacept group reached DAS-defined remission, whereas less than 1% of patients in the placebo were able to reach this milestone. Also at 6 months, 47.3% of patients in the abatacept group and 23.3% of patients in the placebo group experienced clinically meaningful improvement in physical function as defined by a reduction of at least 0.3 from the HAQ-DI baseline. According to Schiff et al. [19], a slightly greater proportion of patients achieve remission (13.7%) when they switch directly from inadequate anti-TNF-α therapy to abatacept, as compared to patients who switch to abatacept following a washout period of at least 2 months (12%). Other measures of efficacy also support the use of abatacept in patients who have failed prior TNF-α inhibitor therapy. For example, Westhovens et al. [20] observed that treatment group patients saw significant improvements in quality of life as assessed by the HAQ and fatigue indices, as well as on the SF-36 (short form 36) physical and mental summary scores and on seven of the eight SF-36 scales.
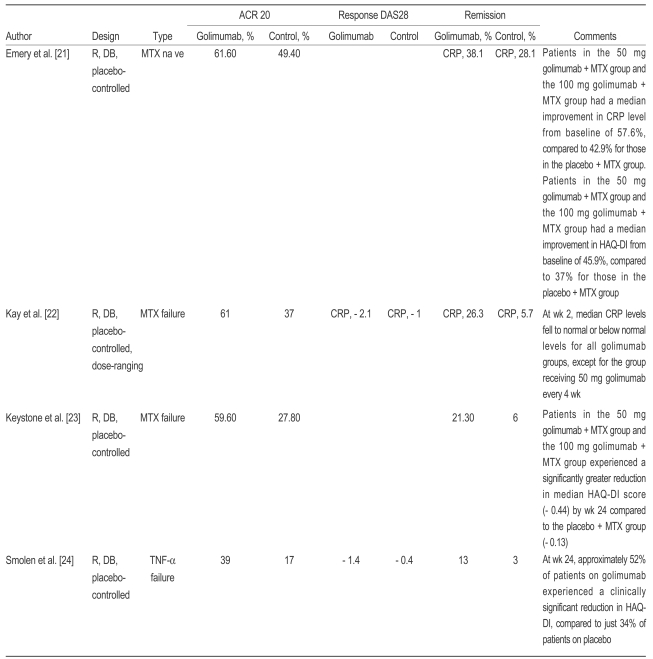
Efficacy: golimumab (Table 5)
MTX naïve
Of the four golimumab studies examined, one examined the efficacy of golimumab in MTX naïve patients with RA [21]. In this year-long study, Emery et al. [21] determined that 61.6% of patients in the golimumab group and 49.4% of patients in the placebo group obtained an ACR20 by the end of the investigation. Also, 38.1% of patients receiving golimumab achieved a DAS-defined remission using C-reactive protein (CRP) level, compared to 28.1% of patients in the placebo group. Patients who received golimumab also saw a median improvement in HAQ-DI from a baseline of 45.9%, while patients receiving placebo saw an improvement of 37%.
MTX failure
Golimumab also appears to be efficacious in patients who have failed to respond adequately to MTX treatment. Kay et al. [22] found that 61% of patients receiving golimumab and 37% of patients receiving a placebo achieved an ACR20 by the end of the 68-week study. Furthermore, DAS-defined remission rates were greater in those receiving golimumab (Table 5). The results of a 2009 study also support the efficacy of golimumab therapy in patients failing MTX treatment [23]. In this study, Keystone et al. [23] reported that 59.6% of patients in the golimumab group obtained an ACR20 during the study, while only 27.8% of patients in the placebo group did the same. More patients in the golimumab group (21.3%) achieved DAS-defined remission than did those in the placebo group (6%), which are similar to the results offered by Kay et al. [22].
TNF-α failure
Golimumab also seems to be of clinical use in patients who have failed TNF-α inhibitor treatment. In a 2009 study by Smolen et al. [24], of the patients failing TNF-α inhibitor therapy, 39% of those in the golimumab group and 17% of those in the placebo group reached an ACR20 by the end of the 24-week study. Thirteen percent of patients in the golimumab group reached DAS-defined remission by the end of the study, which was significantly more than the 3% of patients in the placebo group who achieved remission. At week 24, approximately 52% of patients on golimumab experienced a clinically significant reduction in HAQ-DI, compared to just 34% of patients on placebo.
