What should we prepare for the next coronavirus disease 2019 outbreak? A survey on the opinions of infectious diseases specialists in South Korea
Article information
Abstract
Background/Aims
This study aimed to collect information on the opinions of Korean infectious disease (ID) experts on coronavirus disease 2019 (COVID-19) and related issues in preparation for a future outbreak.
Methods
A survey was conducted over the course of 5 days (from April 21 to 25, 2020), targeting all adult ID specialists currently in the medical field in South Korea (n = 265). An online-based survey was forwarded via text message and e-mail. Only one response was accepted from each participant.
Results
Of these 265 ID specialists gotten to, 132 (49.8%) responded. The highest proportion of the respondents envisaged the current COVID-19 outbreak to end after December 2020 (47.7% for the domestic Korean outbreak and 70.5% for the global pandemic); moreover, 60.7% of them stated that a second nationwide wave is likely to occur between September and December 2020 in South Korea. N95 respirators were considered to be the most important item in hospitals in preparation for a second wave. The most important policy to be implemented at the national level was securing national hospitals designated for the treatment of ID (67.4%).
Conclusions
ID experts in South Korea believe that the COVID-19 pandemic may not be easily controlled and that a second nationwide wave is likely to occur in South Korea. Our results indicate that Korean ID specialists believe that a high level of preparation is needed in various aspects, including the procurement of personal protective equipment, to respond efficiently to a second outbreak.
INTRODUCTION
The coronavirus disease 2019 (COVID-19) has spread rapidly across the globe since late 2019, resulting in the onset of a pandemic on March 11, 2020. As a result, more than 4 million confirmed cases of COVID-19 have been reported, encompassing more than 210 countries as of the end of April, 2020 [1]. The first confirmed patient, a Chinese national, entered the country from Wuhan, China on January 19, 2020 [2], and South Korea became one of the first countries to be affected by the outbreak, with a total of 10 738 infections as of April 27, 2020 [3]. The highest level of infectious disease (ID) alert was declared after the occurrence of a significant outbreak within a religious group in Daegu and its neighboring areas in mid-February 2020 [4], after which several countermeasures were introduced and reinforced. Consequently, the outbreak was mitigated from mid-April, with only around 10 newly confirmed cases per day [3]. Thus, South Korea is revisiting the measures put in place during the worst period of the outbreak, namely social distancing, and is preparing for a return to normal life.
Despite the positive social atmosphere, many experts have been warning of a possible second wave. Considering the characteristics of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is reported to be shed from infected patients at the early phase of the COVID-19 and can be transmitted from asymptomatic patients or patients with vague symptoms, it is prospected hard to be controlled [5-7]. Therefore, a discussion on the preparation for the next COVID-19 outbreak might be necessary in order to protect the social system from collapse.
This study aimed to collect information on the opinions of ID experts on COVID-19 and related issues in preparation for a potential second wave of infections.
METHODS
A questionnaire was designed by three investigators (B.K., S.Y.P., and H.H.C.) based on the ‘COVID-19 Real-Time Barometer Study’ and modified to reflect the current unsolved issues associated with COVID-19 [8]. The other authors of this study reviewed the draft questionnaire, and it was refined on the SurveyMonkey platform (Supplementary material 1). The questions about the opinions on COVD-19-related issues consisted of four categories: (1) prospects of the COVID-19 outbreak, (2) preparation for a future COVID-19 outbreak, (3) therapeutic options for COVID-19, and (4) miscellaneous. Some questions required the respondent to select multiple answers. The survey was conducted over a period of 5 days (from April 21 to 25) in 2020, and targeted all physicians with a board certificate of adult ID in South Korea (n = 275). At the time of the survey, 10 experts were either retired or had passed away and were excluded accordingly. Eventually, 265 ID specialists were identified as the subjects of the survey. A link to the online-based survey was forwarded to the subjects via text message and e-mail. To encourage participation, reminders were sent on the 3rd, 4th, and 5th day. There was no reward for the completion of the questionnaire. The respondents were anonymized and were requested to enter their own identification number in order to distinguish duplicated answers. Only one response was accepted from each participant.
In addition to the main analysis, we performed a subgroup analysis for the opinions on the preparation for future COVID-19 outbreak as per the attending physician’s experience in treating COVID-19 patients. The confidence interval for differences of binomial proportions was measured using the Agrestic-Caffo method.
All statistical analyses were performed using SPSS version 24.0 for Windows (IBM Corp., Armonk, NY, USA). Categorical variables were analyzed using the chi-square test or Fisher’s exact test, as appropriate. A two-tailed p value of < 0.05 was considered statistically significant.
The Institutional Review Board of the Hanyang University Seoul Hospital approved the study protocol (IRB number: 2020-04-039). Online-written informed consent was obtained from participants.
