Sexuality and Quality of Life after Hematopoietic Stem Cell Transplantation
Article information
Abstract
Background
The quality of sexuality is significantly affected by physical changes following hematopoietic stem cell transplantation (HSCT) and the dissatisfied and/or dysfunctional sexuality may cause deterioration in the quality of life (QOL).
Methods
With two models of questionnaires, we interviewed thirty-eight patients who remained in the disease-free status after HSCT and had sex partners, to assess: 1) the changes in sexuality, 2) QOL in physical, psychological, social and spiritual domains and 3) the correlation between sexuality and QOL.
Results
The common physical changes that may affect sexuality in women were secondary amenorrhea (69.2%), loss of sexual interest (53.8%), diminished vaginal secretion (50%), menopausal syndrome (34.6%), dyspareunia (30.8%) and failure to orgasm (23.1%), while men complained of impotence (41.7%) and difficulty in ejaculation (16.7%). For sexuality, satisfaction of sexual activity, attainment of orgasm and frequency of intercourse decreased significantly after HSCT as compared with the pre-transpiant levels. A score measuring QOL after HSCT marked 5.91 on a full score of 10; social domain ranked the lowest (5.01) while physical domain the highest (6.70). Among the items of sexuality, only sexual desire was significantly correlated with QOL: satisfaction, orgasm and frequency were not significantly correlated with QOL.
Conclusion
Although sexuality is affected by the physical changes following HSCT, we should not overlook the psychological and social effects on the sexuality of post-transplant patients. Therefore, educational and counseling programs are very important to restore and improve their sexuality.
INTRODUCTION
Many patients experience significant physical changes that may affect sexuality and disturbances in sexual activities following hematopoietic stem cell transplantation (HSCT). Here, sexuality is defined as possession of sexual power or capability of sexual feelings.
In general, cancer patients suffer from the treatment of cancer as well as from the cancer itself, which results in a decrease in physical, psychological or social functions. In addition, sexuality can be impaired. Andersen quoted that the emotional unsteadiness of cancer patients, resulting from anxiety or depression, affected their sexuality1). In fact, the quality of sexuality was significantly affected by physical changes following HSCT and about one fifth of the patients were sexually dissatisfied2). Gonadal dysfunction is closely associated with high-dose chemotherapy and total body irradiation (TBI). The majority of patients receiving high-dose cyclophosphamide with high-dose busulfan or TBI were reported to have permanent defects in ovaries or testicles3, 4). Sexual dysfunction was more significant in women than in men5). More importantly, the dissatisfied and/or dysfunctional sexuality may cause deterioration in the quality of life (QOL).
Ferrell at al proposed a model illustrating the impact of HSCT on the QOL domains, which consisted of physical well-being, psychological well-being, social well-being and spiritual well-being6). Here, social well-being is influenced by the problems of affection or sexual function.
We conducted a study to determine whether the changes in sexuality were closely correlated with QOL in patients who underwent HSCT. For those who underwent HSCT, we conducted this study to assess: 1) the changes in sexuality in terms of satisfaction, orgasm, sexual desire and frequency, 2) QOL in physical, psychological, social and spiritual domains and 3) the correlation between sexuality and QOL. These data will be important for improving the rehabilitation of patients following HSCT, as well as to provide them with comprehensive care and counseling.
MATERIALS AND METHODS
Patients
Among one hundred and fourteen patients who underwent HSCT at Samsung Medical Center between February 1996 and December 1999, fifty patients who had sex partners and remained in the disease-free status were invited to participate in the study. Thirty-eight patients out of fifty participated in this study. In February 2000, each of them was interviewed by an oncology nurse during the regularly scheduled follow-up visits after HSCT with completion of self-administered questionnaires. At the time of interview, the period after transplantation ranged from 2 months to 46 months post-HSCT and all patients were Korean and 28 years or older.
Questionnaires
A questionnaire of 27 questions, which was originally developed by Kim for the study of sexuality in patients with cervix cancer with regard to the level of satisfaction, frequency of orgasm, level of sexual desire, frequency of intercourse and difficulty in sexual activity, was used for our study of sexuality7); however, it was modified in a few aspects by our team to suit the post-HSCT patients.
