Analysis of risk factor and clinical characteristics of angiodysplasia presenting as upper gastrointestinal bleeding
Article information
Abstract
Background/Aims:
Angiodysplasia is important in the differential diagnosis of upper gastrointestinal bleeding (UGIB), but the clinical features and outcomes associated with UGIB from angiodysplasia have not been characterized. We aimed to analyze the clinical characteristics and outcomes of angiodysplasia presented as UGIB.
Methods:
Between January 2004 and December 2013, a consecutive series of patients admitted with UGIB were retrospectively analyzed. Thirty-five patients with bleeding from angiodysplasia were enrolled. We compared them with an asymptomatic control group (incidental finding of angiodysplasia in health screening, n = 58) and bleeding control group (simultaneous finding of angiodysplasia and peptic ulcer bleeding, n = 28).
Results:
When patients with UGIB from angiodysplasia were compared with the asymptomatic control group, more frequent rates of nonantral location and large sized lesion (≥ 1 cm) were evident in multivariate analysis. When these patients were compared with the bleeding control group, they were older (mean age: 67.94 ± 9.16 years vs.55.07 ± 13.29 years, p = 0.03) and received less transfusions (p = 0.03). They also had more frequent rate of recurrence (40.0% vs. 20.7%, p = 0.02).
Conclusions:
Non-antral location and large lesions (≥ 1 cm) could be risk factors of UGIB of angiodysplasia. UGIB due to angiodysplasia was more common in older patients. Transfusion requirement would be less and a tendency of clinical recurrence might be apparent.
INTRODUCTION
Angiodysplastic lesions are characterized by a thin-walled, fragile vascular network with a disrupted architecture, increased permeability, and susceptibility to rupture. In hemorrhage of upper gastrointestinal tract, it is responsible for approximately 1.2% to 8.0% of cases [1-5]. These lesions may occasionally cause severe bleeding. However, the prevalence of the general population is not well known since there are many asymptomatic individuals who are not evaluated by endoscopic procedures [6,7]. Angiodysplastic lesions are usually small blood vessels visualized within the mucosal and submucosal layers of the gastrointestinal tract. Histologically, the affected vessels are lined by endothelium only with little or no smooth muscle. Endoscopically, they are flat or slightly raised, bright red in color, and well circumscribed or fernlike stellar dendrite lesions usually 2 to 10 mm in diameter. The red area appears to be composed of small blood vessels and it is surrounded by a pale area or halo.
Nowadays, these lesions are increasingly detected, possibly because of the improvements in endoscopic imaging technology and increased chance of endoscopic evaluation. However, there are limited data of the literature on clinical characteristics and long term follow-up of gastrointestinal angiodysplasias. Although upper gastrointestinal bleeding (UGIB) from angiodysplasia in patients with chronic renal failure has been reported [3,8,9], the associated clinical features of UGIB caused by angiodysplasia have not been fully characterized.
In this study, we aimed to analyze the risk factors and clinical characteristics of angiodysplasia presented as UGIB. We compared them with an asymptomatic control group (incidental finding of angiodysplasia in health screening) and estimated the risk of bleeding. Also, we compared them with bleeding control group (simultaneous finding of angiodysplasia and peptic ulcer bleeding) and evaluated the clinical characteristics and outcome.
METHODS
Patients and study design
Between January 2004 and December 2013, a consecutive series of patients who had UGIB and admitted to St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea were retrospectively analyzed. Eighty-eight patients were identified to have angiodysplasia of gastrointestinal tract bleeding after endoscopic examination (esophagogastroduodenoscopy, colonoscopy, capsule endoscopy) (Fig. 1) and were admitted to hospital. Hereditary haemorrhagic telangiectasia, gastric antral vascular ectasia (GAVE), radiation-induced vascular ectasia, and Dieulafoy’s lesions were excluded. We selected the cases that presented UGIB and identified the lesion by esophagogastroduodenoscopy. A total of 35 patients were enrolled in this study.
(A) Multiple round angiodysplasias are observed in the gastric body (upper, bleeding episode; low, stable state). (B) Bleeding from angiodysplasias is observed (upper, bleeding episode) and hemostasis is completed with argon plasma coagulation (low, stable state).
We compared the UGIB group from angiodysplasia with an asymptomatic control group. The asymptomatic control group was composed of 58 individuals who had incidental findings of angiodysplasia in a health screening center, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea. Also, we compared with a bleeding control group and excluded a bias of bleeding itself to identify the characteristics of bleeding from angiodysplasia. The bleeding control group was composed of 28 patients who had simultaneous findings of angiodysplasia with UGIB due to other causes (gastric ulcer and duodenal ulcer bleeding).
