Complications in Transbronchial Lung Biopsy
Article information
Abstract
Transbronchial lung biopsy was performed in 68 patients with various lung diseases. As an inital diagnostic procedure in diffuse and localized lung diseases, trasbronchial lung biopsy offers an attractive alternative to open lung biopsy.
Recently imporvement in the development of medical technology has greatly facilitated this technique, but it must be kept in mind that a transbronchial lung biopsy is not without complication and sometimes potentially serious complications may occur.
This study documents the complications of transbronchial lung biopsy with 8 cases of pneumothorax (11.8%), one case of mediastinal emphysema (1.5%), 3 cases of hemorrhage (4.4%), 2 cases of cardiac arrythmia (2.9%), but none of them was fatal and they responded well with treatment.
INTRODUCTION
Since the introduction of fiberoptic bronchoscopy in 1970, its usefulness in many different situations has been documented1).
Much more of the transbronchial tree can be visualized with the aid of the fiberscope. In addition, fiberoptic bronchoscopy is considered less traumatic to the patients and less anesthesia is required. Another important advantage of fiberoptic bronchoscopy is that it can be done on patients who are on ventilators.
Reports of transbronchial lung biopsy (TBLB) using fiberoptic bronchoscopy began to appear in 1974, about lung biopsies for diffuse pulmonary diseases2).
TBLB allows one to obtain a small specimen of the lung with minimal morbidity, but it should be emphasized that TBLB is not always performed without complications. Although the experience of each investigator has been limited, the incidence of serious complication has been rarely seen3–6).
This report documents the results and comolications of TBLB done at the Veterans Administration Medical Center, affliated with University of Tennessee, in Memphis, Tennessee.
MATERIALS AND METHODS
During the 6 months between Arpil and September 1984, 235 cases of fiberoptic bronchoscopy with perfomed at the Veterans Administration Medical Center, affliated with University of Tennessee, in Memphis, Tennessee.
In 68 of 235 cases, TBLB was performed. All patients should have an empty stomach. Three medications were administered intramuscularly 30 to 60 minutes before the bronchoscopic examination: a narcotic, an anticholinergic, ad a sedative6). Morphine (10 mg) is the preferred narcotic because of its cough suppressing, pain relieving, and euphoria producing properties. Meperidine (Demerol 100 mg) would be preferred in asthamtic patients. Atropine (0.5 mg) minimizes vasovagal reflexes and oral secretions. If a patient is asthmatic, atropine 1 mg is given to block cholinergic bronchospasm. Diazepam (Valium 10 mg) provides extrasedation as well as some protection against acute convulsive reactions to the topical agents such as lidocaine.
The most frequently used topical agents are lidocaine, cocaine, and tetracaine7, 8). Tetracaine is available in an aerosolized spray as a 2 percent solution in cetacaine, and its use is usually limited to spray the mouth and pharynx.
Cocaine, which is widely used by many physicans in the U.S.A. is believed to produce the best anesthesia. The duration of action lasts for 45 to 60 minutes and the recommended dosage is 200 mg.
Lidocaine in 2 percent and 4 percent solutions is currently the most pupular agent, although it, too has definite toxicity, and its total dosage should generally be limited up to 400 mg. Its effect lasts for no more than 20 or 30 minutes.
In the pulmonary department of the University of Tennessee, 4% cocaine is therefore used for the usual patients, but in poor risk patients, only 2% lidocaine is recommended, because the effect of the drug is shorter than that of cocanine.
After topical anesthesia, the TBLB is carried out by passing the closed forceps peripherally under the fluoroscopic guidance to the area of involvement whereupon the biopsy is taken9, 10.
The pre-selected segmental bronchus, through which the foreceps is to be pased, is identified by the fluoroscops and 5 ml of epinephrine (1:20,000) is injected by a boius into this airway. Then the operator utilizes fluoroscopic ontrol to pass the biopsy forceps to the desired area.
Routinely, four 10 five specimens (occassionally up to eight) are taken.
