A Case of Rathke’s Cleft Cyst Inflammation Presenting with Diabetes Insipidus
Article information
Abstract
Rathke’s Cleft Cyst(RCC), which is located at the intrasellar region, is considered to be the distended remnants of Rathke’s pouch, an invagination of the stomodeum. Lined with columnar or cuboidal epithelium of ectodermal origin, RCC usually contains mucoid material and it is found in 13–22% of normal pituitary glands. The cyst rarely leads to the development of symptoms but, when it does, the most common presenting symptoms are headache, visual impairment, hypopituitarism and hypothalamic dysfunction. However, in some cases it presents symptoms of diabetes insipidus, decreased libido and impotence. Recently we experienced a case of RCC inflammation presenting with diabetes insipidus and treated with transsphenoidal surgery. To our knowledge, this is the first report of RCC presenting with symptoms of diabetes insipidus in Korea.
INTRODUCTION
Rathke’s Cleft Cyst (RCC) is considered to be distended remnants of Rathke’s pouch, an invagination of the stomodeum. RCC is found in 13–22% of normal pituitary glands1, 2). It is an intrasellar cyst lined with cuboidal or columnar epithelium containing mucoid material2–5). RCC is usually asymptomatic2, 3, 5). A few cases with symptomatic RCC have a female preponderance, occurring between 40 to 50 years of age. Commonly, presenting symptoms are related to mass effect, such as headache, visual impairment and hypopituitarism. However, those presenting only diabetes insipidus are uncommon1–6). We experienced a case of symptomatic RCC with inflammation presenting feature of diabetes insipidus.
CASE REPORT
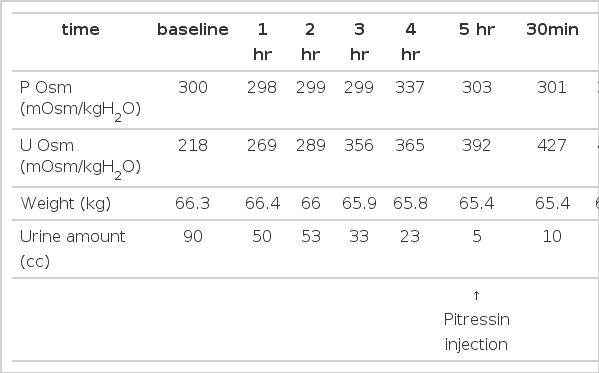
A 69-year-old female housewife complained of a sudden onset of dry mouth, polyuria and polydypsia two months prior to admission. She had been in good health and had no particular medical history. Two months ago, she developed abdominal pain, loose stool, general weakness, malaise, nausea, dry mouth and polyuria. On admission, neurologic examination was done but no particular pathologic findings, including visual field defect, were observed. On admission, she showed chronic ill-looking appearance, a dehydrated tongue and dry skin. Urine volume was 3500–4500 mL a day and urinalysis showed a specific gravity of 1.005, urine osmolarity 227 mOsm/kgH2O, Na 101 mmol/L, K 10 mmol/L and Cl 84 mmol/L. Plasma osmolarity showed 294 mOsm/kgH2O, Na 146 mmol/L, K 3.3 mmol/L and Cl 111 mmol/L. We performed an endocrinological study. The study demonstrated partial hypopituitarism (serum cortisol 1.33 μg/dL, ACTH 16.86 pg/mL, total T3 58.8 ng/mL, total T4 4.8 μg/dL, TSH 0.24 mlU/mL, LH 1.38 mlU/mL, FSH 0.24 mlU/mL, ADH 1.28 ng/mL). Anterior pituitary function was investigated with a set of three tests with insulin tolerance, TRH and LHRH. Cortisol, TSH, FSH and LH responses were compromised, while prolactin responses were retained (Table 1). Plain skull X-ray film of the sella was normal (Figure 1). Magnetic resonance image (MRI) scan showed isodense signal intensity mass lesion in pituitary fossa with infundibular thickening and no enhancement of RCC with dynamic study was observed (Figure 2). As the patient presented polyuria, mild headache and hypoosmolar urine, a water deprivation test was done, revealing a pattern of partial central diabetes insipidus (Table 2). In order to obtain an exact diagnosis, surgery was performed via the transsphenoidal approach. Yellow-colored discharge flowed from the cystic lesion when the anterior pituitary was incised. Cyst drainage and wall biopsy were done. The histopathological examination showed mixed inflammatory cell infiltration in the loose connective tive tissue stroma. Leukocyte common antigen (LCA)-positive lymphocytes were detected. Focally remained columnar epithelial walls were noted and cytokeratin immunohistochemical staining revealed monolayered columnar epithelium in the cyst wall (Figure 3, 4). These findings were compatible with Rathke’s cleft cyst inflammation. After operation, the patient was given a physiologic dose of prednisolone, thyroid hormone and desmopressin nasal spray. Polyuric symptoms disappeared with this regimen. Five months later, desmopressin replacement was stopped and no more polyuric symptoms have developed.

