Prevalence, Predictive Factor, and Clinical Significance of White-Coat Hypertension and Masked Hypertension in Korean Hypertensive patients
Article information
Abstract
Background
The prevalence and clinical significance of white-coat hypertension (WCHT) and masked hypertension (MHT) are unknown in Koreans. Here we measure the frequency of WCHT and MHT in hypertensive subjects and identify the epidemiologic and/or clinical factors that predict it in Korean subjects.
Methods
This study is a retrospective analysis of a random sample from February 2004 to October 2005. All patients had measurements of blood pressure (BP) in the clinic and 24-hour ambulatory blood pressure monitoring (ABPM). Subjects were classified into four groups on the basis of daytime ambulatory BP and clinic BP level: 1) Normotension (NT), 2) MHT, 3) WCHT, and 4) sustained hypertension (SHT).
Results
For all 967 patients, the mean clinic BP was 157.7±22.0/ 95.3±13.1 mmHg, and the mean daytime ambulatory BP was 136.4±15.0/ 86.2±10.7 mmHg. The NT, MHT, WCHT, and SHT groups consisted of 51 (5.3%), 55 (5.7%), 273 (28.2%), and 588 (60.8%) subjects, respectively. The left ventricular mass index was significantly higher in SHT than in the other groups, and was positively correlated with BP, especially ABPM. Compared with NT, the factors associated with MHT were younger age, male gender, higher BMI, clinic BP ≥130 mmHg, and alcohol consumption. Compared with SHT, the factors associated with WCHT were female gender, lower BMI, and clinic BP < 150 mmHg.
Conclusions
WCHT and MHT were prevalent in the hypertensive population. ABPM was more predictive of target organ damage than clinic BP, and could be useful in identifying subjects at risk for WCHT and MHT.
INTRODUCTION
Hypertension is a risk factor for diseases of the cardiovascular system. Mean daytime ambulatory blood pressure (BP) better reflects cardiovascular risk than mean clinic BP measured in a medical office, especially since daily fluctuations in BP reflect the actual BP to which individuals are exposed. Ambulatory blood pressure monitoring (ABPM) over 24 hours is therefore an important means of diagnosing and managing hypertension1-3). With the introduction of 24-hour ABPM, conventional hypertension has been subclassified as white-coat hypertension (WCHT), in which patients exhibit elevated clinic BP but normal daytime ambulatory BP; masked hypertension (MHT), in which patients exhibit elevated daytime ambulatory BP but normal clinic BP; and sustained hypertension (SHT), in which patients exhibit elevated clinic and daytime ambulatory BP4, 5).
WCHT is present in about 7% to 12% of the general population, and in 12% to 50% among stage 1 and 2 hypertension groups by the JNC-6 guidelines6-8). Factors predictive of WCHT include female gender, low educational level, low clinic BP, smoking history, and low BMI6, 7, 9, 10). The degree of target organ damage11-15) and long-term cardiovascular risk11, 16-18) in WCHT patients is higher than normotensive (NT) subjects, but less than in subjects with SHT.
MHT is present in about 10% of patients with hypertension2, 7, 8, 19). Factors predictive of MHT include younger age, male gender, high BMI, high clinic BP, and a history of habitual drinking7, 20). Target organ damage and cardiovascular risk in subjects with MHT are similar or slightly lower than those of SHT8, 19, 21).
While measurement of ambulatory BP for 24 hours is essential to the diagnosis of WCHT or MHT, these conditions are not easy to diagnose in Korea, because measurements of daytime ambulatory BP are not yet common. Accordingly, we assessed the prevalence of WCHT and MHT in hypertensive patients who were followed-up with an ABPM device. We also determined the dynamic, demographic, and clinical factors predictive of WCHT and MHT, as well as their effects on target organ damage, in Korean subjects.
MATERIALS AND METHODS
Subjects
The subjects of this study were hypertensive patients ≥15 years old at an early stage of diagnosis who visited the outpatient unit of the Department of Cardiology at Asan Medical Center between February 2004 and October 2005, and who had undergone 24 hours of ABPM. Subjects with serious cardiovascular complications, such as coronary artery disease and stroke, at their first visit were excluded.
Methods
Demographic characteristics recorded at the first visit included age, sex, height, weight, medication, smoking history, drinking history, combined diseases, and a family history of hypertension. Blood was drawn for measurement of total serum cholesterol, triglycerides, HDL and LDL cholesterol, blood sugar, creatinine, and uric acid. Echocardiographic exams were done, depending on the doctor's decision, to obtain the left ventricular mass index (LVMI) and aortoseptal angle (AoSA). LVMI was calculated by dividing the left ventricular muscles by surface area22), and AoSA was measured from the parasternal long-axis view immediately before the opening of the aortic valve, with AoSA increases defined as over 12023).
