Endoscopic findings around the gastroesophageal junction: an experience from a tertiary hospital in Korea
Article information
Abstract
Background/Aims
Important lesions related to gastroesophageal reflux disease (GERD) are located around the gastroesophageal junction (GEJ). This study examined the distribution of endoscopic findings around the GEJ and elucidated their relationship to each other and esophageal manometric features.
Methods
Endoscopic data were collected prospectively from 2,450 consecutive diagnostic upper gastrointestinal endoscopies. The presence and degree of hiatal hernia (HH), columnar-lined esophagus (CLE), and reflux esophagitis (RE) were recorded. Esophageal manometric data were collected from 181 patients.
Results
The prevalence of HH, CLE, and RE was 9.8, 18.8, and 9.9%, respectively. Of all HH and CLE cases, 62.8 and 98.9%, respectively, were of the short-segment variety. Of all RE cases, 95.0% were mild. Younger age, male gender, the presence of HH, and a higher gastroesophageal flap valve (GEFV) grades were associated with the presence of RE. Increased ZAP grades were associated with increased prevalence and grades of HH, CLE, and RE. Higher GEFV grades were associated with increased prevalence and grades of HH, CLE, and RE. Lower esophageal sphincter pressure (LESP) decreased in patients with HH or RE compared to those without HH or RE.
Conclusions
Endoscopic findings around the GEJ revealed that a substantial proportion of our patients showed features potentially related to GERD. In combination with other recent reports, our study implies that Korea is no longer a very-low-prevalence area of GERD, although it may predominate in silent or milder forms.
INTRODUCTION
The gastroesophageal junction (GEJ) plays a crucial role as a gatekeeper against gastroesophageal reflux, and most clinically important lesions related to gastroesophageal reflux disease (GERD) are located in this area. Therefore, the importance of careful examination of the GEJ during routine diagnostic upper gastrointestinal (UGI) endoscopy cannot be overemphasized.
Several frequently used classification systems describe aspects of endoscopic findings around the GEJ, including the Los Angeles (LA) classification for reflux esophagitis (RE)1) and grading systems for the Z-line appearance (ZAP)2) and gastroesophageal flap valve (GEFV) morphology3). This study explored the distribution of endoscopic findings around the GEJ and elucidated their relationship to each other and esophageal manometric findings.
MATERIALS AND METHODS
Study population
Data were collected prospectively from 2,450 consecutive patients visiting the gastroenterology clinic of one author (YTB) and undergoing their first routine diagnostic UGI endoscopy for various reasons at Korea University Guro Hospital, Seoul, Korea from March 2004 to April 2006. Those who underwent urgent or therapeutic endoscopies or who had previously undergone UGI endoscopies at Korea University Guro Hospital were excluded, as were patients with gastric outlet obstruction.
Endoscopic assessment
All endoscopies were performed by one experienced endoscopist (YTB). Endoscopic findings around the GEJ were described separately, including the presence or absence and degree of hiatal hernia (HH), columnar-lined esophagus (CLE), and RE.
HH and CLE were assessed during insertion of the endoscope with minimum air inflation. The GEJ was defined endoscopically as the distal end of longitudinally arrayed palisade capillaries4), or, if it was unclear, the proximal end of the gastric type mucosal folds5). The patient was diagnosed with HH if the GEJ was located at least 0.5 cm proximal to the level of the diaphragmatic pinchcock action. HH was divided into two grades: short-segment HH if the length was shorter than 2 cm, and long-segment HH if otherwise. The patient was diagnosed with CLE if columnar-looking mucosa was observed proximal to the GEJ4) and was at least 0.5 cm in length. CLE was divided into two grades, short-segment CLE if the length was shorter than 3 cm, and long-segment CLE if otherwise.
Reflux esophagitis and ZAP were observed during both insertion and withdrawal of the endoscope, with maximal air inflation of the lower esophagus in full inspiration if possible. Reflux esophagitis was diagnosed and graded according to the LA classification1). The Z-line was observed carefully for any tongue-like projections or islands of columnar epithelium proximal to the Z-line. ZAP was defined and graded according to Wallner et al2). GEFV with a mucosal fold or ridge surrounding an endoscopic shaft was observed in the retroflexed view and was graded according to Hill et al3).