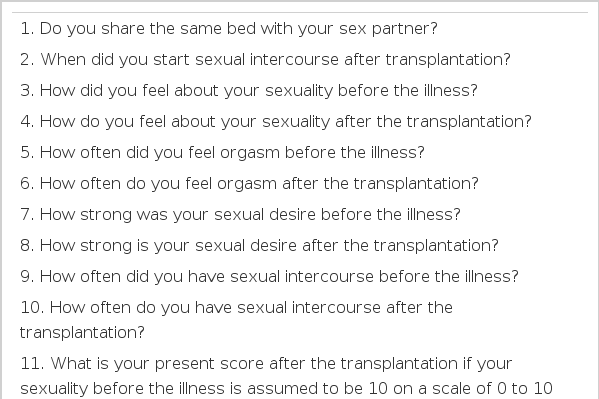
Our modified questionnaire consisted of 9 items that are related to demographic, disease and treatment characteristics and 15 items that are related to sexuality. The items of the patients’ characteristics included sex, age, marital status, religious status, level of education, occupation, diagnosis of underlying disease, type of transplantation and interval between transplantation and study. The items related to sexuality are presented in Table 1.
To measure QOL of the patients, we used the questionnaire developed by Ferrell et al, which consists of 41 items in terms of physical (8 items), psychological (18 items), social (8 items) and spiritual (7 items) domains8). Each domain was scored on a scale of 0 to 10: the worst being 0 and the best being 10. A measure of reliability was computation of internal consistency using Cronbach’s alpha coefficient as a measure of agreement between the items and subscale: an overall score of r=0.95.
Statistical Analysis
The data were described with a frequency, percentile, mean and standard deviation. The changes in sexuality pre- and post-HSCT were analyzed using paired t-test. Pearson’s correlation analysis was applied to investigate the correlation between sexuality and QOL. The statistical significance was presented by P-value for each analysis. The data were analyzed using SPSS 10.0.
RESULTS
Patient Characteristics
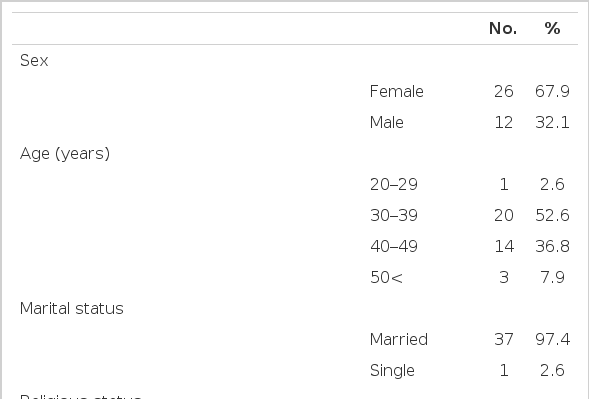
Table 2 lists the demographic, disease and treatment characteristics of the 38 participants. All participants were Korean and their average age was 39 years (range, 28 to 57 years). The ratio of male to female was about 1:2. All but one was married at the time of the interview. Acute myeloid leukemia was the most common disease among the participants and other diseases included aplastic anemia, chronic myelogenous leukemia etc. The mean interval between transplantation and this study was 11.2 months (range, 2 to 46 months post -HSCT).
Physical Changes after HSCT and Changes in Sexuality
Table 3 lists the common physical changes of 26 female and 12 male participants resulting from HSCT. It was noted that a significant fraction of the participants had no changes (15.4% of females and 33.3% of males).
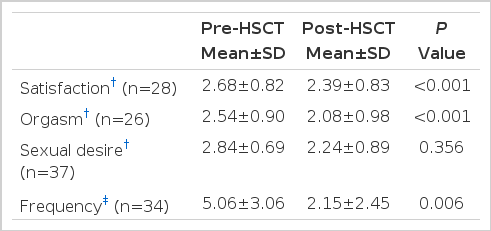
Satisfaction of sexual activity, attainment of orgasm, sexual desire and frequency of intercourse were compared between the pre-HSCT and post-HSCT to assess the qualitative aspects of sexuality (Table 4). The levels of all aspects, except sexual desire, significantly decreased after HSCT (p<0.05, respectively).
Patients (13/38, 34.2%), their spouses (8/38, 21.1%), or both (8/32, 21.1%) avoided sexual contact after HSCT. Twenty-two out of 26 female participants (22/26, 84.6%) ascribed the avoidance of sexual contact to fatigue (15/22, 68.2%), decreased sexual desire (11/22, 50.0%), anxiety about infection caused by sex (8/22, 36.4%), diminished vaginal secretion (6/22, 27.3%), change of appearance (4/22, 18.2 %), anxiety about bleeding (4/22, 18.2%), dyspareunia (3/22, 13.6%), weakness (3/22, 13.6%) and 7 other causes (7/22, 31.8%); while 8 out of 12 male participants (8/12, 66.7%) avoided sexual contact due to anxiety about infection caused by sex (4/8, 50.0%), fatigue (3/8, 37.5%), difficulty in erection (3/8, 37.5%) and 6 other causes (6/8, 75.0%).
