Clinical findings of the patients with legal pulmonary disability - Short-term follow-up at a tertiary university hospital in Korea
Article information
Abstract
Background/Aims
Legal pulmonary disability in Korea is decided for chronic respiratory patients who have been diagnosed for a year or more, and the patients haven't gotten better after more than 2 months of sufficient treatment and they have shown no change in their pulmonary function within the two years after their original diagnosis. The purpose of this study was to investigate the clinical features and progress of those patients who have been diagnosed as having pulmonary disability.
Methods
We reviewed retrospectively the medical records of the patients who had been decided as having pulmonary disability at a tertiary university hospital from 2003 to 2004, and these patients could be followed up for more than 6 months.
Results
The number of enrolled patients was 118 (male : female = 95 : 23) and their mean age was 60±10 years. Their major underlying diseases were chronic obstructive pulmonary disease (n=45, 38%), tuberculous destroyed lung (n=29, 25%), and bronchial asthma (n=27, 23%). Of them, the number of patients with a class 1 pulmonary disability were 24 (20%), there were 28 class 2 patients (24%) and 66 class 3 patients (56%). The FEV1 could be followed up for 42 of these patients, of whom 20 patients showed no change or a decrease in their FEV1 but 22 showed an increased FEV1. Especially, some of them showed the increase of their FEV1 of 10% or more, and the 50% of them were patients with bronchial asthma. During the follow-up period, 6 patients died; 3 were class 1, 1 was class 2 and 2 were class 3. Five of these patients died of their underlying pulmonary diseases or combined pneumonia.
Conclusion
It is necessary to decide the pulmonary disability after sufficient treatment and to perform periodic follow-up testing even after the disability decision for confirming that the disability is stable and also to adjust the class of the disability. Further studies are needed to observe the clinical progress and prognosis of patients with pulmonary disability by performing long-term follow-up for a large number of patients.
INTRODUCTION
Legal pulmonary disability is a newly registered disability in Korea according to the Handicapped-person Welfare Law that was revised and enacted on July 1, 2003. It is confined to those people with a chronic, severe respiratory disorder that creates a restriction or a lack of ability to perform an activity.
In 1980, the World Health Organization (WHO) announced 'Three international classifications of impairments, disabilities and handicaps (ICIDH)', which defined impairment as any loss or abnormality of psychological, physiological or anatomical structure or function. The disability is any restriction or lack of ability that is caused by an impaired ability to perform an activity in the manner or within the range considered normal for a human being, and a handicap is a disadvantage for a given individual that caused by an impairment or a disability that limits or prevents the fulfillment of a role that is normal for that individual1).
Respiratory impairment can be objectively measured through several tests such as spirometry, measuring the carbon monoxide diffusing capacity (DLco), the arterial blood gas analysis (ABGA) and the pulmonary exercise test. Some additional tests may be required according to the underlying diseases. For example, for the patient with bronchial asthma, a methacholine bronchoprovocation test or a bronchodilator response test is necessary2).
The American thoracic Society (ATS) has defined impairment as a purely a medical condition, whereas disability indicates the total effect of impairment on a patient's life. All this is affected by such diverse factors as age, gender, education, the economic and social environment and the energy requirements of an occupation. This definition can be said to include the handicaps suggested by WHO2-4).
For the pulmonary disability, the ATS has announced the diagnostic criteria of the disability based on the pulmonary function test (PFT) in 1982 and 19863-5). Moreover, the criteria suggested by the American Medical Association in 2001 were also used6).
In Korea, the diagnostic criteria are specified in the Handicapped-person Welfare Law enacted in 2003. A pulmonary disability can be diagnosed when the duration of the disease is more than one year and the impairment of the pulmonary function is fixed even after 2 or more months of treatment, and there is a decrease of the forced expiratory volume for 1 second (FEV1) on the PFT or there is hypoxemia on the ABGA at a resting state, as well as dyspnea is present. The grade of pulmonary disability can be decided into three classes.
Only two indices, that is, the FEV1 and the partial pressure of oxygen in arterial blood (PaO2), are used to evaluate pulmonary disability in Korea. However, there is no report on what kinds of pulmonary diseases could be determined to be pulmonary disability with using these two indices, what their clinical features are and how the progress of disease and the prognosis would go according to the three classes of pulmonary disability. The objectives of this study were to investigate the clinical features and progress of those patients who have been diagnosed with pulmonary disability in our hospital and they could be followed up for more than 6 months.
MATERIALS AND METHODS
The medical records and radiologic findings were analyzed retrospectively for the patients who had been diagnosed with respiratory disability at Gachon University Gil medical center from July 2003 to October 2004 and they could be followed up for more than 6 months.
The decision for diagnosing pulmonary disability was made according to the implementing regulation of the Handicapped-person Welfare Law enacted in 2003. The standards are as follows: the disability has to be judged by pulmonary subspecialists, and more than a year had elapsed since the first diagnosis as related with the present state, and the disability is fixed enough to show no improvement even after continuous treatment of 2 months or more. The criteria for the diagnosis are (1) the pulmonary disability persists in spite of sufficient medical treatment, (2) before the disability decision is made, there should be objective testing for the patient through ① the decision on the degree of dyspnea, ② the chest radiography, ③ the PFT, ④ and the ABGA. In addition, if necessary, computerized tomography (CT) of the chest, bronchoscopy, pulmonary exercise testing, ventilation-perfusion scanning of the lungs and pulmonary arteriography should be done for a more accurate diagnosis according to the diseases, (3) of the repetitive test results for more than 2 months, the lowest level is chosen to represent the disease.
