A Case of Pulmonary Vein Tumor Presenting as a Left Atrial Mass
Article information
Abstract
Primary cardiac tumors are extremely rare and can originate within the heart or be the result of tumor spread from other sites. We report a female patient with a pulmonary vein tumor extending into the left atrium that had a suspicious primary malignant origin with a sacral metastatic carcinoma. The patient was admitted complaining of pain in her buttock area as a result of a sacral tumor. It was believed that the sacral tumor was a metastasis from the imaging study and clinical manifestation. The primary malignant origin was evaluated. The chest CT showed a left atrium thrombus-like lesion without a pulmonary abnormality. After a transesophageal echocardiogram, the patient was diagnosed with a pulmonary vein tumor extending to the left atrium. The patient was given palliative radiotherapy for the sacral pain. Initially, the clinical impression was a metastatic sacral tumor with a thromboembolism of the left atrium. However, this patient was finally diagnosed with a pulmonary vein tumor with a left atrium extension by a transesophageal echocardiogram.
INTRODUCTION
Primary tumors of the heart and great vessels are rare. The incidence of primary tumors of the heart is 0.0017% at autopsy, of which 28% are malignant1-3). Tumors involving the aorta, pulmonary vessels, inferior vena cava are quite rare, appearing in the literature mainly in case reports or in a small retrospective case series. These tumors were diagnosed by a thromboembolic event or an obstruction of the vessel. Magnetic resonance imaging (MRI) and a transesophageal echocardiogram (TEE) are useful in differentiating tumors of the great vessels from a thrombus or adjacent pulmonary tumors.
Approximately twenty cases of a tumor from the pulmonary vein have been described since 19392-8). These tumors can extend to the left atrium and invade the mediastinum and lungs. We report the first case of a pulmonary vein tumor extending to the left atrium in Korea.
CASE REPORT
A 69-year-old female was admitted to our hospital complaining of pain in both buttocks and voiding difficulty. She had no history of hypertension, tuberculosis, diabetes or operation. She complained pain in both buttocks, which had persisted for two months as well as voiding and defecation difficulty for one month. She visited the primary clinic and was diagnosed with a metastatic sacral tumor from the lumbar MRI. She was then transferred to our hospital. She did not complain of dyspnea on exertion or hemoptysis. She had an acute ill-looking appearance but had a normal mental state. Her vital signs were as follows: blood pressure 130/90 mmHg, pulse rate 76/min, respiration rate 20/min, body temperature 36.6℃. The physical examination of the chest was normal without a murmur or abnormal lung sounds. The neurological examination of both lower extremities was unremarkable. The tender point of both buttocks radiating to the right anal area was located. The anal tone was normal but the contraction was decreased.
The laboratory examination showed a WBC of 12,300/mm3, hemoglobin of 9.1 g/dL, platelet of 402,000/mm3 and an unremarkable chemistry. The CEA was normal range as 0.51 ng/mL. The chest radiography revealed no cardiomegaly and the pelvic radiography was unremarkable. Abdominopelvic computed tomography (CT) showed a non-calcified and osteoclastic sacral tumor indicative of a metastasis but no other tumor in the abdominal and pelvic cavity (Figure 1). The finding of Chest CT was a 5.5×2.5 cm sized thromboembolism-like mass on the right inferior pulmonary vein and left atrium (Figure 2A, 2B).
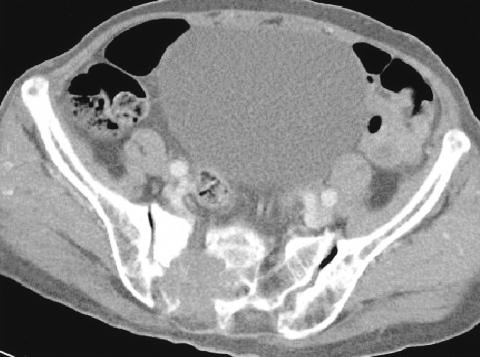
Abdominopevic CT showing 5.0×4.5 cm sized, osteoclastic and non-calcified sacral mass. The others are normal.

(A) 3D reconstruction of the chest CT show a filling defect in the left atrium. (B) Chest CT showing a mass in the left atrium and a pulmonary vein. It appears similar to a pulmonary thromboembolism.
Transthoracic echocardiography (TTE) was performed to evaluate the thromboembolism. TTE revealed a huge round-shaped, well-marginated, homogenous, echogenic and 5.38×2.82 cm sized mass arising from the right inferior pulmonary vein (Figure 3A, 3B). TEE revealed a huge, variable shaped (round to irregular), well marginated and homogenous mass out of the left atrium through right inferior pulmonary vein that was indicative of metastatic cancer (Figure 3C, 3D).