Clinic BP and 24-hour ABPM were measured using standard procedures. If subjects were taking antihypertensive medications, they were stopped for 3 to 7 days prior to measurements of clinic BP and 24-hour ABPM. Based on mean daytime blood pressure (6 am to 10 pm) of clinic BP and 24-hour ABPM, subjects were classified into four groups4, 5).
(1) Normotension (NT)
Clinic BP < 140/90 mmHg and daytime BP < 135/85 mmHg
(2) Masked hypertension (MHT)
Clinic BP < 140/90 mmHg and daytime BP ≥ 135 mmHg or 85 mmHg
(3) White-coat hypertension (WCHT)
Clinic BP ≥ 140 or 90 mmHg and daytime BP < 135/85 mmHg
(4) Sustained hypertension (SHT)
Clinic BP ≥ 140 or 90 mmHg and daytime BP ≥135 mmHg or 85 mmHg
Statistical Methods
Continuous variables are represented as mean standard deviation, and categorical variables as frequency and percentage. Pearson's correlation coefficient analysis was used to assess correlations between blood pressure and LVMI. The NT and MHT groups, and the SHT and WCHT were compared using chi-square tests for categorical variables and Student's t-test for continuous variables. Multivariate logistic regression analysis was used to determine whether any baseline demographic or clinical factors were predictive of MHT and WCHT. All statistical analyses were performed using SPSS 12.0 for Windows. A p-value < 0.05 was defined as statistically significant.
RESULTS
Baseline characteristics
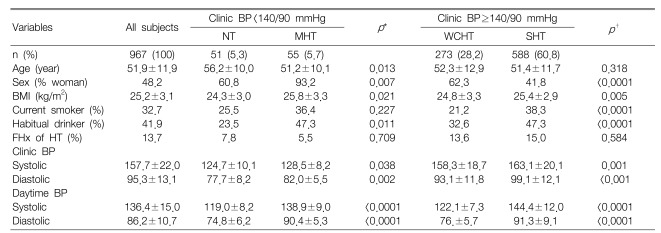
The mean age of the 967 subjects was 51.9±11.9 years. Of these individuals, 52% were male, 32% were current smokers, and 41.9% were habitual drinkers. In addition, 87.1% (886) were taking one or more antihypertensive medications, and 13.7% had a family history of hypertension. Overall, the mean clinic BP was 157.7±22.0/95.3±13.1 mmHg, and the mean daytime ambulatory BP was 136.4±15.0/ 86.2±10.7 mmHg. The NT, MHT, WCHT, and SHT groups consisted of 51 (5.3%), 55 (5.7%), 273 (28.2%), and 588 (60.8%) subjects, respectively (Table 1).
Compared with the NT group, the MHT group had a lower mean age, higher mean body mass index, and higher percentages of males and habitual drinkers (p<0.05 each). In contrast, the WCHT group had a higher percentage of females, a lower mean body mass index, and lower percentages of current smokers and habitual drinkers than the SHT group (p<0.05 each).
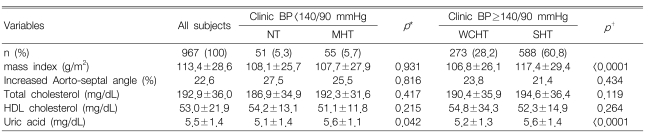
Echocardiographic Findings
The SHT group had a significantly higher LVMI than the WCHT group (p<0.05), but LVMI was not significantly different in the NT and MHT groups. LVMI showed significant positive correlations with both cli0nic BP (r=0.305, p<0.001) and mean daytime ambulatory BP (r=0.175, p<0.001) (Figure 1). There were no significant differences in the percentage of patients with increased AoSA.
'Masked Effect' and 'White Coat Effect'
There were significant negative correlations between clinic BP and mean daytime ambulatory BP minus clinic BP (awake ABPM-clinic BP) for both systolic (r=-0.8, p<0.001) and diastolic (r=-0.6, p<0.001) blood pressure. The white-coat effect was clear among the subjects who exhibited high clinic BP, while the masked effect was clear among subjects who exhibited low clinic BP.
Predictive Factors
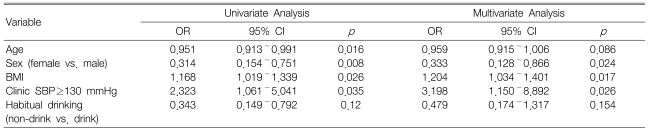
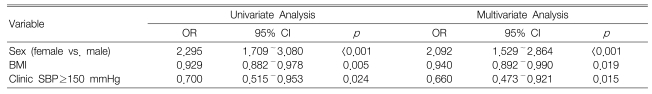
We used univariate logistic regression analysis to identify predictive factors for MHT and WCHT. Factors predictive of MHT included younger age, male gender, higher body mass index, clinic BP ≥130 mmHg that did not meet hypertension criteria, and habitual drinking (Table 3). Factors predictive of WCHT included female gender, lower body mass index, and clinic BP that met the hypertension criteria but <150 mmHg (Table 4). Multivariate logistic regression analysis showed that factors significantly predictive of MHT were male gender, higher body mass index, and clinic BP ≥130 mmHg, and that factors significantly predictive of WCHT were female gender, lower body mass index, and clinic BP <150 mmHg.
