Additive effect of probiotics (Mutaflor) on 5-aminosalicylic acid therapy in patients with ulcerative colitis
Article information
Abstract
Background/Aims
In ulcerative colitis (UC) patients, Escherichia coli Nissle 1917 (EcN) is equivalent to mesalazine for preventing disease relapse; however, evidence of the ability of EcN to increase health-related quality of life or induce remission remains scarce. We investigated the efficacy of EcN as an add-on therapy for UC.
Methods
In this multicentre, double-blind, randomised, placebo-controlled study, a total of 133 UC patients were randomly assigned to receive either EcN or placebo once daily for 8 weeks. Inflammatory bowel disease questionnaire (IBDQ) scores (primary endpoint) and clinical remission and response rates (secondary endpoints) were compared (Clinical trial registration number: NCT04969679).
Results
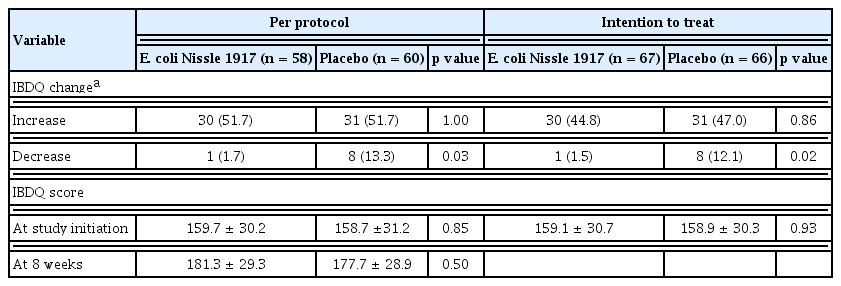
In total, 118 patients (EcN, 58; placebo, 60) completed the study. The number of patients reaching the primary endpoint did not differ between the EcN and placebo groups (30 [51.7%] vs. 31 [51.7%]; per-protocol analysis, p = 1.0; intention-to-treat analysis, p = 0.86). However, significantly fewer patients in the EcN group exhibited a decreased IBDQ score (1 [1.7%] vs. 8 [13.3%]; per-protocol analysis, p = 0.03; intention-to-treat analysis, p = 0.02). Moreover, a significantly higher number of patients in the EcN group displayed clinical response at 4 weeks (23 [39.7%] vs. 13 [21.7%], p = 0.04) and endoscopic remission at 8 weeks (26 [46.4%] vs. 16 [27.1%], p = 0.03).
Conclusions
Although the number of patients reaching the primary endpoint did not differ between the EcN and placebo groups, EcN was found to be safe and effective in preventing the exacerbation of IBDQ scores and achieving clinical responses and endoscopic remission in patients with mild-to-moderate UC.
INTRODUCTION
Inflammatory bowel disease (IBD), including ulcerative colitis (UC), is a group of chronic relapsing inflammatory disorders of the gastrointestinal tract characterised by a multifactorial aetiology. It has been proposed that an excessive mucosal immune response to commensal gut bacteria drives such inflammatory process in genetically susceptible individuals [1]. Considering current evidence that the intestinal microbiota is involved in the pathogenesis of IBD, considerable research efforts have been made in recent decades for developing appropriate strategies to manipulate the gut microbial composition [2–4]. In particular, probiotics that modulate microbial composition could be beneficial for IBD treatment [5,6].
Escherichia coli Nissle 1917 (EcN) is a non-pathogenic gram-negative bacterium belonging to the Enterobacteriaceae family [7]. In contrast to other E. coli strains, this strain does not produce virulence factors and reduces colonic mucosal damage by stimulating the production of human beta-defensin 2, a crucial molecule that protects the mucosal barrier against adhesion and invasion of pathogenic bacterial species [8].
Owing to its beneficial effects on intestinal homeostasis, EcN is one of the most investigated probiotics in patients with UC [6,9]. In a meta-analysis of randomised clinical trials (RCTs) assessing the effect of EcN treatment in patients with UC [9], EcN was found to be equivalent to mesalazine in preventing disease relapse. Moreover, EcN appeared to be as effective as the controls in inducing remission. However, it should be noted that only one study compared the use of EcN against that of a placebo; in contrast, other probiotics such as VSL#3 showed higher or equivalent remission rates than a placebo in four distinct RCTs [6]. Hence, additional evidence on the effectiveness of EcN is required prior to its recommendation for clinical use. Accordingly, recent Korean guidelines recommend the use of EcN solely for remission maintenance, not for remission induction, and only as an alternative treatment when 5-aminosalicylic acid (5-ASA) cannot be administered due to adverse reactions [10]. Further studies are needed to evaluate the ability of EcN to induce remission compared with that of a suitable placebo. The objective of the present study was to investigate the additive effect of EcN administration on 5-ASA treatment, and whether EcN therapy could influence the clinical outcomes and health-related quality of life (HRQoL) of patients with UC when compared with placebo therapy.
