A Case of Systemic Lupus Erythematosus Presenting as Malignant Hypertension with Hypertensive Retinopathy
Article information
Abstract
The variability of cardiovascular abnormalities is one of the characteristics of systemic lupus erythematosus (SLE). Among the cardiovascular manifestations, hypertension is reported in 14% to 58.1% of patients in diverse ethnic populations, and remains a clinically important issue due to its close relationship with early mortality in patients with SLE. The development of hypertension in patients with SLE has been associated with advanced lupus-related renal disease and the medications used for the treatment of lupus. Malignant hypertension is a serious complication of hypertension; it rarely occurs in patients with SLE. However, it can occur in patients with other complicated medical conditions such as the antiphospholipid antibody syndrome (APS) or cardiac tamponade. Here, we report the case of a patient with SLE and malignant hypertension with hypertensive retinopathy that initially presented without clinical evidence of APS or hypertensive nephropathy.
INTRODUCTION
Systemic lupus erythematosus (SLE) is a systemic autoimmune disease that is characterized by a wide spectrum of clinical manifestations, including renal, pulmonary, cardiovascular, and neuropsychiatric abnormalities [1]. In particular, cardiovascular manifestations such as myocarditis, valvular heart disease, pericardial effusion, coronary heart disease, and systemic hypertension have been widely recognized in patients with SLE.
Keith et al. [2] initially described malignant hypertension as a disease entity. Prior to the development of effective anti-hypertensive drugs, malignant hypertension lead to death within about one year after diagnosis. However, the incidence and mortality of malignant hypertension has declined since the development of new therapeutic strategies, including artificial renal replacement therapy and novel medications that are capable of effectively controlling hypertension-related mechanisms or pathways [3]. Malignant hypertension may develop with either essential or secondary hypertension resulting from the underlying or as a disease complication. The main causes of secondary malignant hypertension are thought to be parenchymal renal or renovascular lesions irrespective of the underlying disease [3]. Malignant hypertension has been reported in association with autoimmune rheumatic diseases and in patients with the antiphospholipid antibody syndrome (APS) alone or with SLE and is relatively well described in the medical literature [4]. However, malignant hypertension as the initial presentation of SLE, alone without APS, has not been previously reported. Here, we report a case of lupus nephritis presenting with malignant hypertension, without clinically evident APS, and hypertensive nephrosclerosis on renal biopsy.
CASE REPORT
A 38-year-old woman was referred for the evaluation of visual disturbance and headache lasting for over 3 weeks. Two weeks prior to her visit to our clinic, the patient complained of myalgia, cough and non-productive sputum without clearly identifiable causes. In addition, the visual disturbance and headache were worsening. The patient visited the department of ophthalmology for the visual disturbance, and was diagnosed with hypertensive retinopathy. Anithypertensive medications were prescribed.
The physical examination at the initial visit revealed high blood pressure, 190/110 mmHg, a respiration rate of 25/min and a heart rate of 113 beats/min. The breath sounds at the left lung field were decreased and mild pitting edema of both lower extremities was noted.
