Impact of urgently initiated tele-prescription due to COVID-19 on glycemic control in patients with type 2 diabetes
Article information
Abstract
Background/Aims
Coronavirus disease 2019 (COVID-19) is a global pandemic that had affected more than 13,000 people in South Korea by July 2020. To prevent spread of COVID-19, tele-prescription was permitted temporarily. This study investigated the impact of tele-prescription on glycemic control in patients with type 2 diabetes.
Methods
Glycated hemoglobin (HbA1c) concentrations were retrospectively analyzed in patients with type 2 diabetes who were treated with tele-prescription because of COVID-19 and those who were treated by face-to-face care (non-tele-prescription group) enrolled at the same period of time. Mean HbA1c concentrations and mean change in HbA1c concentration (ΔHbA1c) were compared in these two groups.
Results
The mean HbA1c levels of patients were significantly higher after than before the tele-prescription period (7.46% ± 1.24% vs. 7.27% ± 1.13%, p < 0.05). Mean ΔHbA1c was significantly higher in the tele-prescription than in the non-tele-prescription group (0.19% ± 0.68% vs. 0.04% ± 0.95%, p < 0.05). HbA1c was significantly greater in patients taking fewer oral hypoglycemic agents, no insulin, fewer comorbidities (e.g., coronary artery disease, cerebrovascular accident, and diabetic neuropathy), and higher baseline HbA1c.
Conclusions
Tele-prescription may worsen glycemic control in patients with type 2 diabetes during public health crises.
INTRODUCTION
Since the onset in December 2019 of coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), this disease has spread rapidly to over 160 countries worldwide [1]. As of July 10, 2020, there were more than 13,000 confirmed cases and about 280 COVID-19-related deaths in South Korea [2]. Chronic diseases such as diabetes have been identified as important risk factors for severe illness and death from COVID-19 [3,4]. One meta-analysis showed that mortality rates in patients with confirmed COVID-19 were about 2-fold higher in patients with than without diabetes [5]. Therefore, to reduce mortality from COVID-19, it is important to prevent patients with diabetes from contracting this disease.
The rapid spread of COVID-19 in South Korea led to the unprecedented implementation of strict social distancing. Due to the limitation of face-to-face visits in clinics, telemedicine with remote prescriptions was permitted temporarily, beginning on February 24, 2020 [2]. Originally, telemedicine was developed to provide accessible, cost-effective, high-quality health care services to patients in remote locations using telecommunication technology [6]. It uses electronic communications, advanced computing, and telematics technology to exchange medical information [7]. Telemedicine had already shown its usefulness in disasters and public health crises [8,9], and is expected to reduce the likelihood of COVID-19 infection by avoiding face-to-face contact during the COVID-19 pandemic.
The potential benefit of telemedicine for managing diabetes has been advocated since the early 1980s. Some studies actively involved in blood sugar control using a self-reporting system show that telemedicine can be a good strategy for the treatment of patients with diabetes [10,11]. However, rigorous telemedicine was not ready to start in the current medical environment; therefore, it was started temporally with tele-prescriptions, a form of telephone consultation and remote prescription. Although telemedicine is applicable during disasters and public health crises [8,9], the effects of urgently initiated tele-prescription strategies on glycemic control in patients with type 2 diabetes during public health crises are not clear.
Therefore, the present study investigated whether glycated hemoglobin (HbA1c) concentrations differ between patients with type 2 diabetes treated by tele-prescription and those treated by face-to-face care.
METHODS
Study design and participants
This retrospective, case-control study included patients with type 2 diabetes aged > 20 years who visited two tertiary hospitals, Kyungpook National University Hospital (KNUH) and Kyungpook National University Chilgok Hospital (KNUCH), in Daegu, South Korea. The study protocol was approved by the Institutional Review Boards of KNUH and KNUCH (IRB numbers 2020-07-020 and 2020-05-021, respectively). The ethics boards of the two hospitals waived the requirement for informed consent because of the retrospective study design.
Tele-prescription was conducted entirely at the request of the patient, who received a remote prescription after telephone counseling. The process of tele-prescription included self-monitoring of blood glucose and counseling for insulin dose titration or diet control; therefore, the time required for tele-prescription was almost the same as that for face-to-face care. The number of tele-prescriptions implemented during the entire study period was limited to one. For patients with diabetes, who need immediate blood sugar control through strong interventions (e.g., first insulin start, hyperglycemic crisis, and hypoglycemia), face-to-face care was recommended. However, patients who did not require strong intervention and were already using insulin were managed via tele-prescription. The flow chart of the study design is presented in Fig. 1. The study periods were defined according to the introduction of tele-prescription relative to the COVID-19 outbreak in Daegu. The tele-prescription period was defined as 2 months after tele-prescription was first introduced (February 26 to April 25, 2020). Period 1 (August 26, 2019 to February 25, 2020) was defined as 6 months before the start of tele-prescription and Period 2 as 4 months after the introduction of tele-prescription. HbA1c was measured during Period 1 and again during Period 2. HbA1c results for Period 1 and Period 2 were selected as values; these were measured only once each within 1 to 6 months before and after the tele-prescription period. The control group was selected during the same period using the same method.