METHODS
A multicenter, double-blind, randomised, placebo-controlled study was conducted in a population of patients with mild-to-moderate UC. The study protocol was approved by the investigational review board of each center involved in the study (Kangbuk Samsung Hospital IRB no: KBSMC 2017-11-032) and was registered at www.clinicaltrials.gov (NCT04969679). Written informed consent was obtained from all patients.
Sample size
The sample size was calculated based on a power of 80% and a statistical significance (α) of 95% (p = 0.05). An increase of > 16 points in the inflammatory bowel disease questionnaire (IBDQ) score at 8 weeks was expected to occur in 50% of patients treated with EcN, while a 25% response rate was expected in patients treated with the placebo. This projection was based on Cochrane review data, where improvements in IBDQ score are defined as an increase of ≥ 16 points from the baseline [11]. Furthermore, the rate of IBDQ score increase by ≥ 16 points has been reported to be 37% to 69% for patients treated with antibodies against tumour necrosis factor (anti-TNF) and 23% to 50% for placebo-treated patients [11]. We assumed that probiotics would be less effective than anti-TNF in increasing IBDQ scores. Based on these assumptions, 58 patients were required in each group, with an additional 20% of patients to account for dropouts; hence, a total of 150 patients were to be enrolled in the trial.
Study procedures
The study procedures were conducted for each enrolled patient. At the screening visit, the demographic characteristics, medical history, and current medications of each patient were recorded. Moreover, individual disease activity scores (i.e., Mayo scores) were calculated by the investigator, together with individual scores for four parameters, namely bowel frequency, rectal bleeding, endoscopic score, and physician’s severity rating [12]. All patients completed the IBDQ [13] for HRQoL assessment. In addition, stool collection for microbiome analysis and sigmoidoscopies for endoscopic examination were performed at the trial onset.
Eligible patients were randomly assigned to receive either EcN or placebo once daily for 8 weeks. Patients were enrolled in each centre according to the randomisation list. A randomisation number was strictly assigned according to the order of patient enrolment, which was performed in a double-blind fashion using 1:1 allocation to the two groups (permuted block randomisation).
After randomisation, patients underwent detailed physical examination and history assessment during two visits at 4 and 8 weeks. A partial Mayo score was recorded after 4 weeks. At the end of the trial period (8 weeks), the Mayo and IBDQ scores were recorded, and stool collection and sigmoidoscopy were performed.
All adverse events were documented by supplying the study participants with diary cards to daily assess and record their symptoms, such as stool frequency (SF), bleeding, and abdominal pain (AP). The investigators assessed the participants’ compliance by counting the unused sachets returned by the patients at weeks 4 and 8.
Inclusion and exclusion criteria
Patients with UC, aged 19 years or older, using 5-ASA and presenting mild-to-moderate active UC (Mayo score, 3 to 9) that extended for more than 15 cm from the anal verge, and thus not classifiable as proctitis, were considered eligible for participation. The following exclusion criteria were applied: UC limited to proctitis; use of medications other than 5-ASA, such as immunomodulators, steroids, or biologics, within 3 months; use of antibiotics or probiotics within 2 weeks; and history of bowel resection. In addition, patients requiring hospitalisation and imminent surgical intervention, as well as lactating and pregnant women, were excluded.
Treatment
Patients meeting the inclusion criteria were randomly assigned to one of the two treatment groups and received either EcN or placebo for 8 weeks, in addition to their standard pharmaceutical therapy, that is, 5-ASA. EcN (Mutaflor, BL&H Co. Ltd., Seoul, Korea) is available as sachets containing the E. coli strain Nissle 1917 at a dose of 2.5 × 109 colony forming units (CFU). In the present study, EcN was provided in sealed single-dose plastic sachets, and the placebo was supplied in identical sachets. Patients were required to consume the contents of the sachets in the morning and take one capsule/day from day 1 to day 4 and two capsules/day from day 5.
Concomitant treatments
Patients who were taking 5-ASA orally or as suspension enemas continued therapy at stable doses. Importantly, 5-ASA doses were to be maintained for 8 weeks, and any change in 5-ASA dosing during the 8-week study period was considered a protocol violation. Other medications, such as steroids, antibiotics, probiotics, and antidiarrheal drugs, were not administered.