Esophageal manometry
Routine esophageal manometry was performed in patients showing symptoms suggestive of esophageal motility disorders, such as dysphagia or chest pain. The manometric data were transferred to a computer via a polygraph (Polygraf ID; Medtronic Functional Diagnostics, Skovlunde, Denmark) and pressure transducers (DPT-6000; Smiths Medical Deutschland, Kirshseeon, Germany), which were connected to an eight-channel water perfusion catheter (Medtronic Functional Diagnostics) and a low-compliance pneumohydraulic capillary infusion system (PIP 3-8; Sandhill Scientific, Colorado, USA). The manometric data were reviewed using analysis software (Polygram NET version 4.1; Medtronic Functional Diagnostics), and the lower esophageal sphincter pressure (LESP) was measured using the station pull-through technique. Esophageal peristalsis was evaluated after each of the last 10 of 15 swallows of 5 mL of water, and the distal esophageal peristaltic amplitude (DEA) was measured at 3 and 8 cm proximal to the lower esophageal sphincter.
Statistical analysis
Statistical analysis was performed using SPSS (version 13.0 for Windows, Chicago, IL, USA). Data were expressed as the mean±standard deviation (SD). One-way analysis of variance (ANOVA) was used to assess statistical significance for age, body mass index (BMI), and esophageal manometry parameters according to HH, CLE, ZAP, and GEFV status. Age, BMI, and esophageal manometry parameters were compared among patients with or without HH, CLE, and RE, and among groups with different ZAP and GEFV grades, using unpaired t-tests. Differences in HH, CLE, and RE according to ZAP and GEFV grades and the relationship between ZAP and GEFV grades were assessed using the chi-square test for trend. Spearman's rank correlation coefficient was calculated to examine the correlation between GEFV and RE grades, ZAP and RE grades, and HH and RE grades. To evaluate the ability of the variables of interest to predict CLE and RE, a logistic regression analysis model was used. The LESP and DEA values were compared using one-way ANOVA or unpaired t-tests using log-transformed data. p<0.05 was considered statistically significant.
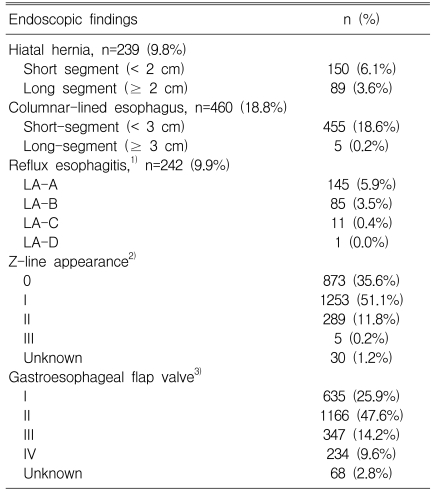
RESULTS
Endoscopic data were collected from 2,450 patients (1,152 men and 1,298 women, age 51.4±13.7 years). The prevalence of endoscopic HH, CLE, and RE was 9.8, 18.8, and 9.9%, respectively. Short-segment HH made up 62.8% of all HH cases, whereas short-segment CLE made up 98.9% of all CLE cases. Of all RE cases, 95.0% showed grades LA-A or B. ZAP grade I and GEFV grade II were the most common types, occurring in 51.1 and 47.6% of patients, respectively (Table 1).
The age and BMI of patients with endoscopic CLE were significantly higher than in those without endoscopic CLE, although the differences were not large. Male gender, the presence of HH or RE, and higher ZAP (grade II or III) or GEFV (grade III or IV) grades were all significantly associated with the presence of endoscopic CLE in the univariate and multivariate analyses (Table 2).

Clinical and endoscopic features of patients with or without endoscopic columnar-lined esophagus (n=2,450).
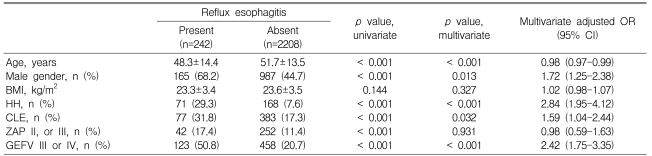
Patients with RE were significantly younger than those without RE, although the difference was not large. No significant difference in BMI was observed between those with or without RE. Male gender, the presence of HH or CLE, and high GEFV grades (III or IV) were significantly associated with the presence of RE in the univariate and multivariate analyses. Higher ZAP grade (II or III) was significantly associated with the presence of RE in the univariate analysis, but not in the multivariate analysis (Table 3).