The laboratory studies included a complete blood count and acute phase reactants, the results showed: white blood count 3,700/mm3, hemoglobin 9.4 g/dL, platelets 12,700/dL, erythrocyte sediment rate 50 mm/hr (normal < 20 mm/hr), and C-reactive protein 8.5 mg/dL (normal < 0.5 mg/dL). Routine chemistry revealed some abnormal results, including a total protein 6.9 g/dL, albumin 2.8 g/dL, creatinine 1.6 mg/dL (normal < 1.5 mg/dL), and cholesterol 202 mg/dL. Immunological screening for autoimmune diseases showed an antinuclear antibody (ANA) titer of 1:320 with a speckled pattern, and 56.10 IU/mL of antibody to anti-double-stranded DNA (normal < 5 IU/mL). The complement levels were decreased to 37.9 mg/dL for C3 and 4.3 mg/dL for C4. Tests for the lupus anticoagulant, anti-cardiolipin antibody of IgM, IgG and IgA, anti β2-glycoprotein1 (β2-GP1), and venereal disease research laboratory test (VDRL) were all negative. The initial urinalysis showed albumin 2+, red blood cell count > 30/HPF and WBC 1 to 3/HPF in a spot urine. Significant proteinuria of 6,489 mg was calculated in the 24-hour urine. Plain chest radiography showed cardiomegaly with a moderate left pleural effusion. Renal arterial stenosis was not detected on the computed tomography angiography of the abdomen. The findings of the transthoracic echocardiography revealed a small to moderate pericardial effusion, large left pleural effusion with fibrinous material, enlargement of the left atrium, and left ventricular concentric hypertrophy. On the fundoscopic examination, serious retinal detachment, cotton-wool spots and retinal hemorrhages, of both eyes were, compatible with a hypertensive retinopathy grade III (Fig. 1A). Magnetic resonance imaging with angiography of the brain showed no definite abnormal findings.
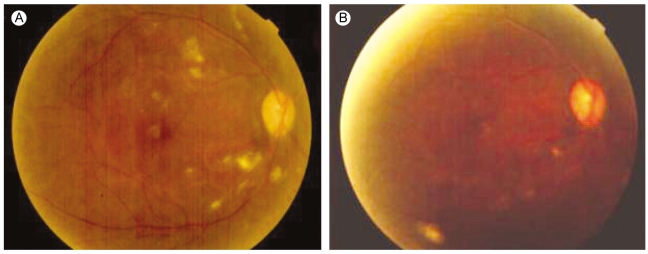
(A) Retinal detachments, multiple cotton-wool spots and retinal hemorrhages noted before treatment. (B) After treatment, retinal hemorrhages, cotton-wool spots and detachments were nearly resolved.
The patient was diagnosed with SLE based on the clinical features and laboratory results including the ANA, pleural and pericardial serositis, anti-dsDNA, and renal involvement with massive proteinuria; the findings fulfilled the American College of Rheumatology classification criteria for the diagnosis of SLE [5]. The patient also met the World Health Organization (WHO) criteria for malignant hypertension. The renal biopsy revealed a membranous lupus nephritis according to the WHO histopathology criteria; there was no evidence of hypertensive nephrosclerosis.
The blood pressure of the patient was well controlled near 120/80 mmHg with a combination of several anti-hypertensive medications, including a calcium-channel blocker, an angiotensin receptor blocker and beta-blockers. Fundoscopic examination, after 5 months of therapy, showed near resolution of the retinal hemorrhages, detachments and cotton-wool spots (Fig. 1B). Prednisolone (1 mg/kg/day) in combination with intravenous cyclophosphamide (750 mg dose/month) were administered for the lupus nephritis. The prednisolone was slowly tapered. However, the patient could not tolerate the serial cyclophosphamide therapy after three treatments; the medication was changed to 100 mg of azathioprine, 200 mg of hydroxychloroquine and 5 mg of prednisolone to control the lupus disease activity. The patient had a normal serum creatinine level. However, the 24-hour urine had 3,496 mg of protein. At present, the visual acuity has recovered and the patient is stable.
DISCUSSION
This case illustrates the course of a patient with the unusual initial presentation of lupus nephritis with malignant hypertension; the patient had no clinical features of APS and hypertensive nephropathy on renal biopsy. Malignant hypertension is characterized by markedly elevated blood pressure associated with ischemic retinal injury consistent with grades III or IV hypertensive retinopathy; it is one of the most serious complications of hypertension. In addition to the ocular features of visual disturbance, transient ischemic attack and papilledema, it may be associated with renal abnormalities such as arteriolar fibrinoid necrosis and onionskin lesions, as well as hematological abnormalities such as microangiopathic hemolytic anemia [6]. Malignant hypertension may develop in patients with either essential hypertension or hypertension resulting from secondary causes related to advanced renal parenchymal diseases such as glomeronephritis, scleroderma, analgesic nephropathy, or radiation nephropathy and renovascular stenosis [3].