Quality of Life
From the results of the questionnaire for QOL on a scale of 0 to 10, the average score was 5.91 (range, 3.75 to 7.43) with 6.70 for physical domain, 5.40 for psychological domain, 5.01 for social domain and 6.67 for spiritual domain (Table 5).
DISCUSSION
This study was conducted to evaluate the changes in sexuality, QOL and the correlation between sexuality and QOL in patients who underwent HSCT.
In our study, female participants reported secondary amenorrhea, loss of sexual interest, diminished vaginal secretion, menopausal syndrome, dyspareunia and failure of orgasm in descending order while male participants reported impotence and difficulty in ejaculation. Men reported fewer physical changes than women. Sanders et al. reported that the physical changes following a transplant were closely related to gonadal dysfunction, which resulted from the damage of gonads by conditioning regimens3, 4).
When we compared satisfaction of sexual activity, attainment of orgasm, sexual desire and frequency of intercourse between pre-HSCT and post-HSCT to assess the qualitative aspects of sexuality, the levels of all aspects, except sexual desire, significantly decreased after transplantation. According to the study done by Syrjala et al. the changes in sexuality, for women, persist even on the 3rd year if they are not prevented or resolved by 1 year post-HSCT5). In contrast, some of the men recover their sexual function as time elapsed. Wingard et al found, from a mailed survey for 126 post-HSCT adult survivors, that sexual satisfaction correlated with the serum levels of estrogen in women and testosterone in men2). Impotence and decreased libido can be early symptoms of hyperprolactinemia that is related to the inhibition of gonadotropin-releasing-hormone secretion by the elevated prolactin levels and some degree of antagonism by prolactin to the peripheral action of testosterone9). Impotence is also associated with hyperthyroidism and hypothyroidism. In addition, decreased sexual frequency and satisfaction were closely associated with greater psychological distress and decreased energy10). Syrjala et al found that females experienced more sexual problems following HSCT than males (80% vs. 29%) and there were no significant pre-HSCT variables predicting sexual satisfaction for females while older age, poorer psychological function, unmarried life and lower sexual satisfaction predicted sexual dissatisfaction for males5).
We found that men and women commonly listed anxiety about contracting infection from sex and fatigue as the main causes of avoiding sexual contact following HSCT. It is certainly necessary for health care givers to recognize these issues of sexual activity and therefore educate and counsel these patients to correctly understand sexuality post-HSCT and solve problems associated with sexuality. In this study, patients (13/38, 34.2%), their spouses (8/38, 21.1%), or both (8/32, 21.1%) avoided sexual contact as a solution for dissatisfied sexuality. For this reason, their spouses need education and counseling as well.
In our study, a score measuring the quality of life after HSCT marked 5.91 on a scale of 0 to 10. Among the domains on the survey, social domain ranked the lowest (5.01) while physical domain the highest (6.70). This could be interpreted as meaning that it is hard for these patients to recover personal relationship, including sexuality, on time. Ferrell et al reported that family distress and sexuality had the most negative influences on the social well-being subscale for long-term cancer survivors8). When various indices of physical and psychosocial status were compared between pre-BMT and one-year follow-up, the only significant differences were sexual relationship and vigor subscales11).
When it came to the correlation between sexuality and QOL, only sexual desire was significantly correlated with the overall QOL. Sexual satisfaction had a tendency to correlate with the overall QOL (p=0.071). Sexuality failed to show any correlation with the social domain of QOL, which is supposed to be influenced by sexuality in a model depicting the impact of BMT on QOL by Ferrell6).
Educational, behavioral and mechanical interventions could be offered to patients with sexual problems to improve their QOL associated with sexuality. In fact, it was found that brief sexual information made a substantial improvement in sexual activity for women who survived from cancer12). important information to help patients recover to the acceptable level of sexuality.
It is recommended that a study be done in a prospective manner with a large sample size to define the correlation between sexuality and QOL after HSCT. Based on that, it is necessary to develop educational and counseling programs for patients following HSCT.
Acknowledgments
We thank Seon Woo Kim, Ph.D. at Samsung Biomedical Research Institute for the statistical analysis, Meen Jong Lee and So Yeon Seol for assistance in manuscript preparation.