Primary endpoint
The primary endpoint depicted the beneficial effects of EcN in patients with mild-to-moderate UC, in terms of an increase in the IBDQ score of > 16 points from the baseline at 8 weeks.
Secondary endpoints
The secondary endpoints represented possible beneficial effects of EcN on the following parameters of UC activity: (1) clinical remission, that is, partial Mayo score, assessed at week 4, ≤ 1 or Mayo score, assessed at week 8, ≤ 2; (2) clinical response, that is, decrease in the partial Mayo score, assessed at week 4, by more than two points, or decrease in the Mayo score, assessed at week 8, by more than three points; (3) improved endoscopic scores and endoscopic remission, as revealed by an endoscopic subgroup Mayo score = 0 at week 8; (4) endoscopic response, as revealed by a decrease in the endoscopic subgroup score of more than one point at week 8; and (5) changes in the microbial composition of stools, including diversity and taxonomy.
DNA extraction and bacterial 16S rRNA gene sequencing
Participants were required to collect faecal samples 24 hours before visiting the hospital and to store them at −20°C immediately after defecation. Samples deposited by the participants after arrival at the hospital were then immediately stored in a deep freezer (−70°C) at the laboratory. Detailed methods, including those of DNA extraction from stool samples and 16S rRNA gene sequencing, are reported in the Supplementary Methods.
Statistical analysis
Continuous variables are presented as the mean±standard deviation. Categorical variables are presented as numbers and percentages. Differences in the baseline characteristics, primary endpoint, and secondary endpoints between the groups were compared using chi-square test for categorical variables and Student’s t test for continuous variables. The primary endpoint was analysed via both a per-protocol (PP) and an intention-to-treat (ITT) method; secondary outcomes were analysed using a PP method. Statistical significance was set at p < 0.05. SPSS version 20.0 (IBM Corp., Armonk, NY, USA) was used for statistical analyses. The details of stool microbiome analysis are reported in the Supplementary Methods.
RESULTS
Participant flow
A total of 134 patients were initially enrolled in the study, but one patient withdrew before treatment assignment. Therefore, 133 patients (67 in the EcN group and 66 in the placebo group) were eventually enrolled. However, in the EcN group, nine patients withdrew during follow-up, four experienced a worsening of UC symptoms, one presented with other adverse events, and four withdrew their informed consent for study participation. Moreover, six patients in the placebo group withdrew during follow-up, among which four experienced a worsening of UC symptoms, one experienced other adverse events, and one withdrew informed consent (Fig. 1). In total, 58 patients in the EcN group and 60 in the placebo group completed the study.
Baseline data
The clinical characteristics of patients in the two groups were comparable (Table 1). Indeed, no significant differences were observed in terms of demographic characteristics. At the beginning of the study, no differences were observed in the systemic or topical use of 5-ASA between the two groups. In particular, except for one patient in the EcN group and two patients in the placebo group taking balsalazide, all patients were administered mesalamine.
Primary endpoint
Overall, EcN was not superior to placebo in increasing the IBDQ scores of mild-to-moderate UC (30 [51.7%] vs. 31 [51.7%], respectively; PP, p = 1.0; ITT, p = 0.86). (Table 2) At the beginning of the study, the IBDQ scores were 159.7 ± 30.2 for the EcN group and 158.7 ± 31.2 for the placebo group (p = 0.85); after 8 weeks, the scores were 181.3 ± 29.3 and 177.7 ± 28.9 (p = 0.50), respectively. Paired t test revealed statistically significant increases in IBDQ scores in both groups (mean increase in the EcN group, 22 points, p < 0.001; mean increase in the placebo group, 19 points, p < 0.001).
However, when considering decreases in the IBDQ score (i.e., reductions by > 16 points), a significantly lower number of patients in the EcN group exhibited decreased IBDQ scores than that of patients in the placebo group (1 [1.7%] vs. 8 [13.3%]; PP, p = 0.03; ITT, p = 0.02).