(A) Transechocardiography, apical four chamber veiw. This showed a huge, round-shaped ,well-marginated, homogenous and echogenic mass (arrow) arising from right inferior pulmonary vein. (B) Transechocardiography, apical two chamber view. This showed 5.38×2.82 cm sized mass (arrow) that occupied left atrium. (C) Transesophageal echocardiography, mid-esophageal four chamber view. this showed a variable shaped (round to irregular), well marginated and homogenous mass (arrow) being out on left atrium. (D) Transesophageal echocardiography, mid-esophageal four chamber view. this showed a huge mass (arrow) that occupied left atrium.
It was believed that the sacral tumor was a metastatic carcinoma considering the age of the patient because the sacral tumor showed an osteoclastic mass without calcification on the abdominopelvic CT (Figure 1) and a metastatic tumor on the MRI. Therefore, it was concluded that a primary carcinoma might be a pulmonary vein tumor. A surgical biopsy of sacral metastatic tumor was performed. Histologically, the majority of the specimen was blood. Two nests of epithelioid tumor cells were floating in the fibrinated blood. The round to ovoid tumor cells contained a moderate amount of cytoplasm and irregular hyperchromatic nuclei. Singly scattered tumor cells were also admixed with inflammatory cells (Figure 4A). Immunohistochemically, the tumor cells were positive for pancytokeratin (Figure 4B) but negative for the leukocyte common antigen (LCA) and vimentin. These findings were consistent with a metastatic carcinoma. A further examination was made to locate another primary tumor of the metastatic sacral carcinoma. However, no other primary tumor could be found. Therefore, the final diagnosis was a primary tumor of pulmonary vein with sacral metastasis. Open-heart surgery could not be performed because of the patient's old age and poor general condition. Therefore, palliative radiation therapy was performed and analgesics were administered for sacral pain management.
DISCUSSION
Tumors from the pericardiac tissue are extremely rare. Only twenty cases of tumors from the pulmonary vein have been described2-7, 9). In 1939, Ausbuettel et al reported the first case of a pulmonary vein tumor by autopsy1). During the 1990s, patients with a pulmonary vein tumor were treated by open-heart surgery2-6, 8-10). The common symptoms of the patients with pulmonary vein tumor were dyspnea, cough, or hemoptysis. Death during surgery occurred in 2/20 cases, but the others had good survival if there was no local metastasis. The pathological diagnosis was a sarcoma or leiomyosarcoma1-5, 7, 8, 10). Sarcomas of the inferior vena cava, in contrast to those of the aorta and pulmonary artery, tend to be well-differentiated leiomyosarcomas. Many tumors of the pulmonary vein are leiomyosarcoma11).
Our patient was a 69 year-old female with the chief complaint of sacral pain due to a bony metastasis but there were no symptoms of the pulmonary vein tumor. The chest CT of this patient showed a thrombus-like lesion of the left atrium. TTE and TEE was performed, which showed no mass attached to the left atrial wall and a right inferior pulmonary vein mass extending to the left atrium. Although we could not exclude a myxoma or thrombus, it was believed that a mass originating from the pulmonary vein could be a tumor. Most patients with a pulmonary vein tumor had dyspnea, cough that was induced by the tumor1-10). An incidental diagnosis is rare4). In addition, some patients had a local metastasis to the adjacent organ (mediastinum, lung, lymph node etc.), but no distant metastasis. Our case had a pulmonary vein tumor and a sacral metastasis. A search was made for other primary malignancies except for the pulmonary vein tumor but none could be found. Although open-heart surgery could not be performed to confirm the diagnosis, the final diagnosis was a pulmonary vein tumor and sacral metastasis. It is possible that other diagnoses such as a malignancy of an unknown primary origin with the pulmonary vein and sacral metastasis or primary sacral tumor with a pulmonary vein metastasis could have been made. Generally, a metastatic pulmonary vein tumor originates from the lung but this patient had no pulmonary abnormality on the chest CT12-14). In addition, MRI and abdominopelvic CT of this patient showed a sacral tumor that was indicative of a metastatic rather than primary malignancy15). A surgical biopsy of the sacral tumor was performed, which was diagnosed as a metastatic carcinoma. Pathologically, a sarcoma or leiomyosarcoma shows a positive reaction in vimentin, cytokeratin, desmin, smooth muscle actin (SMA). The sacral tumor of our patient was negative to these immunohistochemical stains, and a metastatic carcinoma was diagnosed. In the prescribed cases, the pathologic diagnosis was a sarcoma or leiomyosarcoma but not a carcinoma.
We report a case of pulmonary vein tumor extending to the left atrium mimicking a thromboembolism.