RESULTS
Of the 68 patients entered into this study, all of them were males with mean 62 years of age, ranging from 42 to 86 years (Table 1). The patients studied here consisted of 32 whites, 31 blacks and other races, as shown in Table 2.
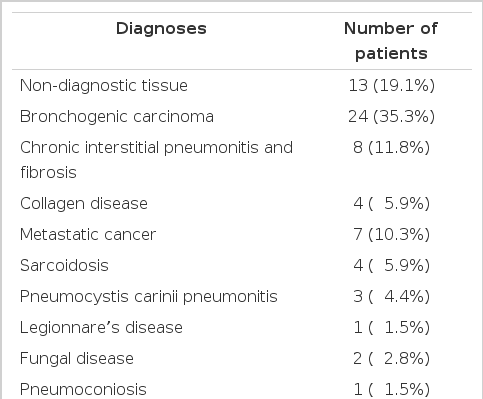
Table 3 pressents the smoking history of these patients. Diagnoses after the TBLB are listed in Table 4.
Non-diagnostic tissues were obtained in 13 cases (19.1%), including too small size of specimens. When results of the biopsy did not fit the clinical findings, open lung biopsy was recommended, if the patient cound tolerate it.
Lung cancer was the most frequent disease diagnosed with TBLB (24 cases, 35.5%) in this study. Others icnluded chronic interstitial pneumonitis and fibrosis, metastatic cancer, collagen disease, sarcoidosis, Pneumocystis carinii pneumonitis, fungal disease, legionnarre’s disease, pneumoconiosis and lipoid pneumonitis, in order. Comparing to our data in Korea, sarcoidosis is more frequent cause of diffuse pulmonary diseases.
Table 5 demonstrates that pneumothorax was the most common complication of TBLB (8 cases, 11.8%). A thoracic roentgenorgam should be obtained immediately after the procedure and again approximately 24 hours later. intraplerual suction was used for 24 to 48 hours in 5 cases (7.4%), and as a result of treatment, none was proven to be a serious problem.
Hemorrhage, estimated at greater than 50 ml, occurred in 3 cases (4.4%), which did not requrie sugery in order to control the bleeding.
There were 2 cases of cardiac arrythmia (2.9%) with premature ventricular contractions, which were successully controlled by the lidocaine infusion.
DISCUSSION
TBLB has been used for the diagnosis of pulmonary nodules and diffuse lung diseases3, 11, 12).
In 1965, 13 cases of diffuse pulmonary disease, in which lung biopsy specimens were obtained via the rigid bronchoscope, were reported11).
In 1969, Shigeto Ikeda introduced his flexible bronchoscope at the Mayo Clinic. Soonafter, pulmonologists in the U.S. were enthusiastic about its use for general diagnostic bronchoscopic procedures. Recently TBLB has been proven to be useful in the diagnosis of many different lung disease.
Fiberoptic bronchoscopy with TBLB is helpful in the diagnosis of suspected lung cancer. In case of invisible lesions, the accuracy of diagnosis can be improved to about 70% with the combination of transbronchial biopsy and transbronchial brushing under the fluoroscopic guidance9, 13, 14).
TBLB is also useful in the diagnosis of metastatic neoplasms to the lung and transbronchial biopsy and transbronchial brushing are complementary15).
Another important indication of TBLB is the diagnosis of diffuse infiltrative lung diseases. Sarcoidosis and diffuse carcinomatosis are the two main diffuse infiltrative lung diseases that can be definitely diagnosed with TBLB.
The TBLB of up to 90% of patients with sarcoidosis will demonstrate non-caseating granulomas whether or not the lungs are involved raiographically16). Other causes of diffuse pulmonary infiltrates are less readily diagnosed with TBLB because the sample is so small, and an open lung biopsy is preferred in such patients when possible17).
Since the compromised hosts frquently develop acute illness with pumonary infiltrates, the fiberoptic bronchoscopy with TBLB may be a useful procedure in these individuals. The procedure should be done as soon as possible to make the definite diagnosis of pulmonary infiltrates, if the clinical picture and sputum Gram’s stain do not suggest acute bacterial pneumonia.