Definition and data collection
UGIB was defined as the objective evidence of bleeding with melena, hematochezia, presence of fresh bloody vomitus, abrupt drop of more than 2 g/dL of hemoglobin level, and identified endoscopic finding [8]. Age, sex, smoking and alcohol history, characteristics of angiodysplasia (location, size, number), presence of gastric atrophy, and ulcers were evaluated. Also, comorbid illnesses, hypertension (blood pressure ≥ 140/90 mmHg or on medication), diabetes (fasting blood sugar [FBS] ≥ 126 mg/dL or hemoglobin A1c ≥ 6.5% or on medication), chronic kidney disease (serum creatinine concentration ≥ 1.2 mg/dL for 3 months), chronic liver disease (liver cirrhosis), cardiovascular disease (heart failure, arrhythmia, valvular heart disease, coronary artery disease), and medication history (nonsteroidal anti-inflammatory drugs [NSAIDs], aspirin, and anti-coagulants) were evaluated.
Statistical analyses
SPSS version 18.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. All continuous variables were reported as the mean ± SD. Student t test was used for continuous variables and a chi-square test for categorical data. Logistic regression analysis was used to compare between the two groups. Statistical significance was accepted for a two-sided value of p < 0.05.
Ethics statement
This study was approved by the Institutional Review Board of The Catholic University of Korea (VC14RISI0244).
RESULTS
The clinical characteristics of patients with UGIB from angiodysplasia compared with asymptomatic control group are shown in Table 1. In the group of 35 patients with UGIB from angiodysplasia, the mean age was 67.9 years and 17 (48%) were men. In the group of 58 patients with asymptomatic individuals of angiodysplasia, the mean age was 60.0 years and there were 28 men (48%). Comorbidities included chronic renal disease (n = 7), chronic liver disease (n = 5), congestive heart failure (n = 7), and diabetes mellitus (n = 14). Eleven patients were taking medications including NSAIDs, aspirin, and anti-coagulants.

Clinical characteristics of patients with UGIB from angiodysplasia compared with the asymptomatic control group
Among the patients with UGIB from angiodysplasia, 14 (40.0%) had recurrent bleeding events. At initial endoscopy, bleeding stopped spontaneously in 18 patients (51.4%). Endoscopic treatments including argon plasma coagulation (n = 20), hemoclips (n = 4), and combined (n = 3) were performed in 21 patients. In three patients with recurrent bleeding episodes, the medications including hormonal therapy (n = 2) and high dose of tranexamic acid (n = 1). These did not terminate the bleeding episodes, but did reduce the requirement for transfusion.
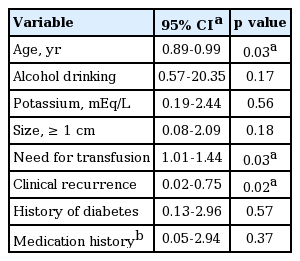
When patients with UGIB from angiodysplasia were compared with the asymptomatic control group, there were significant differences of age, hemoglobin level, hematocrit, blood urea nitrogen, sodium, albumin, FBS, non-antral location (body/fundus), and size of the lesion (≥ 1 cm) in univariate analysis. Also, history of diabetes and medication history (NSAIDs, aspirin, and anti-coagulants) were different. On multivariate analysis, there were significant differences of non-antral location (body/fundus) and size of the lesion (≥ 1 cm) (Table 2). Underlying comorbidities, such as chronic liver disease, chronic renal disease, congestive heart failure, hypertension, and diabetes mellitus, were not associated with UGIB from angiodysplasia. Medication history was not also related with UGIB from angiodysplasia.
Multivariate analysis for upper gastrointestinal bleeding from angiodysplasia compared with asymptomatic control group
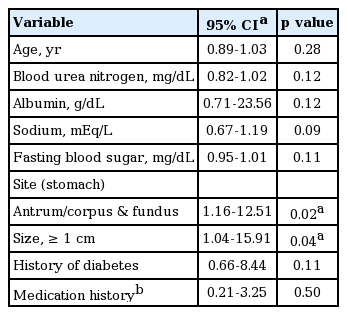
The clinical characteristics of patients with UGIB from angiodysplasia compared with simultaneous finding of angiodysplasias with peptic ulcer bleeding are shown in Table 3. On multivariate analysis, UGIB from angiodysplasias were more common in older patients (mean age: 67.94 ± 9.16 years vs. 55.07±13.29 years, p = 0.03) and the patients received fewer transfusions (p = 0.03). They had more frequent rate of recurrence (40.0% vs. 20.7%, p = 0.02) (Table 4).