RESULTS
Demographic characteristics of respondents
Among the 265 ID specialists, 132 (49.8%) responded. The mean age of the respondents was 42.8 ± 6.6 years, with an average of 8.9 ± 6.0 years elapse since they had acquired their ID board certificates and 57.6% were female. Almost all the respondents (99.3%) were working at secondary-care or tertiary-care hospitals; the majority (75.8%) were working at a national or private university-affiliated hospital. The proportion of respondents who had treated COVID-19 patients as an attending physician was 68.2% (Table 1).
Opinions of ID specialists on COVID-19 related issues
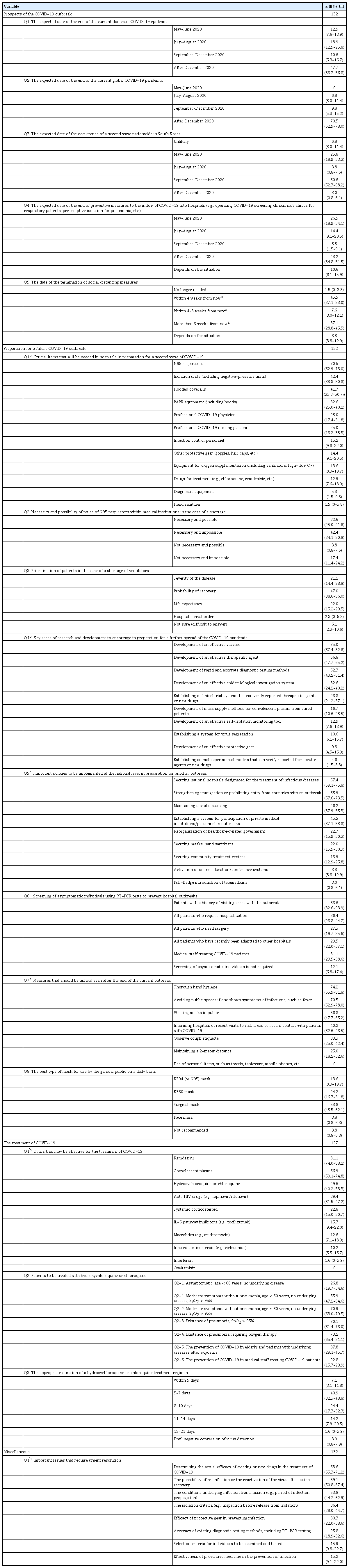
Table 2 shows the results of our survey. Most respondents stated that they envisaged the current COVID-19 outbreak to end after December 2020 (47.7% for the domestic outbreak and 70.5% for the global pandemic), as well as a second nationwide wave in South Korea between September and December 2020 (60.7%). Accordingly, the majority believed that the current preventive strategies being implemented in Korean hospitals need to be maintained even after December 2020 (43.2%).
N95 respirators were considered to be the most important item for hospitals in preparation for a second wave, followed by isolation units and hooded coveralls. Furthermore, 75.0% of the respondents believed that the reuse of N95 respirators might be necessary in the case of a shortage. In the case of a shortage of ventilators, 47.0% believed that patients should be prioritized based on the likelihood of their recovery. In preparation for another outbreak, the respondents believed that the most important areas of research and development to be fostered were the development of effective vaccines (75.0%), the development of effective therapeutic drugs (56.8%), and the development of rapid and accurate diagnostic testing methods (52.3%). The most important policies to be implemented at the national level included securing national hospitals designated for the treatment of ID (67.4%), strengthening immigration policies or prohibiting the entry of individuals from affected countries (65.9%), and maintaining social distancing (46.2%). Most of the respondents (88.6%), as concerns the screening of asymptomatic individuals for the prevention COVID-19 outbreaks in medical institution, answered that real-time reverse-transcriptase polymerase chain reaction testing would be necessary for patients with a recent history of visits to affected countries or regions, in order to prevent outbreaks occurring within hospitals. The respondents stated that the most important measures to be upheld by the general public after the end of the outbreak were thorough hand hygiene (74.2%), followed by avoiding public spaces if one has symptoms of COVID-19 (70.5%), and the wearing of masks in public (56.8%). The most recommended type of mask for use on a daily basis was the surgical mask (53.8%).
In terms of treatment options, the respondents reported that remdesivir was the most promising (81.8%) therapeutic agent for the treatment of COVID-19, followed by convalescent plasma (65.9%) and hydroxychloroquine or chloroquine (49.2%). The majority of respondents showed a preference towards the use of hydroxychloroquine or chloroquine regimens in the elderly or in severe cases, while prophylactic use was not preferred.
The respondents stated that issues requiring urgent attention and resolution included “determining the actual efficacy of existing or new drugs for the treatment of COVID-19” (63.6%), “the possibility of re-infection or the reactivation of the virus after patient recovery” (59.1%), and “the conditions underlying the infection transmission” (53.8%).
The comparison in opinions on the preparation for another COVID-19 outbreak as per the attending physician’s experience in treating COVID-19 patients
Most ID specialists who had experience in treating COVID-19 patients answered that powered air purifying respirator equipment (44.4% vs. 7.1%) are important items for hospitals in preparation for a second wave compared with those who had no experience in treating COVID-19 patients (Supplementary Table 1).