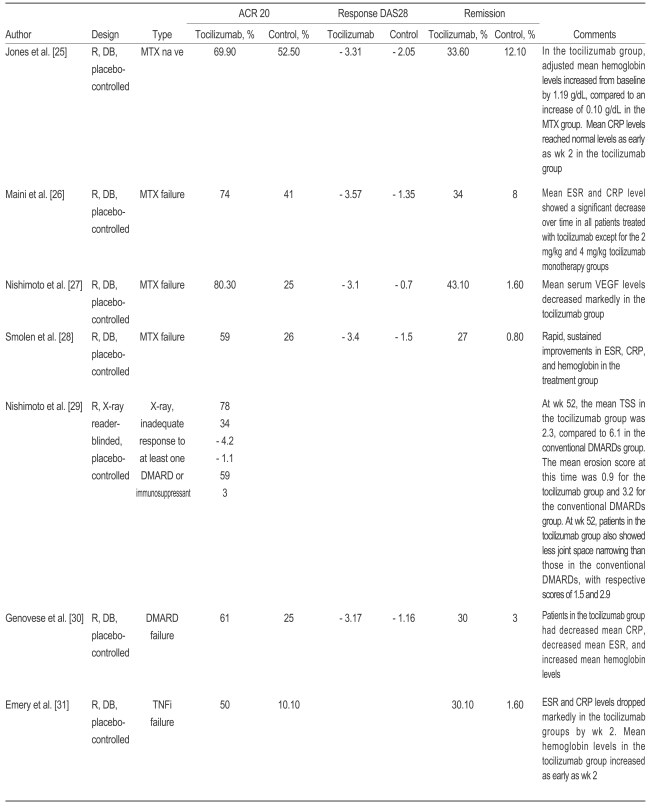
Efficacy: tocilizumab (Table 6)
MTX naïve
In their 2009 study, Jones et al. [25] examined the efficacy of tocilizumab in MTX naïve patients with RA. Nearly 70% of patients in the tocilizumab group were able to obtain an ACR20 by the end of the 24-week study, compared to 52.5% of patients in the control group. Additionally, 33.6% of patients in the tocilizumab group and only 12.2% of patients in the control group achieved DAS-defined remission during the study.
MTX failure
Tocilizumab also appears to show promising efficacy in patients with RA who have responded inadequately to MTX. Across studies, a greater proportion of inadequate responders to MTX treated with tocilizumab achieve an ACR20 than do inadequate responders to MTX in control groups (Table 6) [26-28]. Patients failing MTX treatment who receive tocilizumab also demonstrate rapid, sustained improvements in erythrocyte sedimentation rate (ESR), CRP, and hemoglobin than do patients assigned to control groups [26,28]. Nishimoto et al. [29] and Genovese et al. [30] suggest that this efficacy holds for patients failing with DMARDs other than MTX. For example, Nishimoto et al. [29] determined that 78% and 59% of patients receiving tocilizumab achieved an ACR20 and remission, respectively, while 34% in the control group achieved ACR20 and 3% achieved remission. That study also found that the mean erosion score at week 52 was 0.9 for the tocilizumab group and 3.2 for the control group, and that joint space narrowing was reduced in the tocilizumab group. Genovese et al. [30] reported similar ACR20 and remission rates, and suggested that patients in the tocilizumab group had decreased mean CRP, decreased mean ESR, and increased mean hemoglobin levels (Table 6).
TNF-α failure
One study investigated the efficacy of tocilizumab in patients who failed TNF-α inhibitor treatment. In a 2009 study, Emery et al. [31] reported that 50% of patients receiving tocilizumab and 10.1% of patients in the control group obtained ACR20. Also, 30.1% in the tocilizumab group and only 1.6% control group patients achieved remission by the end of the study. As with the MTX failure studies, patients who fail TNF-α inhibitor treatment and receive tocilizumab show significant reductions in ESR and CRP levels and increased hemoglobin levels [31].
