Clinical and Bronchoscopic Findings in Ugandans with Pulmonary Kaposi's Sarcoma
Article information
Abstract
Background
Pulmonary Kaposi's sarcoma (PKS) directly affects the life expectancy of those infected and yet the clinical and radiographic features of Kaposi's sarcoma (KS) with pulmonary involvement are nonspecific, which makes diagnosis difficult. In Uganda, pulmonary tuberculosis, which has clinical features that closely resemble those of PKS, also occurs commonly and thus confusion is bound to arise. Bronchoscopy is a recognized diagnostic investigatory modality for PKS. The aim of present study was to identify unique or useful points for the differential diagnosis of PKS and other opportunistic infections.
Methods
The clinical, radiologic, and bronchoscopic findings in thirty-five Ugandan patients (age 20-50, median 32) with PKS were analyzed.
Results
Cough and weight loss were most common and occurred in 97.1%, whereas fever occurred in 62.9%, and breathlessness in 57.1%. Thirty-four patients (97.1%) showed mucocutaneous KS, and palatal KS was most frequent and was observed in 74.3%. In addition, 25 patients (71.4%) showed the characteristic endobronchial plaques of KS. The most frequently observed radiographic abnormality was bilateral reticulonodular density. Histological examinations of bronchoscopic biopsies revealed KS in 7 (36.6%) cases. Five PFS patients (25%) also had co-existent tuberculosis.
Conclusions
The majority of patients with PKS showed no specific findings on physical examination, apart from mucocutaneous KS. Our findings indicate that palatal KS may be a strong predictor of PKS. In Uganda, pulmonary tuberculosis may be the most common concomitant pulmonary infection in PKS patients.
INTRODUCTION
Kaposi's sarcoma (KS) is the most common malignancy in HIV infected patients, and although KS occurs in persons without HIV in tropical Africa, its prevalence is very low. In western countries, Kaposi's sarcoma is regarded as a disease of homosexual and bisexual men1). But, in Africa the main mode of HIV transmission is via heterosexual intercourse, and thus KS is also commonly found in females. For this reason, the clinical features of pulmonary Kaposi's sarcoma (PKS) in Africa may differ from those in Western countries.
In Uganda, pulmonary tuberculosis, whose clinical features resemble those of PKS, also occurs commonly, and thus these two disease entities are likely to be confused. Clinically we have observed patients who have been administered anti-tuberculous medicine, and who are later proven to have PKS by bronchoscopy. These patients tend to show some improvement initially on anti-tuberculous regimens, but their symptoms return after a few months. Thus, we questioned the progress of these patients, as to whether they had PKS only or whether they had co-existent PKS and pulmonary tuberculosis from the beginning. PKS must be considered in the differential diagnosis of all respiratory patients with HIV/AIDS, and bronchoscopy must be performed to identify its presence; however, it is difficult to perform bronchoscopy on all due to a lack of facilities in Uganda. Therefore, we attempted to determine whether there is some unique or useful point that can be used to differentiate PKS from other opportunistic infections.
MATERIALS AND METHODS
Between June 1993 and July 1997, 236 patients with HIV-infection were examined by fiberoptic bronchoscopy at Mulago hospital, and of these 64 patients had findings of PKS by bronchoscopy. Each of these patients received a complete physical examination and a detailed history-taking by the investigator. Chest X-ray findings were classified according to the predominant abnormality, e.g., unilateral or bilateral reticulonodular densities, increased bronchovascular marking only, or effusion. Those who were not reviewed thoroughly by the investigator were excluded from this study. The study inclusion criteria for PKS were; 1) typical bronchoscopic findings (25 cases), bright red or violaceous raised mucosal lesions (Figure 1), or 2) the presence of KS by biopsy (7 cases), or 3) clinically considered PKS (3 cases) including chest X-ray findings (Figure 2) and no evidence of other pulmonary disorders. Thirty-five patients were eligible for inclusion. Twenty-two patients were men and 13 were women, and their age range was 20-50 (median 32). Bronchoscopic biopsies were obtained in 20 of the cases whose KS lesions were located at bifurcation of bronchi, and bronchoalveolar lavage (BAL) was performed in these cases. Ziehl Neelsen, Leishmann staining and direct fluorescent staining for Pneumocystis carinii were performed on all BAL specimens. Chest X-ray and bronchoscopic findings were compared by the investigator. Infection with HIV was proven by a positive enzyme-linked immunosorbent assay.

