Primary systematic AL amyloidosis with upper gastrointestinal involvement: endoscopic findings of a protein deposition disorder
Article information
A 64-year-old female was admitted to the hospital with complaints of recurrent non-intensive right-sided pain, facial petechiae, 20,2-pound weight loss over the past 10 months. Her physical examination revealed palmar erythema, liver 3 cm below costal margin, non-palpable spleen. Laboratory test results showed leukocytosis, increased level total bilirubin, conjugated bilirubin, aspartate aminotransferase, gamma-glutamyl transpeptidase, alkaline phosphatase, and total cholesterol. The urinalysis showed albumin negative. Abdominal ultrasonography and computed tomography scan with contrast showed considerable hepatosplenomegaly with moderate diffuse parenchymal changes (steatosis) of the liver and pancreas without any sighs of portal hypertension. Upper gastrointestinal endoscopy revealed palatal petechiae, multiple shallow ulcers covered with fibrin along the entire length of the esophagus with mucosal friability, spontaneous hemorrhage, atrophic gastritis with erosions and regions of intestinal metaplasia with erosions of the duodenal mucosa (Fig. 1). Histopathological examination of esophageal and gastric mucosa biopsy demonstrated diffuse eosinophilic deposition within the lamina propria of mucosa, muscularis mucosa, and vessels walls in the submucosa. Staining of the specimens with Congo red for amyloid deposits was strongly positive (Fig. 2). The results of ultrasound-guided liver biopsy revealed amorphous material stained by Congo red stain demonstrating characteristic positive birefringence under polarized light. λ-Light chains (ALs) were identified by immunohistochemical analysis. AL amyloidosis was confirmed. Treatment with bortezomib, melphalan, and dexamethasone was prescribed.

(A) Upper gastrointestinal (GI) endoscopy showing multiple shallow ulcers covered with fibrin along the entire length of the esophagus with mucosal friability. (B) Upper GI Endoscopy showing atrophic gastritis with erosions and regions of intestinal metaplasia. (C) Upper GI Endoscopy showing erosions of the duodenal mucosa with a fine granular appearance.
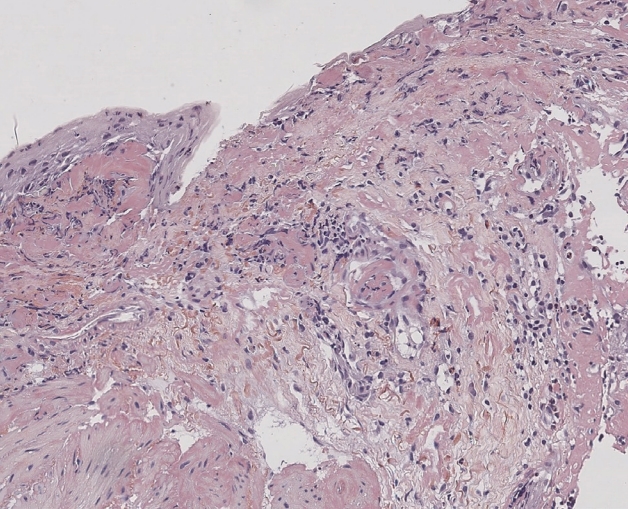
Histopathological section revealed diffuse congophilic deposition within the lamina propria of mucosa, muscularis mucosa and vessels walls in the submucosa of esophageal mucosa (Congo red stain, ×200).
AL amyloidosis is associated with a poor prognosis with a median survival time of 7.95 months for patients with gastrointestinal involvement. Endoscopic mucosal findings are nonspecific and variable, including erosion, ulcers, stricture and easily bleeding mucosa, and/or submucosal hematoma should suspect amyloidosis. Till date, at least 36 human precursor proteins of amyloid have been identified. The most common type of this disease is AL amyloidosis secondary to plasma cell dyscrasia, with an incidence of 9.7 to 14.0 per million person-years. Gastrointestinal amyloidosis is less common in primary systematic amyloidosis, with only 1% incidence.
Informed consent was obtained from the patient for the publication of this case.
Notes
No potential conflict of interest relevant to this article was reported.