Secondary endpoints
At week 4, a significantly higher number of patients in the EcN group presented a decreased partial Mayo score, by two or more points from the baseline, than that of patients in the placebo group (23 [39.7%] vs. 13 [21.7%], p = 0.04) (Table 3). At week 8, no differences in clinical remission and clinical response rates were detected between the two groups. When SF and AP from Mayo score were compared separately, two groups showed no differences in terms of SF improvement (i.e., score = 0 or decreasing by more than one point) at 4 and 8 weeks. However, a significantly higher number of patients in the EcN group reported AP improvement (i.e., score = 0 or decreasing by more than one point) than that of patients in the placebo group at 4 weeks (91.4% vs. 61.7%, p < 0.001) and 8 weeks (86.2% vs. 66.7%, p < 0.001). In addition, a significantly higher number of patients in the EcN group exhibited endoscopic remission than that of patients in the placebo group (26 [46.4%] vs. 16 [27.1%], p = 0.03).
Following microbiome analysis, no statistically significant differences in α-diversity were observed between stool samples from the placebo and EcN groups, either at the baseline or at week 8 (Supplementary Fig. 1). For either group, principal component analysis (PCoA) of β-diversity did not reveal any distinct clustering patterns at the baseline or at week 8 (Supplementary Fig. 2). Individual differences (i.e., differences in the same patient before, during, and after the study) in microbial profiles between the baseline and week 8 were less pronounced than differences between individuals (i.e., differences between each pair of patients before, during, after the study), regardless of the treatment regimen (EcN or placebo) or clinical outcome (no response or response, in terms of either clinical remission or response at 8 weeks) (Supplementary Fig. 3). No significant difference was observed in the abundance of the Escherichia and Shigella genera, the first of which includes EcN, even in the group of patients exhibiting clinical response following EcN treatment (Supplementary Fig. 4).
Safety and tolerability
Adverse events were reported in 18 (26.9%) patients in the EcN group and 14 (21.2%) patients in the placebo group (p = 0.54). No major adverse events were observed. Several adverse events reflected common symptoms of active UC, such as bloody stools, diarrhoea, and AP, recorded in 14 (14.9%) and eight (12.1%) patients in the EcN and placebo groups, respectively (p = 0.80). Overall, seven patients receiving EcN (10.4%) reported other mild side effects, with one patient experiencing more than one symptom: two patients reported abdominal discomfort, two headache, one flu-like syndrome, one nausea, one epigastric pain, one chest discomfort, and one dizziness. In the placebo group, six patients (9.1%) reported mild side effects, with three patients reporting more than one symptom: three patients reported flu-like syndrome, two abdominal discomfort, two headache, one nausea, and one constipation. One patient from the EcN group with flu-like symptoms and one patient from the placebo group with constipation symptoms withdrew from the study during follow-up because of their symptoms.
Compliance
Among the 118 patients who completed the study, the mean number of days in which medication was taken was 55 ± 4.2. The adherence rate was 97% in the EcN group (n = 58) and 98% in the placebo group (n = 60; P = 0.22).
DISCUSSION
The present RCT was undertaken to evaluate the efficacy of EcN as an add-on treatment to conventional 5-ASA-based therapies for UC. Our findings revealed that EcN was not superior to the placebo in increasing the IBDQ scores of patients with mild-to-moderate UC. However, a significantly lower number of patients in the EcN group exhibited a decreased IBDQ score than that of patients in the placebo group. In addition, a significantly higher number of patients in the EcN group showed clinical response at week 4 and endoscopic remission at week 8 than that of patients in the placebo group.
Reportedly, the probiotic EcN can maintain remission in patients with UC, demonstrating effects equivalent to those of mesalazine [9]. In terms of remission induction, only one study in the literature compared the effect of EcN enemas with that of a placebo; in two other studies, a standard-of-care regimen with mesalazine or ciprofloxacin was applied [14,15]. In this study, we compared the efficacy of orally administered EcN with that of a placebo. However, an increase in IBDQ scores, rather than remission, was considered the primary endpoint, since the aforementioned previous three studies have reported varying results for the latter parameter. In particular, Rembacken et al. [15] compared the effect of oral EcN with that of mesalamine and found no significant difference in remission rates between the two groups (68% vs. 75%, p = 0.058). Nevertheless, both groups benefited from concomitant therapies, including steroid treatment, which were possibly more efficacious in resolving inflammation than EcN and mesalamine. Moreover, Matthes et al. [16] compared the efficacy of EcN enema with that of a placebo. These authors reported a higher dose-dependent remission rate in the EcN group after PP analysis (p = 0.046); however, this result was not confirmed by ITT analysis. Another study compared the effects of EcN, ciprofloxacin, and a placebo [14]. Unexpectedly, it was found that significantly fewer patients treated with EcN achieved remission than those who received the placebo (54% vs. 89%, p < 0.05). Therefore, currently available data on remission are inadequate to predict remission rates in patients treated with EcN when compared with those of patients treated with placebo, as well as to calculate the sample size required for the present study. Thus, the primary endpoint was established as an increase in IBDQ scores. Herein, we hypothesised that EcN treatment would trigger a more significant increase in IBDQ scores compared with that triggered by the placebo, based on a review that summarized the effect of biological interventions for UC treatment on HRQoL [11].