A total of 1,000 patients were treated by tele-prescription at the two hospitals (733 at KNUH and 267 at KNUCH) during the defined tele-prescription period, which is equivalent to 14.17% and 16.88%, respectively, of all outpatients of the department of ‘Endocrinology and metabolism’. Among these, 539 patients, 419 at KNUH and 120 at KNUCH, were treated for diabetes. Of these 539 patients, 236 were excluded, including (1) patients who were not followed-up during Period 2 (127 at KNUH, 48 at KNUCH); (2) patients who changed oral hypoglycemic agents (OHA) or insulin during Period 1 (27 at KNUH, 10 at KNUCH); (3) patients diagnosed with diabetes < 1 year before Period 1 (none at KNUH, two at KNUCH); (4) patients hospitalized < 1 year before Period 1 (eight at KNUH, two at KNUCH); (5) patients diagnosed with type 1 diabetes (two at KNUH, none at KNUCH); and (6) patients being treated for serious illnesses, including those receiving chemotherapy (four at KNUH, six at KNUCH). The case group, therefore, consisted of 303 patients.
During the same period of time, 2,852 patients (2,316 at KNUH and 536 at KNUCH) with diabetes were treated by face-to-face care. Among these, 1,821 patients (1,405 at KNUH and 416 at KNUCH) measured baseline HbA1c levels during Period 1. To effectively control for confounding factors, such as age, gender, and baseline HbA1c, 1:1 propensity score matching was performed to select 302 patients as the control group according to the same inclusion and exclusion criteria.
Statistical analysis
All statistical analyses were performed using SPSS version 26.0 software (IBM Inc., Armonk, NY, USA). Paired t tests were used to compare mean HbA1c levels within each group during Periods 1 and 2. Independent t tests were used to compare differences in ΔHbA1c level in the two groups between Periods 1 and 2. A p < 0.05 was considered statistically significant.
RESULTS
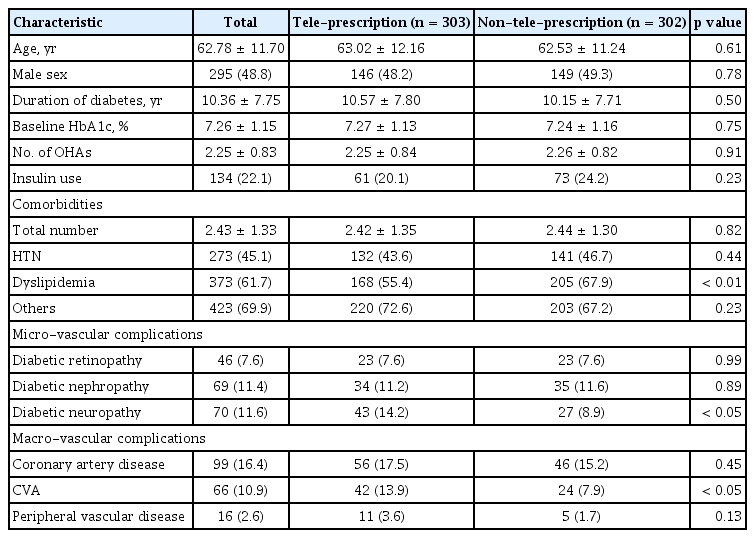
Baseline characteristics of patients with type 2 diabetes in the tele-prescription and non-tele-prescription groups
The characteristics of the patients enrolled in this study and of all patients with diabetes are presented in Table 1 and Supplementary Table 1, respectively. The mean age of all participants was 62.78 ± 11.70 years, the mean duration of diabetes was 10.36 ± 7.75 years, the mean baseline HbA1c was 7.26% ± 1.15%, the mean number of OHA per patient was 2.25 ± 0.83, and the mean number of comorbidities per patient was 2.43 ± 1.33. Of the total participants, 134 (22.1%) patients were taking insulin, 273 (45.1%) were taking anti-hypertensive drugs, and 373 (61.7%) were taking lipid-lowering drugs. There were no between-group differences in patient age, gender, duration of diabetes, baseline HbA1c concentration, number of OHAs, insulin use, and number of comorbidities. However, there were significant differences between the groups regarding diabetic neuropathy and cerebrovascular accident (CVA).