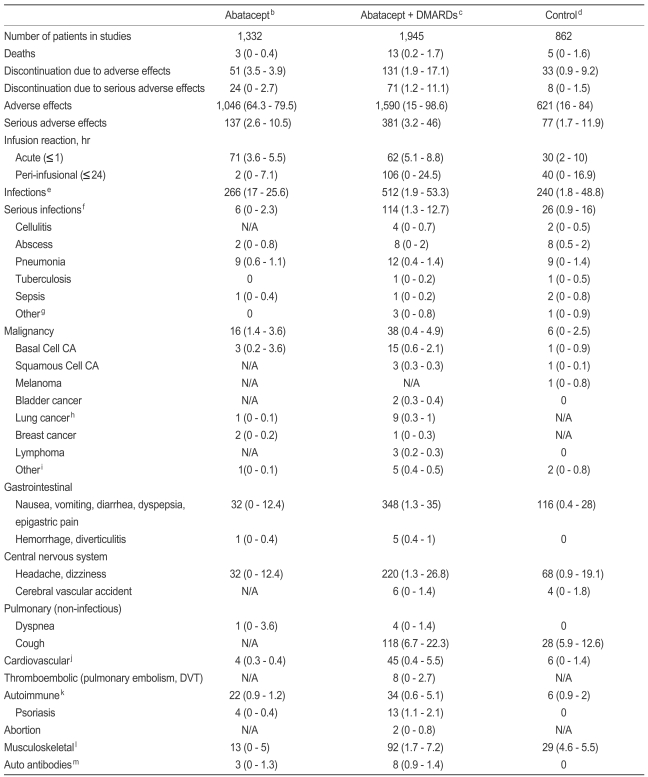
Safety: abatacept (Table 7)
While abatacept, golimumab, and tocilizumab are generally regarded as safe and well tolerated, the inherent immunosuppressive nature of these drugs requires caution in their use. We examined nine studies evaluating abatacept as either a monotherapy or in combination with DMARDs, and the results regarding safety are shown in Table 7 [8,10,11,13-16,18,19]. Given that these studies varied in design and methods for assessing safety outcomes, the results presented in Table 7 should be interpreted with caution. As expected, the combination of abatacept plus another DMARD was generally associated with more adverse events of all types, although the overlap of ranges indicates that the differences are not likely to be statistically significant. For example, patients in the abatacept plus DMARD category experienced more serious adverse effects (3.2 to 46%) than those in the control group (1.7 to 11.9%). Tuberculosis was observed in both the abatacept plus DMARDs group and the control group (one case in each group). Within the abatacept plus DMARDs group, both hemorrhage (0.4 to 1%) and cardiovascular complications (0.4 to 5.5%) occurred, but not statistically more often than in the control group (0.0% and 0.0 to 1.4%, respectively).
Table 7 delineates a particularly interesting set of observations regarding malignancies. Malignancy rates in both the abatacept only group (1.4 to 3.6%) and the abatacept plus DMARDs group (0.4 to 4.9%) overlapped considerably with malignancy rates in the control group (0.0 to 2.5%), implying little to no difference in malignancy risk among these three groups. However, an evaluation of the specific malignancy types suggested the possibility that some tumors were more common when using abatacept. These data approach statistical significance and raise the possibility that more data should be gathered for these cancers. Rates of basal cell carcinoma in the abatacept only and abatacept plus DMARDs groups (0.2 to 3.6%) occurred at a greater frequency than in the control group (0.0 to 0.9%). Also, three cases of squamous cell carcinoma were observed in the abatacept plus DMARDs group, compared to just one case in the control group. Additionally, three patients in the abatacept plus DMARDs group developed lymphoma, whereas no patients in the control group experienced this complication. Finally, three patients within the abatacept only and abatacept plus DMARDs groups developed breast cancer, and 10 patients developed lung cancer.
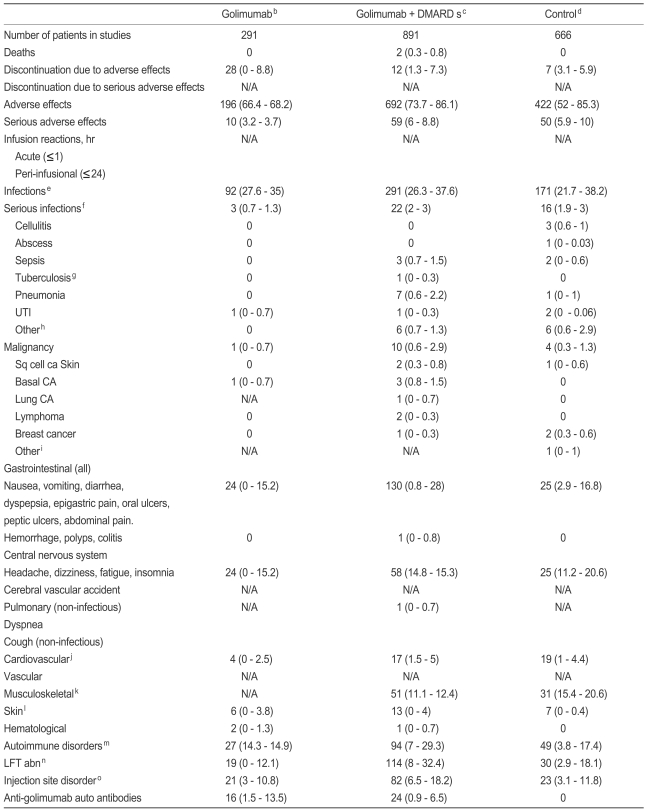
Safety: golimumab (Table 8)
We examined four studies evaluating golimumab as either a monotherapy or in combination with DMARDs. The safety data are combined and displayed in Table 8 [21-24]. Again, we limit our discussion to selected observations from Table 8, and do not imply that any of these observations are of statistical significance. Rather, they are presented as clinical considerations to consider when using this biologic. Patients receiving golimumab alone or golimumab plus DMARDs experienced more adverse skin events (0.0 to 4.0%) than the control group (0.0 to 0.4%). Similarly, patients receiving golimumab plus DMARDs had more pneumonia (0.6 to 2.2 vs. 0.0 to 1.0% for control), malignancy (0.6 to 2.9 vs. 0.3 to 1.3% for control),and basal cell carcinoma (0.8 to 1.5 vs. 0.0% for control).