Various studies on IBD have reported that increases in the IBDQ score of 15 and 32 points from the baseline constitute the lower and upper boundaries, respectively, of clinically meaningful improvements in HRQoL [11]. In the present study, IBDQ scores were significantly increased in the EcN group, by a mean of 22 points. However, no difference was observed in the percentage of patients displaying increased IBDQ scores when compared with that of the placebo group. Interestingly, when comparing the rates of decrease in IBDQ scores between the two groups, a significantly lower number of patients in the EcN group showed decreasing IBDQ scores than that of patients in the placebo group. Among previous studies that investigated the efficacy of probiotics in improving IBDQ scores in patients with UC, Fujimori et al. [17] reported increasing IBDQ scores after 4 weeks in all test groups, including a probiotic group (treated with Bifidobacterium longum), a prebiotic group (treated with psyllium), and a symbiotic group (treated with both B. longum and psyllium); however, a statistically significant difference over time was observed only in the symbiotic group (probiotic group, 162 to 169, non-significant; prebiotic group, 174 to 182, non-significant; symbiotic group, 168 to 176, p = 0.03). These results suggest that probiotics alone might not be sufficient to improve HRQoL in UC patients but may still be effective in preventing UC exacerbation.
Regarding UC activity, a significantly higher number of patients in the EcN group exhibited clinical response at 4 weeks (39.7%) and endoscopic remission at 8 weeks (46.4%) than that of patients in the placebo group. These results are consistent with the findings of Matthes et al. [16], who assessed the effects EcN enema administration and found that 47.6%, 38.9%, and 45.5% of the patients receiving 40, 20, and 10 mL of EcN, respectively, showed remission or improved histological scores. These results indicate that both orally administered EcN and EcN enemas are effective in inducing remission in UC, especially in terms of endoscopic activity.
In a previous RCT examining the use of Clostridium butyricum to treat UC patients with ileal pouch anal anastomosis [18], the abundance of Clostridium coccoides tended to increase after therapy in the placebo group, while that of Enterococcus spp. tended to decrease after therapy in both groups. Moreover, the abundance of bacteria of the Escherichia genus was significantly decreased in the probiotics group after therapy compared with that before therapy. In another study, a case-control investigation was conducted, and all the individuals included in the probiotics group consumed probiotics containing B. longum, Lactobacillus acidophilus, and Enterococcus faecalis [19]. Microbial diversity analysis revealed that the number of operational taxonomic units, as well as the abundance-based coverage estimator and Chao indices, were higher in the short-term treatment group compared with those in the long-term treatment group. However, the two groups displayed no differences in terms of Shannon and Simpson indices. This study demonstrated that long-term intake of probiotics caused significant changes in the structure of the gut microbiota, including an increased proportion of beneficial microorganisms. Based on these findings, we hypothesized that EcN administration might alter the structure of the gut microbiota, including its diversity; however, this was not found to be the case. It is well known that the stool microbiota can be affected by food and lifestyle; therefore, our lack of findings may be attributed to our inability to control for these important variables.
The strength of our study lies in the fact that this is the first RCT to evaluate the efficacy of orally administered EcN when compared with that of a placebo. In addition, we evaluated the efficacy of EcN as an add-on treatment to conventional 5-ASA therapies. Previous RCTs have confirmed the efficacy of other drugs when compared with that of conventional 5-ASA therapy. Since drugs such as probiotics or immunomodulators are commonly combined with 5-ASA to treat mild-to-moderate UC in clinical settings, data on the efficacy of EcN as an add-on treatment may be critical. Finally, in contrast to three previous studies [14–16] that investigated the efficacy of EcN in inducing UC remission, we avoided any combination with other potent medications, such as steroids and immunomodulators, to induce remission in patients with UC. Therefore, the observed prevention of IBDQ score decrease and improved UC activity can be directly attributed to the effect of EcN.
However, a few limitations of the present study must be acknowledged. First, since an increase in the IBDQ score was set as the primary endpoint due to lack of previous data, the clinical efficacy of EcN in terms of the secondary endpoints of the present study need to be further confirmed. Secondly, the stool microbial communities of the two groups did not differ, and we did not identify species whose abundance responded specifically to EcN as 16S rRNA amplicon sequencing limited our evaluation to the species level; therefore, in future studies, we aim to perform additional experiments using methods such as shotgun sequencing or EcN-specific polymerase chain reaction.