The main diagnosis made with TBLB in this setting are infections (particularly Pneumocystis carinii) and neoplasms. If the results of TBLB shows only nonspecific inflammation, an open lung biopsy should be cosidered18, 19).
It should be emphasized that TBLB is not always done without complications. Most fiberoptic bronchoscopies are done with sedation and local anesthesia. The sedation with morphine, diazepam or other sedative drugs can cause respiratory depression and lead to acute respiratory failure after bronchoscopy. Also the bronchoscopy itself can lead to decreased pulmonary function20).
An acute decrease in the arterial PO2 also occurs during bronchoscopy and tends to persist for several hours21). Supplemental oxgen shoul be administered during the procedure and the patients oxygen status should be observed carefully thereafter.
Fever and pulmonary infiltrates also occur following bronchoscopy22). But most important complications of TBLB are pneumothorax and hemoptysis. This study demonstrates that pneumothorax is the most common complication of TBLB. In the 68 cases, 8 cases (11.8%) have had pneumothorax and closed thoracotomy was done in 5 cases (7.4%) of them. Cortes et al13), reported that pneumothorax occurred in 5.5% from the biopsy procedure and was the most frequent complication, and the frequency of pneumothorax could not be correlated with three technical factors; the size of the biopsy forceps, the number of biopsies obtained per procedures, and the total number of procedures performed. Fatal cases due to tension pneumothorax were reported. Any patients who develop pneumothorax should be closely observed for more than eight hours in a facility where a thoracostomy tube can be inserted immediately.
Any type of biopsy can lead to hemoptysis, and hemorrhage estimated at greater than 50 ml occurred in 3 cases (4.4%) in this study. None of them died of severe bleeding or required open thoracotomy. But fatal hemoptysis following TBLB has been reported by Zavala9). So the patients selected for TBLB should undergo screening for abnormalities of hemostasis.
Tests of prothrombin time, partial thromboplastin time, and platelet counts should be done on all patients. Also bleeding time should be determined in patients with a history of coagulopathy. Bleeding time will detect abnormalities in platelet function which are not detected by the other tests. Such abnormalities are prone to occur in uremia, hematologic malignancies, and as a consequence of drug administration24). Currently Zavala introduced the wedge method to control hemorrhage25). The procedure consists of securely lodging the tip of the fiberoptic bronchoscope into the selected distal bronchus before, during, and after TBLB.
After biopsy, the forcep is withdrawn through but the fiberoptic bronchoscope is left firmly in the place to prevent bleeding from the tracheobronchial tree. If within a minute no evidence of bleeding is seen at the tip of the bronchoscope, the instrument is withdrawn and other areas are chosen for additional biopsies. If hemorrhage occurs, the bronchoscope is kept in the wedge position for four or five minutes to allow time for a clot to form.
The cause of cardic arrythmia during fiberoptic bronchoscopy is not known. In many medical centers, the standard procedure is to monitor EKG only in high risk patients or those who have a history of cardiovascular diseases23).
In this study, the incidence of premature ventricular contractions is 2 cases (2.9%). It has been reported that acute myocardial infarction or other serious arrythmias might occur, but none was observed in our study.
Mediastinal emphysema has rarely occurred and no specific treatment is usuall required becasue the mediastinal air will be absorbed if the patient inspires high concentration of oxygen. On rare occassions, the mediastinal air can compress the veins in the mediastinum, impeding venous return and resulting in hypotension. In such cases surgical decompression of the mediastinum should be performed, usually through needle aspiration of mediastinostomy just above the suprasternal notch26).
Other potential complications are as follows; laryngospasm, bronchospasm, flooding the airway from a ruptured lung abscess and death. But in this study, there is no complication, as described above.
We have found that TBLB may be useful for a specific diagnosis in a number of different lung diseases. Although TBLB is generally considered a safe procedure, serious complications may occur.
This study resented the potentially serious complications as pneumothorax, hemorrhage, cardiac arrythmia and mediastinal emphysema. The guidelines have been established and adopted by University of Tennessee Medical Center regarding contraindications of TBLB.