Mean HbA1c and ΔHbA1c of patients with type 2 diabetes in the tele-prescription and non-tele-prescription groups
In the tele-prescription group, the mean HbA1c levels were significantly higher during Period 2 than Period 1 (7.46% ± 1.24% vs. 7.27% ± 1.13%, p < 0.05) (Fig. 2). By contrast, mean HbA1c levels were similar during Periods 1 and 2 in the non-tele-prescription group (7.24% ± 1.16% vs. 7.28% ± 1.24%, p = 0.48). Regarding the difference in HbA1c between Periods 1 and 2, ΔHbA1c was significantly greater in the tele-prescription than in the non-tele-prescription group (0.19% ± 0.68% vs. 0.04% ± 0.95%, p < 0.05) (Fig. 3).
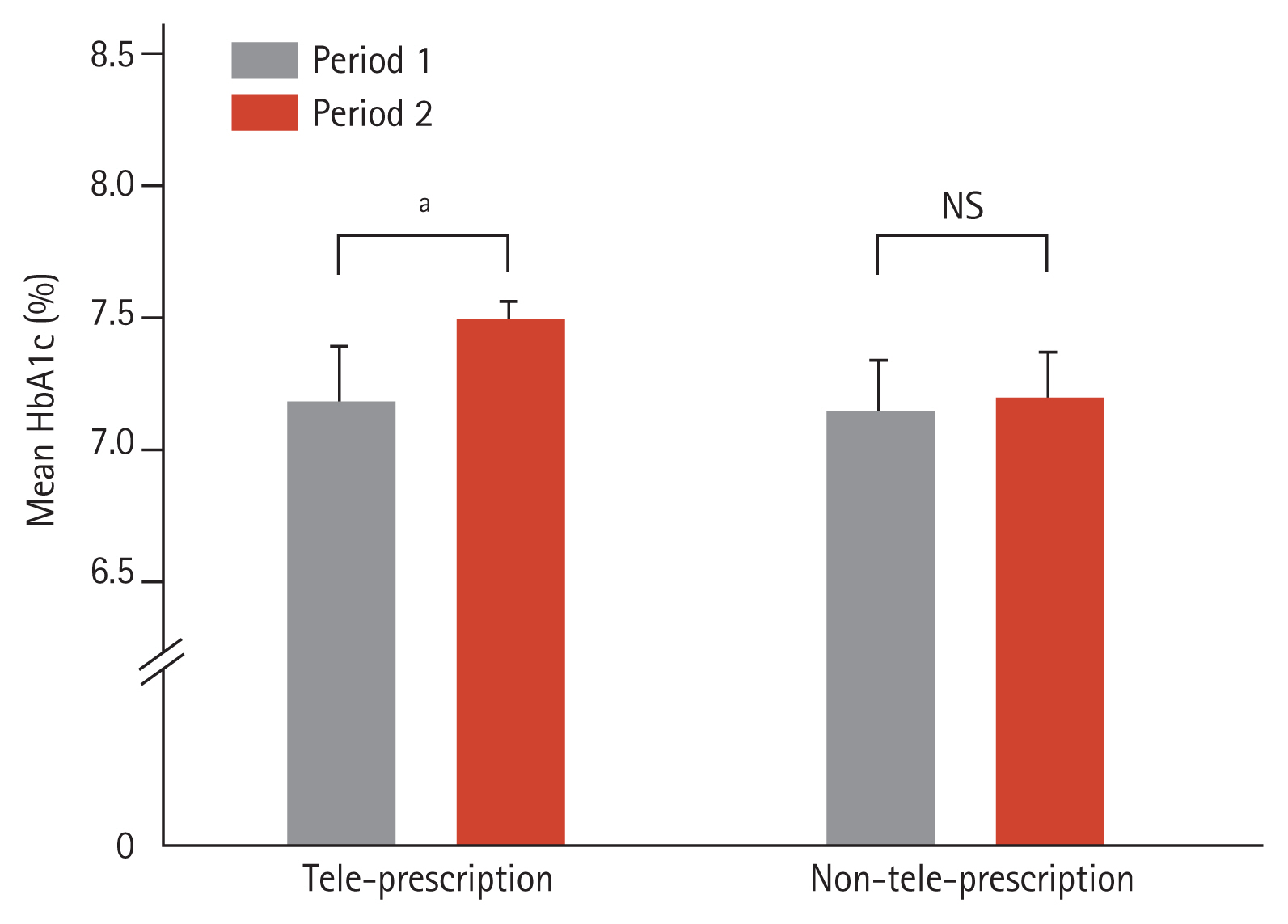
Mean glycated hemoglobin (HbA1c) of patients with diabetes in the tele-prescription and non-tele-prescription groups. Tele-prescription group: 7.27% ± 1.13% (Period 1), 7.46% ± 1.24% (Period 2); non-tele-prescription group: 7.24% ± 1.16% (Period 1), 7.28% ± 1.24% (Period 2). Results are reported as the mean ± standard deviation HbA1c concentration. Data were analyzed using a paired t test. NS, not significant. ap < 0.05.