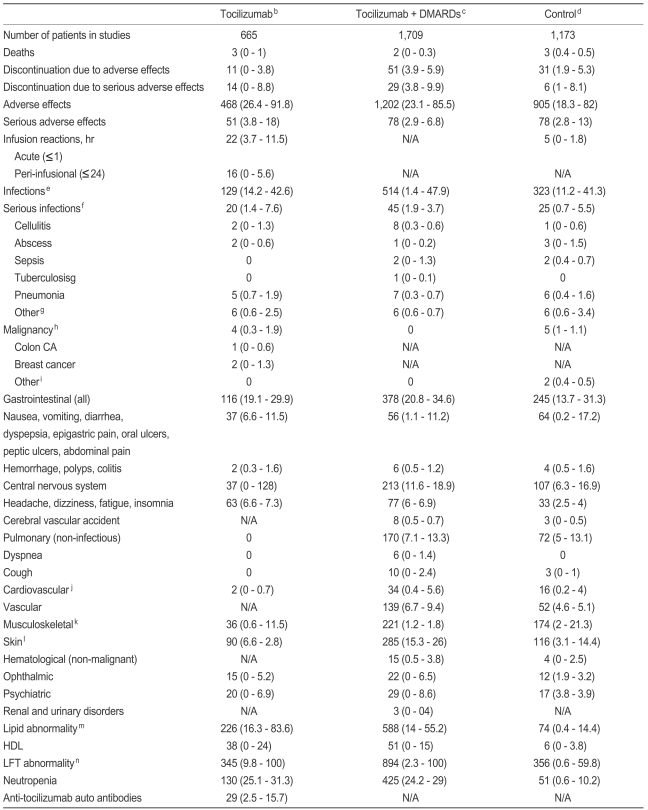
Safety: tocilizumab (Table 9)
To evaluate the safety of tocilizumab, we examined seven studies investigating the biologic alone or in combination with DMARDs [25-31]. The results of these studies are presented in Table 9. Our discussion of Table 9 is limited to selected clinical observations and does not imply statistical significance. Patients using tocilizumab monotherapy generally experienced more adverse effects (26.4 to 91.8%) and serious adverse effects (3.8 to 18%) than those in the control group (18.3 to 82% and 2.8 to 13%, respectively). Perhaps most interesting in Table 9 is the apparent increase in high density cholesterol (HDL), total cholesterol, and liver function test abnormalities, and neutropenias in patients receiving tocilizumab alone or tocilizumab plus DMARDs than control group patients. Between 0.0 and 24% of patients in the tocilizumab and tocilizumab plus DMARDs group saw HDL increases, compared to just 0.0 to 3.8% of patients in the control group. Similarly, in the tocilizumab and tocilizumab plus DMARDs groups, a greater number of patients experienced lipid abnormalities (14 to 83.6%) and liver function test abnormalities (2.3 to 100%) than did those in the control group (0.4 to 14.4% and 0.6 to 59.8%, respectively). While only 0.6 to 10.2% of patients in the control group exhibited neutropenia, between 24.2 and 31.3% of patients in the tocilizumab and tocilizumab plus DMARDs groups showed this side effect. Of note, these ranges did not overlap. Taken together, these observations suggest that physicians should consider HDL increases, lipid and liver function test abnormalities, and neutropenia when using tocilizumab.
CONCLUSION
Abatacept, golimumab, and tocilizumab represent three new drugs targeting specific biological molecules to treat RA. Abatacept demonstrates acceptable safety and tolerability, and clinically meaningful efficacy in patients who are MTX naïve or who have had an inadequate response to prior conventional DMARDs or TNF-α inhibitor therapy. Golimumab effectively reduces the signs and symptoms of RA and is generally well tolerated in patients who are MTX naïve or who have failed conventional DMARD or TNF-αinhibitor treatment. Similarly, tocilizumab has been shown to be effective for improving the signs and symptoms of RA and has a safety profile similar to abatacept and golimumab, although it causes reversible increases in triglycerides, LDL-cholesterol, and liver enzymes. Despite these encouraging results, the place for each of these drugs in the RA armamentarium is not fully understood given the lack of head-to-head studies and long-term extension data.
Notes
No potential conflict of interest relevant to this article was reported.