DISCUSSION
Large-scale studies in western countries on WCHT and MHT have led to JNC-7 and ESC-ESH guidelines recommending the use of ABPM for 24 hours24-26). However, ABPM is not widely used in Korea, and their prevalence is not known. Here, we assessed 24-hour ABPM in almost 1000 Korean subjects to determine the prevalence of both WCHT and MHT.
Cardiovascular risk is considerably reduced if mean daytime blood pressure, determined by ABPM, is lower than 135/85 mmHg, establishing this as the normal upper limit of ABPM10, 26-29). However, many previous studies defined it as under 125/80 mmHg, leading to differences in estimates of WCHT prevalence: from around 10% in the general population and 15% to 50% among those with slightly elevated blood pressure. Its prevalence among Koreans with early stage hypertension was 28.2%, perhaps due to the fact that they were mildly hypertensive patients.
MHT, previously called 'white-coat normotension' or 'reversed WCHT', was first described as a phenomenon of normal clinic BP and high daytime ambulatory BP4, 30). Its prevalence ranges from 9% to 13.4% in the general population8, 19) and from 7% to 22.9% in hypertensive patients2, 7). The prevalence of MHT observed in this study was somewhat lower, 5.7%, probably because fewer young patients were included in the study, and therefore may not reflect primary medical practice. Furthermore, since this was not a random prospective study, we cannot exclude the possibility that MHT patients with normal clinic BP were no longer followed-up.
LVMI correlates significantly with 24-hour daytime ambulatory BP in hypertensive subjects31), and 24-hour daytime ambulatory BP better reflects cardiovascular risk than clinic BP2, 3). We also found significant correlations between 24-hour daytime ambulatory BP and echocardiographically-determined LV hypertrophy and LVMI. In contrast to previous studies13, 15, 19), however, we did not detect clear differences among the four blood pressure groups. This may have been due to the relatively low number of patients in each group, although we cannot exclude the possibility that LV hypertrophy in some patients was affected by their past medication history. It should be noted, however, that all of our subjects were recently diagnosed. Prospective studies in large numbers of subjects are needed to determine causal relationships between BP and LV hypertrophy, as well as to determine if target organ damage affects long-term prognosis.
While the percentage of patients with AoSA increases significantly with age, there were no significant differences among the four blood pressure groups, perhaps because we did not measure the exact angle.
We also assessed factors that could distinguish between NT and MHT or between WCHT and SHT, which cannot be differentiated by clinic BP. In agreement with previous studies6, 7, 9, 10, 20), we found that factors significantly predictive of MHT were younger age, male gender, higher body mass index, and clinic BP ≥130 mmHg, while the factors significantly predictive of WCHT were female gender, lower body mass index, and hypertensive clinic BP <150 mmHg. Nicotine-induced hyperfunction of the sympathetic nerve caused by smoking contracts the peripheral vascular system and raises BP for about 30 minutes32, 33). Since continual smoking raises daytime ambulatory BP and since subjects may temporarily stop smoking before visiting the clinic, measured clinic BP may be lower than daytime ambulatory BP. Thus, a previous study reported that smoking is predictive of MHT, whereas not smoking is predictive of WCHT9). Although we found that smoking status was not predictive of WCHT or MHT, smoking may distinguish among hypertensive groups because the percentage of smokers in the WCHT group was significantly lower than that in the SHT group.
Whereas some studies measured clinic BP two to three times per subject and averaged these values7, 8), we measured clinic BP only once. Our procedure may have introduced an error in the diagnosis of WCHT by failing to reduce the white coat effect. Furthermore, the ABPM effect, in which average blood pressure increased 7/4 mmHg for the first four hours after wearing an ABPM device34), could cause errors in diagnosis. Therefore, randomized, prospective studies, in which clinic BP is determined by measuring BP twice for each of three visits35), and in which daytime ambulatory BP is determined by performing ABPM for 48 hours and taking the results for the second day, may more accurately determine the correlations among prevalence rates of MHT and WCHT, target organ damage, and cardiovascular risk.
In conclusion, we found that the prevalence rates of WCHT and MHT among Korean hypertensive patients were similar to those in western countries. ABPM is essential for diagnosing such patients, and better reflects target organ damage such as LV hypertrophy. These findings indicate that ABPM should be used to determine factors predictive of WCHT and MHT, thus enabling early detection of high risk patients and providing them with proper treatment.