Typical bronchoscopic finding of pulmonary Kaposi's sarcoma, bright red or violaceous raised mucosal lesions.
RESULTS
Clinical symptoms
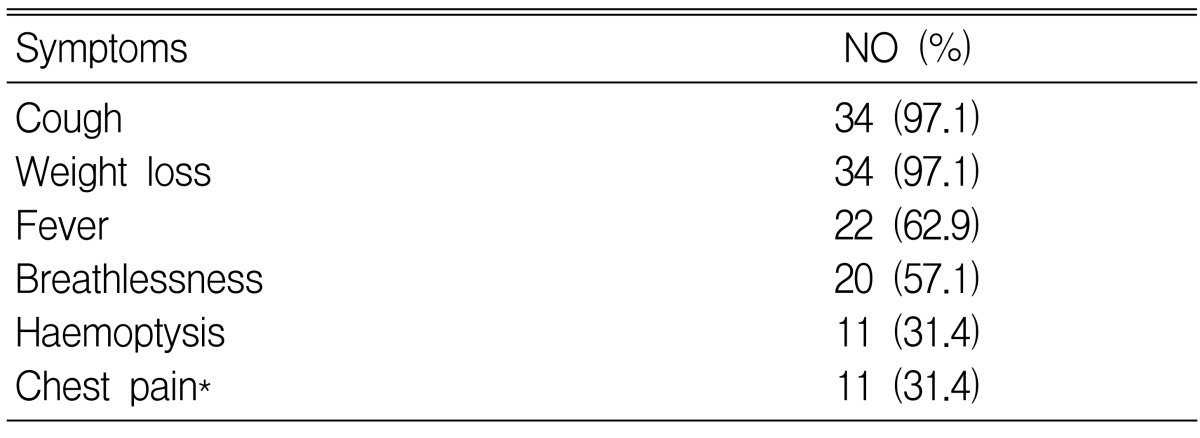
All patients had significant clinical symptoms whether respiratory or general in nature. Coughing and weight loss were most common (97.1%). Fever (62.9%), breathlessness (57.1%), hemoptysis, and chest pain (31.4%) followed. Chest pains were usually retrosternal in nature and this was aggravated by coughing (Table 1).
Physical findings
General examination showed no specific findings except for mucocutaneous KS. Generalized lymphadenopathy was observed in 18 cases (51.4%), and oropharyngeal candidiasis in 8 cases, of which 2 cases showed laryngeal candidiasis without oral candidiasis. Peripheral edema was observed in only 5 cases. But, mucocutaneous KS was observed in 34 (97.1%), and palatal KS was frequently observed 26 (74.3%). Chest findings were minimal. In 3 cases a dullness to percussion was heard, decreased breath sounds were perceived in 2 cases, and rhonchi and crepitations were auscultated in 4 cases each. In 3 cases a pleural friction rub was heard.
Chest radiographs
Thirty-four of the 35 cases showed an abnormal appearance and 1 case had a normal chest radiograph. This one case had lymphadenopathic KS proven by biopsy and was subjected to bronchoscopy because of a cough. The majority of cases showed bilateral reticulonodular density. However 6 cases showed a unilateral lesion and 3 cases showed increased vascular markings only. Pleural effusion was found in 4 cases (Table 2).