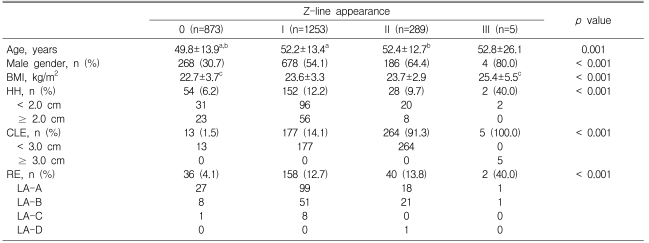
Patients with ZAP grades of I or II were significantly older than those with ZAP grades of 0, and males were more likely to have high ZAP grades. Patients with ZAP grade III had a higher BMI than those with ZAP grades of 0. An increase in ZAP grade was also significantly associated with the increased prevalence of HH, CLE, and RE (Table 4). Increased HH, CLE, and RE grades were all correlated with increased ZAP grades (Spearman's rank correlation, r=0.075 and p<0.001, r=0.548 and p<0.001, and r=0.141 and p<0.001, respectively).
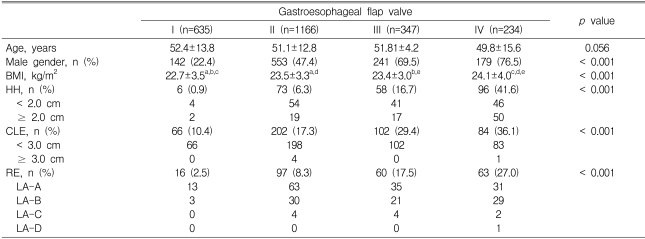
No difference was observed in GEFV grade according to age, although increased GEFV grade was significantly associated with male gender. BMI was also significantly higher in patients with GEFV grades of IV compared to those with lower GEFV grades, and increased GEFV grades were significantly associated with the increased prevalence of HH, CLE, and RE (Table 5). Higher HH, CLE, and RE grades were all significantly correlated with higher GEFV grades (Spearman's rank correlation, r=0.325 and p<0.001, r=0.198 and p<0.001, and r=0.231 and p<0.001, respectively). Higher GEFV grades were correlated with higher ZAP grades (Spearman's rank correlation, r=0.271, p<0.001; Table 6).
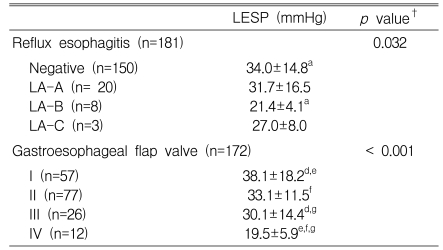
Esophageal manometric data from 181 patients (68 men and 113 women) that underwent both upper endoscopy and esophageal manometry were analyzed. LESP was significantly lower in patients with HH or RE than in patients without HH or RE. Patients with high GEFV grades (III or IV) had significantly lower LESP and DEA values. LESP and DEA did not differ between patients with or without endoscopic CLE or between patients with lower versus higher ZAP grades (Table 7).
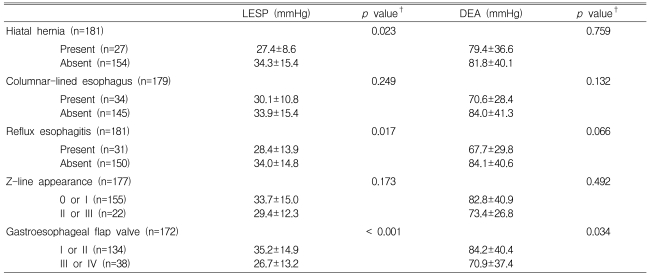
Lower esophageal sphincter pressure (LESP) and distal esophageal contraction amplitude (DEA) according to endoscopic findings
In patients with LA-B grade RE, LESP was significantly lower than in patients without RE, and there was a negative correlation between LESP and GEFV grade (Table 8). No difference in LESP was observed according to the grade of HH, CLE, or ZAP.