Glycated hemoglobin concentration (ΔHbA1c) of patients with diabetes in the tele-prescription and non-tele-prescription groups. Tele-prescription group: 0.19 ± 0.68; non-tele-prescription group: 0.04 ± 0.95. Results are reported as the mean ± standard deviation ΔHbA1c concentration. Data were analyzed using an independent t test. ap < 0.05.
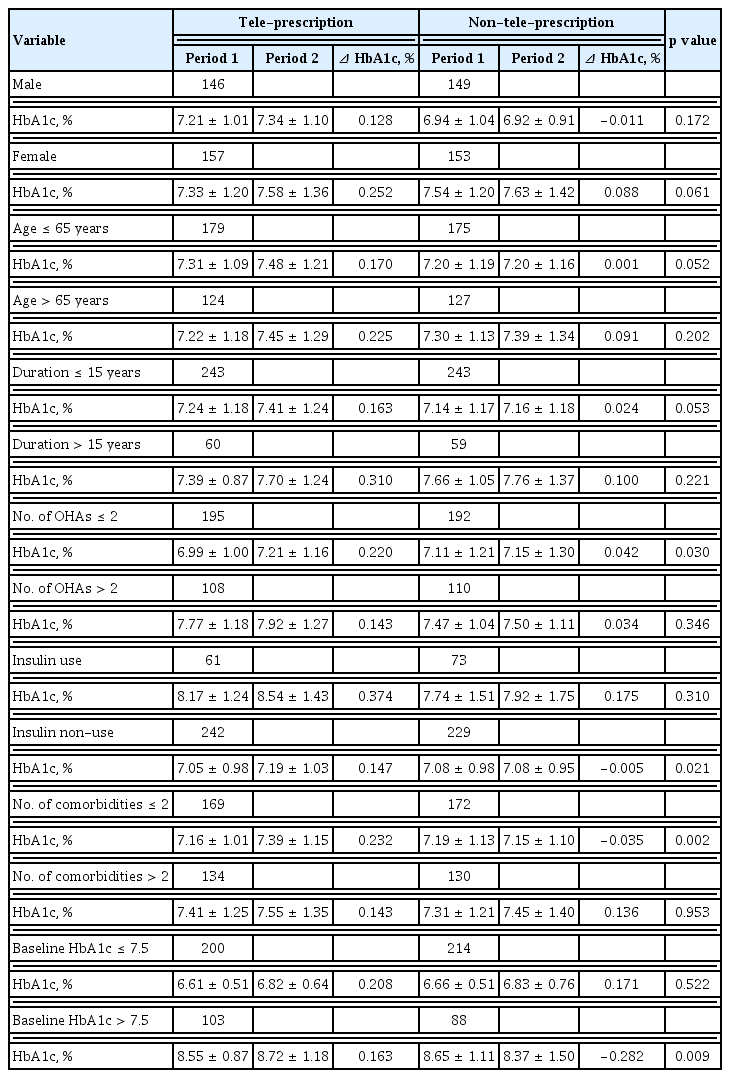
Subgroup analysis of delta glycated hemoglobin in the tele-prescription and non-tele-prescription groups
Subgroup analysis was performed to assess the relationships of ΔHbA1c with gender, age, duration of diabetes, number of OHAs, insulin use, number of comorbidities, and baseline HbA1c in the two groups (Table 2). The HbA1c in participants with fewer OHAs (≤ 2), non-insulin users, fewer comorbidities (≤ 2), and higher baseline HbA1c (> 7.5%) was significantly higher after than before the introduction of tele-prescription (p < 0.05). In addition, HbA1c was significantly higher after than before tele-prescription in patients without coronary artery disease, CVA, and diabetic neuropathy (p < 0.05) (Supplementary Table 2).