Pituitary fossa MRI show isodense signal intensity mass occupying the pituitary fossa and infundibular thickening.
DISCUSSION
RCC arises from the remnants of Rathke’s pouch, an invagination of the stomodeum formed by the fourth gestational week2, 3, 7). Normally, Rathke’s pouch is closed off by proliferation of the anterior and posterior lobe of the pituitary gland, and this lumen forms a thin residual cleft in the gland. The resulting cleft persists as a cyst lined with columnar or cuboidal epithelium of ectodermal origin. Failure of obliteration of Rathke’s cleft with proliferation of the lining cells and accumulation of secretions may result in cyst formation between anterior and middle lobes2, 3). Voelker et al. reviewed 155 cases of RCC saying that RCC is usually asymptomatic and found in 13–22% of normal pituitary glands in autopsy8). RCC is an intrasellar cyst containing mucoid material. RCC shows few symptoms with the size of less than 1 cm. However, when it grows more than 1 cm2–5, 9) or inflammatory changes develop, various symptoms may occur, especially when it expands to the infundibular portion and suprasellar region2–5, 9, 10). Most common presenting symptoms are headache, visual disturbance, hypopituitarism and hypothalamic dysfunction. However, a few cases reported decreased libido, impotence and diabetes insipidus2, 10). Mechanical compression of the pituitary gland by the cyst, as well as inflammation itself, may play a major role in causing pituitary dysfunction in RCC patients9). Lymphoplasmatic inflammation induced by mucus secreted by goblet cells of the cyst wall leads to inflammatory changes of RCC and leakage of cyst contents into the pituitary gland can occur, possibly leading to the development of abscess formation9, 11, 12). Voelker et al. and Ross et al. reported hypopituitarism in 39% and 12% of patients, respectively6, 8). But some authors reported 100% incidence of hypopituitarism9). Thus, subclinical RCC presenting no specific symptom may occur frequently. Eguchi et al. said that RCC greater than 1 cm which develops symptomatic hypopituitarism involving more than two hormones should be treated with a surgical approach as the general recommendation9). The most frequent cases involve hyperprolactinemia, followed by gonadotropin deficiency, pan-hypopituitarism, hypothyroidism and hypocortisolism2). Our case exhibited hypopituitarism without prolactin deficiency. Its size was more than 1.5 cm. It showed isodense intensity on T1-weighted image on MRI. Usually RCC shows hypodense. intensity on T1-weighted image but inflammatory change could be shown as isodense or hyperdense intensity like our case4). Incision of the cyst was made, yellowish pus-like aspirates flowed from the cyst. Accordingly, RCC inflammation and abscess formation were suspected. Biopsy findings revealed mixed inflammatory cell infiltration in the loose connective tissue stroma and focally remained cyst wall composed of columnar epithelium. Cytokeratin immunohistochemical staining revealed monolayered columnar epithelium in the cyst wall. RCC presenting with diabetes insipidus is rare2, 3, 9). Diabetes insipidus is thought to be a result from stalk impairment4). El-Mahdy et al. reports 28 cases of symptomatic RCC treated by transsphenoidal operation and only one of those cases (3.6%) presents diabetes insipidus, while 4 patients (14.3%) suffered preoperatively from diabetes insipidus2). It is important to differentiate RCC from other neoplastic lesions, such as craniopharyngioma and pituitary adenoma1, 3, 4, 13). Differentiation from pituitary adenoma is important as it is very difficult to distinguish RCC from pituitary adenoma3). Preoperative diagnosis in most reported cases were pituitary adenoma. The widening of sella turcica was the common point of differentiation in many cases of pituitary adenoma in simple skull image3). Yoshida et al. reported that the mean age of the patients was 38 years old, and the highest frequency was in the fifth decade with marked female preponderance7). Endocrinological presentation of RCC, such as amenorrhea, is thought to be the major cause of marked female preponderance2, 9). With the advent of MRI, asymptomatic or subclinical RCCs are now being detected with increasing regularity. Simple drainage and partial excision of the cyst wall is the treatment of choice1–5, 9). Wide removal of the cyst wall should be avoided because of possible damage to the hypothalamus, pituitary, optic nerves and optic chiasm1). Transsphenoidal surgery is preferred because there is danger of damage to the hypothalamus and optic apparatus1–5, 9). Surgical treatment is generally recommended even when the patient has mild symptoms or signs such as headache, mild defect of visual field, increased prolactin or a cyst size of more than 10 mm9). Patients with small-sized RCC, or even asymptomatic, should be followed up regularly with an MRI. Systematic endoclinological examination is recommended once a year9). Generally, the prognosis after a partial removal of the cyst wall or simple aspiration of the cyst seems to be good even though the cyst recurs2, 3).