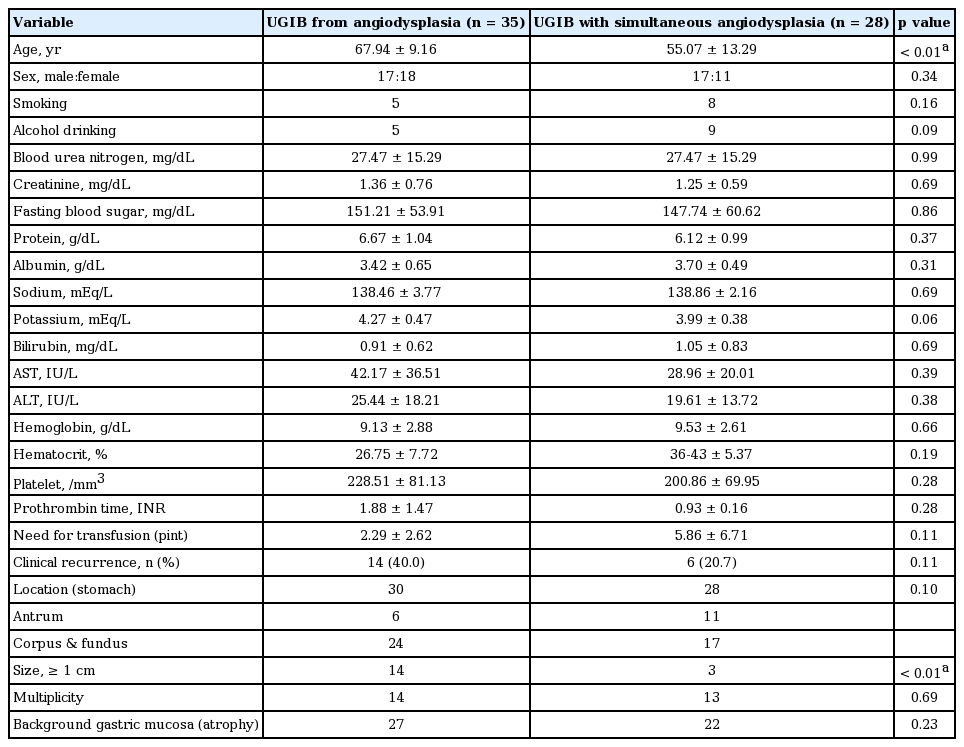
Comparison of upper gastrointestinal bleeding (UGIB) from angiodysplasia and UGIB with bleeding control group (simultaneous finding of angiodysplasia and bleeding of other causes)
DISCUSSION
Angiodysplasias are degenerative lesions of previously healthy blood vessels. Confusion about the exact nature of these lesions has resulted in various terms that include arteriovenous malformation, hemangioma, telangiectasia, and vascular ectasia. Among them, two widely-used terms are telangiectasia and angiodysplasia. The former applies to isolated mucosal vascular ectasias, while the latter is usually applied to gastrointestinal lesions [10]. Angiodysplasias have been reported in association with aortic valve disease, systemic sclerosis, hereditary hemorrhagic telangiectasia, and in patients on chronic hemodialysis [8,11-13]. Herein, we studied the acquired form of angiodysplasias; and other vascular lesions such as GAVE or radiation-induced vascular ectasia were excluded because of their relation with a specific disease. Dieulafoy lesions were also excluded because of their somewhat different pathophysiology with angiodysplasias. The etiology, pathophysiology, and clinical characteristics of angiodysplasias remain unclear. It is presumed that angiodysplasias of the stomach have evolved from the similarity of colonic type [14]. Intermittent submucosal venous obstruction, intermittent arterial flow, and local vascular degeneration with local hypoxemia may be potential etiologic factors [10,15,16].