Bronchoscopic findings
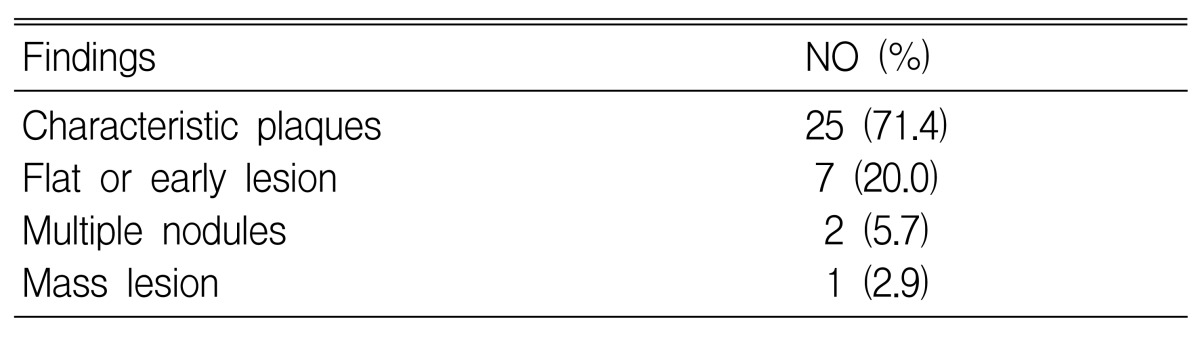
Twenty-five cases showed characteristic plaques (71.4%). A flat or early lesion was found in 7 cases, multiple nodules in 2 cases, and masses in 1 case (Table 3).
Comparison between extent of radiological findings and the severities of bronchoscopic features
The severities of bronchoscopic findings were found to parallel the extents of radiographic lesions in 19 cases (54.2%). Nine cases showed severe bronchoscopic features and 7 less severe features. Further details are provided in Table 4.
Bronchoscopic biopsy and bronchoalveolar lavage
Biopsies were performed in 20 cases, but biopsy results were available for 19. Seven of 19 cases showed Kaposi sarcoma histologically (36.8%). Bronchoalveolar lavage was performed in 20 cases, but the Gram staining results were difficult to interpret because Gram (+) cocci and Gram (-) bacilli were both found but the predominant strain was not identified in most cases. Moreover, Ziehl Neelsen staining showed acid-fast bacilli in 5 (25%) of 20 cases, and 1 case of Cryptosporidium was found. Direct fluorescent staining for Pneumocystis carinii proved positive in one case.
DISCUSSION
Kaposi sarcoma originates from endothelial cells of the blood vessels or lymphatics2). In the past, it was considered to be a rare disease, but KS has gained increased in prominence during the HIV/AIDS era. KS is frequently observed in homosexual males and in women whose partners are bisexual, and these two groups have 4 fold higher KS occurrence rates than their counterparts1). These epidemiological features suggest that cofactors related to sexual habits are important in the transmission of KS, and a viral aetiology has been postulated as the transmissible infectious agent of KS3, 4).
KS is mainly a tumour of the skin and of mucocutaneous surfaces, but it may affect any part of the body. Kaposi sarcoma involving sites other than the respiratory system does not significantly enhance patient morbidity or mortality, whereas pulmonary Kaposi sarcoma adversely affects quality of life and significantly reduces life expectancy. In the case of PKS, in particular, average survival time after diagnosis, in the absence of appropriate treatment, is 6 months or less. Combination chemotherapy with adriamycin, bleomycin, and vincristine has been found effective, but not curative, in the treatment of PKS5-7). The detection of PKS and institution of proper treatment is therefore important.
The incidence of PKS is difficult to assess because, even bronchoscopy fails to establish a diagnosis in every case. Mitchell and Miller reported that only 45% of cases have endobronchial lesions located at segmental orifices in the main trachea or bronchi that are reachable with a bronchoscope8). However, bronchoscopy remains the most useful tool for diagnosing PKS. According to postmortem studies, PKS was found in 47% of patients with cutaneous KS9) and in 59% of patients dying with AIDS had KS, though PFS was not unsuspected premortem in any patient10). Therefore, the incidence of PKS in AIDS patients may be approximately 29%. The bronchoscopic appearance of endobronchial KS is considered to be characteristic enough to allow a diagnosis9, 11). Endobronchial KS lesions have a characteristic violaceous appearance, which to the inexperienced observer, may be confused with another inflammatory process of the bronchial mucosa. Moreover, often a concomitant opportunistic infection is present, which should be evaluated by BAL and by subsequent microbiological analysis of the fluids. PKS should be considered in the differential diagnosis of all HIV infected patients presenting with respiratory symptoms. However, in patients with AIDS, where many opportunistic infections may mimic PKS, this is not always easy.