In conclusion, our study showed that EcN treatment was not more efficient than the placebo in promoting increased IBDQ scores, that is, the primary endpoint. Nevertheless, EcN was found to be safe and effective in preventing the worsening of IBDQ scores and achieving clinical responses and endoscopic remission in patients with mild-to-moderate active UC.
KEY MESSAGE
1. This is the first randomised clinical trial to evaluate the efficacy of orally administered Escherichia coli Nissle 1917 (EcN) compared with that of a placebo. A significantly lower number of patients in the EcN group exhibited decreased inflammatory bowel disease questionnaire (IBDQ) scores than that of patients in the placebo group.
2. A significantly higher number of patients in the EcN group showed clinical response at week 4 and endoscopic remission at week 8 than that of patients in the placebo group.
SUPPLEMENTARY METHODS
DNA extraction and bacterial 16S rRNA gene sequencing
DNA from stool samples was extracted within 1 month after storage using the Stool DNA Isolation Kit (#27600, Norgen Biotek Corp., Thorold, ON, Canada) according to the manufacturer’s instructions.
The V3–V4 region of the 16S rRNA gene was amplified using 341F and 805R primers with the Illumina adaptor overhang sequences, 341F (5-‘TCG TCG GCA GCG TCA GAT GTG TAT AAG AGA CAG CCT ACG GGN GGC WGC AG 3’) and 805R (5’ GTC TCG TGG GCT CGG AGA TGT GTA TAA GAG ACA GGA CTA CHV GGG TAT CTA ATC C 3’). Amplicons were purified using a magnetic bead-based clean-up system (Agencourt AMPure XP, Beckman Coulter, Brea, CA, USA). Indexed libraries were prepared by limited-cycle polymerase chain reaction using Nextera technology, further cleaned up, and pooled at equimolar concentrations. The final library was denatured with 0.2 N NaOH and diluted to 6 pM with a 20% PhiX control.
Sequencing and demultiplexing were performed using the Illumina MiSeq platform by employing a 2 × 300 bp paired-end protocol, according to the manufacturer’s instructions. The Mothur software version 1.44.3 (https://mothur.org/) was used to process the microbiome data according to the MiSeq SOP (https://mothur.org). Briefly, the paired-end reads were assembled into 31,904,045 contigs, which were then aligned to the V3–V4 region of the Silva bacterial reference multiple sequence alignment (Release 102). After removing low-quality sequences and filtering chimeras, the 20,554,921 resulting sequences were taxonomically classified with Wang’s method with the default options (kmer size = 8, bootstrap cut-off = 80%, and number of iterations = 100) using RDP reference sequences and taxonomic assignments (version 16). The sequences were classified at the genus level as recommended for the Ribosomal Database Project (RDP) reference, resulting in 503 phylotypes. The corresponding abundance table revealed that Bacteroides, Faecalibacterium, and Prevotella were the most abundant, with 315 phylotypes observed more than 10 times.
Statistical assessment
For stool microbiome analysis, the abundance table of phylotypes at the genus level was used for calculating α- and β-diversities using Mothur version 1.44.3. Next, to account for variable sequencing depth among samples, the phylotypes of each sample were subsampled using the smallest sample size (32,650). The subsampling was repeated 1,000 times, and the resulting coefficients were averaged for each sample. The α-diversity was measured using the Shannon coefficient, and the β-diversity was estimated using Bray-Curtis dissimilarities and Yue and Clayton θ distances. For the β-diversity, principal coordinate analysis was calculated with Mothur, while all other statistical analyses, including MA plots of rank values for a given genus, were performed with R version 4.1.0 (R Foundation for Statistical Computing, Vienna, Austria). For MA plots, the phylotype abundance values were replaced by ranks in each sample. Accordingly, the M value is the difference between ranks after and before treatment with either Escherichia coli Nissle 1917 (EcN) or placebo, while the A value is the average of ranks after and before treatment. In the MA plot, A and M values are plotted on the x and y axes, respectively.
Acknowledgments
We acknowledge the support provided by the computing resources of the Global Science experimental Data hub Center (GSDC) Project and the Korea Research Environment Open NETwork (KREONET) of the Korea Institute of Science and Technology Information (KISTI).
Notes
This study was supported by a research grant from BL&H Co., Ltd.