The cardiovascular manifestations associated with SLE are variable, and include conditions such as pericarditis, impairment of left ventricular function, early coronary atherosclerosis, valvular heart disease, and systemic arterial hypertension. Hypertension has not been considered as a clinically important feature of SLE. However, hypertension has become a major concern because it is associated with early mortality related to the variable atherosclerotic events or renal damage associated with lupus nephritis. Reports on the prevalence of hypertension in patients with SLE vary from 14% to 58.1% in different ethnic populations [7].
There have been a number of studies correlating the clinical features of SLE with the development of hypertension. Among them, are reports that the development of hypertension, in patients with SLE, was more common in patients with advanced lupus-related renal pathology or impairment of renal function. However, Budman and Steinberg [7] demonstrated that the presence of significant renal disease was not a necessary condition for the development of hypertension; they found that the creatinine clearance and nephritic range proteinuria (more than 3.0 g of urine protein per 24 hours) were not significantly different in hypertensive patients compared to normotensive patients.
In addition to advanced renal disease as a cause of hypertension, anti-rheumatic drugs including corticosteroids and cyclosporin might be associated with either the onset or aggravation of hypertension. However, one report has indicated no correlation between the use of corticosteroids and hypertension [7]. Interestingly, in a retrospective analysis of SLE patients, Kaplan et al. [8] demonstrated that hypertension developed less frequently in patients with rheumatoid-like arthritis than in patients without persistent arthritis. The high dose steroid therapy, used to treat the lupus nephritis, had no influence on the management of hypertension in this case.
There are few reports on the clinical presentation of malignant hypertension in patients with SLE in the medical literature [3]. Most prior cases with malignant hypertension occurred during the course of treatment with high dose corticosteroids or with the development of complicated medical issues, such as cardiac tamponade.
Malignant hypertension is relatively more common in SLE patients with clinical features of APS compared to the SLE patients without APS [4]. Malignant hypertension in APS is associated with variable renal manifestations such as renal artery stenosis, renal infarction, thrombotic microangiopathy, renal vein thrombosis, or glomerulonephritis; these renal abnormalities mainly result from thrombosis formation at any of the renal vessel sites [9]. For the patient presented in this report, investigations were conducted to determine whether there was evidence of APS. The studies included renal angiography using computed tomography, serologic markers for lupus anticoagulant, VDRL, β2-GP1, and anticardiolipin antibody. In addition, the renal pathology on a biopsy specimen did not show any of the findings compatible with APS, such as fibrinoid necrosis or onionskin lesions. Therefore, none of the studies performed supported the diagnosis of APS.
SLE related retinopathy is one of most serious ocular findings in this disease. It may lead to loss of vision in untreated patients. Although a well-defined classification of retinopathy has not yet been established, Giorgi et al. [10] proposed a practical classification based on the pathogenesis and clinical features. The association with either lupus retinal vasculitis or atherosclerosis suggests the "classic type" retinopathy, whereas the Hughes' retinopathy is related to retinal thrombosis due to antiphospholipid bodies. Appropriate therapeutic strategies for lupus-related retinopathy should be determined according to the classification of retinopathy. Immunosuppressive therapy or prophylactic low dose aspirin can be effective for the treatment of retinal vasculitis or atherosclerotic changes. Despite the high dose steroid and cyclophosphamide therapy used in this case, more than 3 months were required for improvement of the visual acuity. This suggested that the ocular abnormalities were due to hypertensive retinal changes rather than a retinal vasculitis.
In conclusion, we present a case that illustrates that hypertension may be a clinically important in the initial diagnosis of patients with SLE and associated with the development of diverse cardiovascular events in these patients. Further study of the pathogenesis and clinical effects of malignant hypertension on the courses of SLE is needed.
Notes
No potential conflict of interest relevant to this article was reported.