DISCUSSION
Recent epidemiologic studies indicate that RE is on the rise in Asia, with a reported prevalence of 3~16%6-8). However, most cases (80~95%) present in a relatively mild form (LA-A or B)6, 9). In our study, the prevalence of RE was 9.9%, and 95.0% of these cases were mild. Although our data may not represent the general Korean population, recent reports from other Korean cities obtained similar data for the prevalence of erosive RE10, 11).
Younger age, male sex, the presence of HH or CLE, and higher GEFV grade were significantly associated with the presence of RE in our study. There are several reported pathogenic factors for RE, including low LESP, short LES length (especially the intra-abdominal portion), disturbed esophageal acid clearance, and transient LES relaxation12-16). Our data suggest that patients with RE were younger than those without RE; although the explanation for this is unclear, it may be due to an alpha error resulting from a very large sample size. In addition, although the difference was statistically significant, it may not be large enough to be clinically relevant. Several studies have reported that LESP and esophageal motor activity become progressively impaired with increasing severity of RE17, 18). We found a significantly lower LESP in patients with RE compared to those without RE. In addition, our study demonstrated a progressive decrease in LESP with increasing RE grade, suggesting a probable correlation between lower LESP and RE.
Hiatal hernia is thought to predispose patients to GERD via various mechanisms, such as low LESP and impaired acid clearance from the esophagus19, 20). Our results are consistent with previous reports and demonstrate correlations between the presence of HH and RE and lower LESP.
The definition of endoscopic CLE is controversial as it depends on the definition of the precise point at which the esophagus ends and the stomach begins. Generally, the endoscopic GEJ is defined as the proximal end of the gastric folds in addition to the distal end of the fine longitudinal vessels4, 5, 21). We diagnosed endoscopic CLE if the length of columnar-lined mucosa proximal to the distal margin of the palisade zone on the lower esophagus was 0.5 cm or longer; if it was unclear, the proximal end of the gastric type mucosal folds was used as an indicator of the GEJ instead. We adopted an arbitrary threshold of 0.5 cm to avoid overdiagnosis, considering a potential gap of several millimeters between the "true" GEJ and the distal margin of the palisade zone5). The prevalence of endoscopic CLE in our study was 18.8%, and almost all patients showed the short-segment variety. Based on our previous experience, about one-third of endoscopic CLE cases would be diagnosed as Barrett's esophagus after histological examination with non-targeted biopsy specimens22).
In this study, older age, male gender, higher BMI, the presence of HH, the presence of RE, and higher GEFV grades were significantly associated with the presence of endoscopic CLE. These findings have implications for the association between gastroesophageal reflux and the presence of endoscopic CLE. Again, the discrepancy in age between RE and CLE cannot be explained clearly. However, as noted in patients with RE, the difference in age according to the presence or absence of CLE may not be large enough to be clinically significant. In addition, we did not detect a correlation between the presence of endoscopic CLE and manometric parameters, such as LESP and DEA.
Wallner et al.1) first proposed the ZAP classification, a 4-grade system for the appearance of the endoscopic Z-line. This system is correlated with the prevalence of intestinal metaplasia in the GEJ and GERD symptom frequency23-25). In our study, the presence of HH, CLE, higher RE grades, and higher GEFV grades were all significantly correlated with ZAP grades. These results suggest that the ZAP classification is an indicator of pathological changes in the GEJ and gastroesophageal reflux.
The GEFV, the sling or oblique fibers of the stomach located below the LES, contribute to the barrier function via a flap valve mechanism. Since Hill et al.2) developed an endoscopic grading system to assess the GEFV, several reports have noted a correlation between increased GEFV grades and the increased prevalence of GERD and Barrett's esophagus10, 26, 27). We found that male gender was associated with higher GEFV grades and our data confirm the association between an increased GEFV grade and the increased prevalence and grade of HH, CLE, and RE. These results suggest that GEFV grading may permit the endoscopic evaluation of gastroesophageal reflux status. We also found a negative correlation between GEFV grade and LESP level, implying that increasing GEFV is associated with the deterioration of LES function.
In conclusion, endoscopic findings around the GEJ revealed that a substantial proportion of our patients showed features potentially related to GERD. Combined with other reports10, 11), these results suggest that Korea is no longer a very-low-prevalence region for GERD, although the disease may predominate in silent or milder forms.