The most common clinical symptoms found in our study subjects, namely, cough and weight loss, are non-specific symptoms which are equally attributable to other diseases, notably tuberculosis. The most common radiographic abnormality (bilateral reticulonodular shadowing) is also a feature of tuberculosis. The coexistence of opportunistic infections, which is probably a common occurrence in patients with HIV/AIDS, may confound the diagnosis of PKS and mask PKS symptoms. Fever and weight loss were probably common among our study subjects because they tended to present with late stage illness. Fever and weight loss arealso two of the three major criteria employed in the WHO clinical definition of AIDS. However, the finding of haemoptysis in about 31% of our patients may have special significance, in as much as PKS should be considered an important cause of haemoptysis in the Ugandan setting.
All of the study subjects had detectable mucocutaneous KS lesions at locations other than the lungs. In particular, 74.3% had palatal KS lesions, which is consistent with the findings of Moss et al. who suggested that palatal KS may be a strong predictor of PKS12). The finding of palatal KS lesions in a patient with respiratory symptoms increases the possibility of PKS, and thus, it is recommended that such patients should receive a bronchoscopic examination. Oropharyngeal candidiasis was noted in surprisingly few cases, which may have been due to previous treatment with antifungals.
We found that the extent of radiographic abnormality reflected the extent of endobronchial disease (as determined by bronchoscopy) in only half of the patients. However, in 44.8% of cases the extent of radiographic abnormality and bronchoscopic findings were inconsistent. Gruden reported a statistically significant relationship between the extent of tracheobronchial disease and radiographic staging13). However, he also noted that advanced KS of the lung parenchyma could be present in some patients with no visible endobronchial disease at bronchoscopy. This could explain the apparent discrepancy between radiography and bronchoscopy. Moreover, these findings are consistent with the findings of the present study. In addition, it should be noted that a normal chest radiograph in one of our PKS patients indicates that a normal chest X-ray does not rule out a diagnosis of PKS. We believe that this discrepancy may also have been due to the presence of a concomitant infectious disease, such as pulmonary tuberculosis.
Pleural effusion was noted only in 4 cases (11.4%), a significantly lower proportion than has been reported in Western countries14-16), which is similar to the level previously found in an African country (14.8%)7). This finding may mean that the existence of pleural effusion is not helpful in the differential diagnosis of PKS in Africa.
At bronchoscopy, "typical lesions" were observed in most patients (71.4%), with endobronchial disease. One series reported that a bronchoscopic biopsy in KS is dangerous, as it was found to result in significant haemorrhage in 30% of cases9), but we found that when haemorrhage occurred it was minimal and stopped fairly quickly. However, the yield of bronchoscopic biopsies was not good. Only 7 of 19 biopsies (36.8%) showed KS on histological examination, which is only slightly higher than previously reported values7, 17). Nevertheless, these biopsies are important because they may prove a diagnosis of PKS histologically in the presence of other coexisting conditions.
Acid-fast bacilli were found in 5 specimens (25%) of bronchoalveolar lavage fluid, but Pneumocystis carinii was found only in one specimen, which reflects the more frequent occurrence of Mycobacterium tuberculosis than Pneumocystis carinii as an opportunistic respiratory pathogen in Ugandans infected with HIV. It was interesting to find that Cryptosporidium, a rare respiratory pathogen, was identified in one specimen by Ziehl Neelsen staining. These results demonstrate the need for BAL given the presence of a PKS lesion.
In conclusion, the majority of PKS patients revealed no unique physical finding except mucocutaneous KS. Our study shows that palatal KS may be a strong predictor of PKS, and that radiological features may be unhelpful for evaluating the extent of PKS. In Uganda, pulmonary tuberculosis is the most common concomitant pulmonary infection in PKS patients. Therefore, BAL must be performed in all PKS patients to rule out the possibility of concomitant infection.