DISCUSSION
The results of this study demonstrated that urgently initiated tele-prescription did not show a better effect on glycemic control in patients with type 2 diabetes during the COVID-19 outbreak than face-to-face care. Mean HbA1c concentration showed a greater increase in patients after introduction of tele-prescription than in those treated by face-to-face care. ΔHbA1c in the tele-prescription group was especially higher in patients with fewer OHA medications, no insulin, fewer comorbidities, and higher baseline HbA1c.
Social distancing, introduced after the start of the COVID-19 pandemic, has resulted in many changes to the medical environment. The need for telemedicine has been emphasized, with several countries, including China [12], Singapore [13], and Australia [14], implementing telemedicine programs. Some studies demonstrate the benefits of telemedicine in patients with diabetes. A meta-analysis of 35 randomized controlled trials of telemedicine using video, phone, and e-mail showed a reduction in HbA1c of −0.37% (p < 0.001) in the telemedicine group compared with controls [15]. A recent study that included patients with type 1 and 2 diabetes showed an overall mean reduction in HbA1c in the telemedicine groups with type 1 (−0.12% to −0.86%) and type 2 (−0.01% to −1.13%) diabetes [16]. Although many advantages of telemedicine are known [17,18], it was difficult to implement proper telemedicine protocols in this study due to limited availability of medical technology and devices. We found that the mean HbA1c level increased significantly after introduction of tele-prescription, but was unaltered in the non-tele-prescription group. Furthermore, ΔHbA1c was significantly greater in the tele-prescription than in the non-tele-prescription group.
Subgroup analysis showed that HbA1c after tele-prescription care was significantly higher in patients with fewer OHA medications, and comorbidities. In addition, tele-prescription care was associated with a higher ΔHbA1c in patients not taking insulin, which may be explained, at least in part, by their inability to adjust their medications according to glucose levels (unlike insulin users). Furthermore, ΔHbA1c was higher in patients with baseline HbA1c > 7.5% than in those with baseline levels ≤ 7.5%, suggesting that tele-prescription may be deleterious in patients who require immediate and active strategies for glucose control. Interestingly, especially in patients without comorbidities such as coronary artery disease, CVA, and diabetic neuropathy, HbA1c was significantly higher after than before the tele-prescription period. It is assumed that the changes in lifestyle interventions may have had an impact on glucose control these groups due to the COVID-19 pandemic, but further research is required to prove a causal relationship. These findings suggest that if remote diagnosis is not conducted, glycemic control may worsen; thus tele-prescription should be used carefully, especially for patients with relatively lesser comorbidities during the public health crisis.
Since this is a retrospective study, it has several limitations. First, the baseline characteristics of the patient group, such as height and weight, were not investigated, and relatively different HbA1c values (depending on gender) may introduce selection bias that affects the results in subgroup analysis. Second, the glucose control was assessed only by measuring HbA1c levels; we did not take into account additional factors such as physical activity, diet, or adherence to medication, which could affect glycemic control. Third, patients who request telephone prescriptions are more likely to show relatively low compliance with treatment; however, this variable was not reflected in our study. Fourth, the observation period was too short to fully assess the impact of tele-prescription care on glucose control. To overcome this limitation, a preemptive and well-organized system is required. Objective indicators of diet, physical activity, and drug compliance, which are factors that can affect blood sugar control, should be identified. Finally, a discussion about how to implement this for patients who need appropriate intervention through remote counseling is needed.
Despite these limitations, our study has generated meaningful findings. To the best of our knowledge, this report is the first to show the impact of tele-prescription on glycemic control in patients with type 2 diabetes during the COVID-19 pandemic. These findings suggest that care should be exercised when introducing a tele-prescription strategy for treatment of diabetes during a public health crisis, especially for patients with relatively well controlled blood sugar. In addition, such strategies should be accompanied by appropriate intervention and remote diagnosis, which includes self-monitoring of glucose. Additional studies are needed to determine the impact of telemedicine on clinical outcomes during acute health crises.
KEY MESSAGE
1. Tele-prescription, which was urgently initiated during the coronavirus disease 2019 (COVID-19) outbreak, did not show a better effect on glycemic control in patients with diabetes than face-to face care.
2. In particular, the following patients with diabetes need more careful monitoring during urgently initiated tele-prescription: less oral hypoglycemic agent (≤ 2), non-insulin users, fewer comorbidities (≤ 2), and higher baseline glycated hemoglobin (> 7.5%).
3. During a public health crisis, tele-prescription is expected to provide many benefits for patients with diabetes, but this should be accompanied by a well-organized system and remote diagnosis.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This work was supported by a Biomedical Research Institute grant, Kyungpook National University Hospital (2020).
We thank all the patients for participating in this study.