Multiple lesions and use of anticoagulant agents are risk factors of bleeding. In patients experiencing at least one episode of overt UGIB, multiple lesions were found in 63% of cases [17]. In this study, there were strong associations with UGIB from angiodysplasia, when angiodysplasia was larger than 1cm or associated with non-antral location (gastric body/fundus). The multiplicity and co-existence of chronic renal insufficiency were not related with UGIB from angiodysplasia. As for multiplicity, there were 40% of our cases in UGIB from angiodysplasias, whereas there were 39.7% of cases in asymptomatic angiodysplasias. As for chronic renal failure associated with UGUB from angiodysplasias, patients with chronic renal failure were more likely to have coagulopathies that were related to platelet defects and abnormal function of von Willebrand factor [18]. However, this finding has not been a consistent result. It is thought that chronic renal failure contributes the formation of angiodysplasias, but may not be a risk factor of UGIB. Broader studies will be required before any definitive conclusions can be drawn.
In our study, it was noteworthy that non-antral location (gastric body/fundus) of angiodysplasia was a risk factor of bleeding. Previously, it was hypothesized that the vigor of muscular contraction in the antrum is much greater than elsewhere in the stomach, possibly predisposing to venous obstruction and subsequent vascular ectasia [19]. However, whether a similar theory of venous obstruction should be proposed for gastric lesions is uncertain. Furthermore, our result was opposite and a non-antral location of angiodysplasias had a tendency of UGIB. Recently, it was suggested that increased expression of an angiogenic factor likely has a pathogenic role in human angiodysplasia. Vascular endothelial growth factor (VEGF) has been identified as the key mediator for angiogenesis [20]. Different stimuli induce VEGF expression, including hypoxia, growth factors, cytokines, nitric oxide, hormones, and oncogenes. Abnormal concentrations of VEGF result in aberrant angiogenesis with formation of angiodysplastic lesions that lack a smooth muscle cell layer and are more susceptible to rupture and bleeding [21-23]. It was thought that gastric body might be prone to damage for the endogenous stimuli that induce high concentration of VEGF.
On univariate analysis, history of diabetes mellitus and medication including NSAIDs or aspirin were associated with bleeding, but on multivariate analysis there were no statistical significances. Although our result revealed that diabetes mellitus was not risk factor of bleeding, it was not known whether glycemic control was related with UGIB from angiodysplasia. Hypothetically, hyperglycemia could be an essential cause of reactive oxygen species-mediated oxidative stress by nicotinamide adenine dinucleotide phosphate oxidase [24-27]. As for association with the use of NSAIDs, aspirin, or anti-coagulants, only a few case reports are available. There is no scientific evidence. Further studies would be needed to elucidate whether diabetes mellitus contributes to bleeding of angiodysplasias and whether strict control of blood sugar can reduce the risk of bleeding. Also, the association with use of the aforementioned drugs and bleeding of angiodysplasias must be studied.
Clinical presentation of UGIB from angiodysplasias is usually characterized by maroon-colored stool, melena, or hematochezia. Bleeding usually is self-limited, but it can be chronic, recurrent, or even acute and life threatening. Sometimes, iron deficiency anemia and stools that are intermittently positive for occult blood can be the only manifestations of angiodysplasias [3]. In our results, bleeding stopped spontaneously in over 50% of cases and the recurrence was up to 40% of cases. Recently, a meta-analysis revealed that pooled recurrence bleeding rate was 36% over a mean of 22 months [28]; this result is compatible with the present findings. This suggests that upper gastrointestinal bleeding from angiodysplasias would display a similar pattern of small bowel or colon type.
There were several limitations in this study. First, this study had a single-center, retrospective design. The enrolled patients of the study were admitted to a hospital and asymptomatic patients with chronic anemia who did not have admission could be under-evaluated. Second, the number of patients with angiodysplasia included was relatively small. From this consideration, it would be possible that other variables including drug history and comorbidities were not conclusive. Third, area of angiodysplastic lesion would be more important risk factor of bleeding than diameter of the lesion. However, in clinical practice, it is very difficult to calculate the area of lesion. Fourth, the diagnosis of angiodysplasias may be easily missed on endoscopy unless this is performed by an experienced operator.
In conclusion, angiodysplasias that were larger than 1 cm or located in a non-antral area (gastric body/fundus) would have a bleeding risk. Clinically, UGIB from angiodysplasias was more common in older patients. The transfusion requirement would be less and tendency of clinical recurrence might be apparent. Further experiences and large scaled studies would be anticipated to elucidate risk factors of UGIB from angiodyspalsias.
KEY MESSAGE
1. Angiodysplasias that were larger than 1 cm or located in a non-antral area (gastric body/fundus) would have a bleeding risk.
2. Clinically, upper gastrointestinal bleeding from angiodysplasias was more common in older patients. The transfusion requirement would be less and tendency of clinical recurrence might be apparent.
Notes
No potential conflict of interest relevant to this article was reported.