DISCUSSION
This survey highlights the opinions of Korean ID experts on controversial COVID-19-related issues. The opinions of these experts regarding emerging IDs are especially valuable as: (1) their opinions are based on their direct experience; (2) a relatively long time is needed to obtain scientific evidence on diseases; and (3) their opinions provide a guide for improving public preparedness. Our results provide useful information in preparation for another potential future COVID-19 outbreak.
In contrast to the positive social atmosphere in South Korea, many ID specialists do not envisage the current outbreak to be controlled easily. Considering the high viral load at the initial phase of the disease, even in asymptomatic patients [6], the complete control of viral transmission remains a challenge. Once social interactions between individuals return to normal and international travel is reinstated, the possibility of a COVID-19 second wave in South Korea is likely to increase accordingly.
The N95 respirators were considered as the most important item to be procured in hospitals. Since SARS-CoV-2 is transmitted via the respiratory tract, health workers when caring for patients must use appropriate masks. In particular, the use of N95 respirators is an effective measure to protect healthcare personnel from the transmission of the virus during aerosol-generating procedures [9]. Unfortunately, hospitals experienced a lack of protective equipment in the middle of the outbreak, which is representative of the difficult experience of South Korea in dealing with the pandemic. In addition, experience might lead the majority of respondents to believe that the reuse of N95 respirators would be inevitable in the case of a shortage.
Many ID specialists believe that at the national level, securing hospitals designated specifically for the treatment of IDs is necessary. This may help to provide an effective therapy to COVID-19 patients, as well as protecting non-infectious patients admitted to other hospitals. Indeed, preventive measures against the inflow of COVID-19 into hospitals are fundamentally important since COVID-19 could be fatal when transmitted to in-patients [10]. Policymakers should consider this when establishing policies related to COVID-19.
The most important social measures to be upheld even after the end of the outbreak were hand hygiene and avoiding public places when a person has symptoms of infections. Given that the microorganisms are frequently transmitted via one’s hand to another or themselves, hand hygiene is considered to be the single most important measure in reducing the transmission of microorganisms [11]. Given the fact that the dissemination of SARS-CoV-2 cannot be prevented just by wearing a mask and the virus can remain viable and infectious on surfaces up to days, hand hygiene should be emphasized to prevent infection [12,13]. Furthermore, interestingly, due to the thorough adherence to measures for the prevention of microorganism transmission, we witnessed that the incidence of other notorious transmissible IDs such as chickenpox, influenza, epidemic conjunctivitis, etc., decreased significantly in 2020 compared to other years [14]. People need to understand that not only the individual’s health but also the health of the entire society could be protected with adherence to these measures.
As study results about the effectiveness of drugs tested for the treatment of COVID-19 have been released, opinions about the therapeutic option also have been converging accordingly. Since hydroxychloroquine or chloroquine was still one of the most promising therapeutic agents at the time of the survey period, we surveyed the opinion about the use of hydroxychloroquine or chloroquine in more detail. Unfortunately, the recent studies revealed that the use of hydroxychloroquine or chloroquine in COVID-19 might not be effective [15]. The only drug that showed effectiveness against COVID-19 to the date (June 5, 2020) is remdesivir. It shortened the time of recovery in patients with COVID-19 and evidence of lower respiratory tract infection but it did not lower the mortality [16].
This study had some potential limitations. First, the response rate was approximately 50% and those who were interested in such a study might tend to have responded to the survey. In order to minimize the selection bias, we sent reminders three times as well as offered the online link via both smartphones and computers to ease the access to the survey. Moreover, the demographic data of respondents (age 42.8 ± 6.6; female sex 57.6%) were similar to those of the entire target population (age 44.7 ± 6.7; female sex 50.6%) and the possibility of selection bias would not have been high. Second, some items might be interpreted differently by respondents due to the nature of the survey study.
In conclusion, many Korean ID experts believe that the COVID-19 pandemic will not be easily controlled and that a second nationwide wave is likely to occur in Korea. The country’s preparedness in various aspects, including the provision of personal protective equipment in hospitals, will be necessary in order to deal with a potential future outbreak efficiently.
KEY MESSAGE
1. The highest proportion of the Korean infectious disease specialists envisaged the current coronavirus disease 2019 (COVID-19) outbreak to end after December 2020
2. N95 respirators were considered to be the most important item in hospitals while securing hospitals designated specifically for the treatment of infectious diseases was the most important policy to be implemented at the national level.
3. The respondents stated that the most important measures to be upheld by the public after the end of the outbreak were thorough hand hygiene and avoiding public spaces if one has symptoms of COVID-19.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
We would like to acknowledge all the respondents for their participation in the survey. The authors are also grateful to the Korean Society of Infectious Disease for identifying the target participants for the survey; Editage (www.editage.co.kr) for English language editing; Han-Pyo Hong (Biostatistics Collaboration Unit, Industry-University Cooperation Foundation, Hanyang University) for statistical analysis.