Through the above standards, the grade class of the pulmonary disability is decided as follows:
Pulmonary Disability Class 1 - Those who feel the dyspnea, even while resting, enough to receive oxygen treatment due to the chronic respiratory insufficiency, and whose FEV1 is lower than 25% of the predicted value in the resting state or the PaO2 without an oxygen supply is lower than 55 mmHg in the stable state of disease.
Pulmonary Disability Class 2 - Those who feel dyspnea even while moving in the house due to chronic respiratory insufficiency, and whose FEV1 is lower than 30% of the predicted value in the resting state or the PaO2 without an oxygen supply is lower than 60 mmHg in the stable state of disease.
Pulmonary Disability Class 3 - Those who feel dyspnea, even while walking on flat ground, due to chronic respiratory insufficiency, and whose FEV1 is lower than 40% of the predicted value in the resting state or the PaO2 without an oxygen supply is lower than 65 mmHg in the stable state of disease.
The clinical features of the patients were checked, as well as the respiratory diseases and standards of the disability diagnosis at the time of the disability diagnosis. Through the follow-up investigation, the date of diagnosing the disability was examined along with the patients' hospitalization and death records according to the disability class. The underlying disease of the pulmonary disability was based on the diagnosis by the pulmonary subspecialists who had made the decision. The data is presented as means standard deviations. Chi-squared tests were performed to compare the categorical variables and the orderly data was evaluated by the Mann-Whitney U test. A p value below 0.05 was considered statistically significant. Statistical analyses were performed using SPSS version 10.0 (SPSS Inc., Chicago, Illinois, USA).
RESULTS
Clinical feature of pulmonary disability
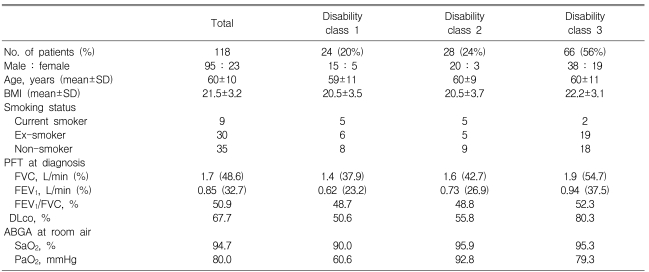
The total number of patients who had been diagnosed with pulmonary disability was 158. Among them, only 118 patients were followed up for more than 6 months. Their mean age was 60±10 years, and the number of males and females was 95 and 23, respectively. Of the 74 patients who answered the question if they had smoked, 88% had a smoking history that averaged 39±21 pack-years. For the pulmonary disability grade class, the class 1 patients were 20%, the class 2 patients were 24% and the class 3 patients were 56%. There was no significant difference for gender, age and the smoking history among the class groups (Table 1).
Of the diagnosed diseases for the pulmonary disability patients, the most frequent one was chronic obstructive pulmonary disease (COPD)(n=45, 38%), and the next ones were tuberculous destroyed lung (TDL)(n=29, 25%) and bronchial asthma (BA)(n=27, 23%). In addition, there was bronchiectasis (BE)(n=8, 6.7%), interstitial lung disease (n=5, 4%), pneumonectomy (n=3, 2.5%), and lung cancer (n=1, 0.8%) (Figure 1).

Underlying pulmonary diseases of the patients with legal pulmonary disability. The most common cause of the pulmonary disability is COPD (38%). Chronic obstructive airway diseases such as COPD, TDL (25%), and BA (23%) are the main causes of pulmonary disability.
CEP, chronic eosinophilic pneumonia; Lung Ca, lung cancer; DILD, diffuse interstitial lung disease; BE, bronchiectasis; TDL, tuberculous destroyed lung; BA, bronchial asthma; COPD, chronic obstructive pulmonary disease
As accompanying diseases, hypertension (n=15, 12.7%) was most frequent, and the next ones were diabetes mellitus (n=12, 10.1%), osteoporosis (n=8, 6.7%), and ischemic heart disease (n=6, 5.1%).
Diagnostic tests for the decision of pulmonary disability
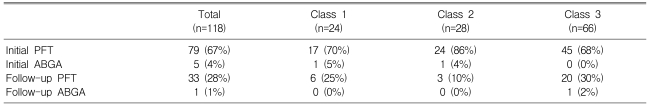
All the patients who were diagnosed with pulmonary disability had the 1st PFT performed, and 26% of them had the ABGA performed. After 2 months, only 28% of the patients had the follow-up PFT performed to check the fixation of the disease, and 13% had the follow-up ABGA performed. The rest of the patients (72%) took no follow-up tests.
For 67% of the patients, the disability decision was made on the basis of 1st PFT, and 4% of the decisions were decided by the 1st ABGA. The cases for which the decisions were not made right after the 1st PFT, but rather, they were made according to the follow-up test after 2 months and according to the disability diagnosis standards were just 29% (PFT 28%, ABGA 1%)(Table 2).
Follow-up of PFT after the diagnosis of pulmonary disability
After the decision of pulmonary disability, 42 patients were followed up with PFT. The average period for the follow-up PFT was 11.9 months and the median period was 12 months. Of them, 22 patients (52%) showed the increase of the FEV1 on the PFT; there were 10 patients with COPD, 7 with BA, 3 with TDL, 1 with BE and 1 with idiopathic pulmonary fibrosis. Especially, 8 of 22 patients (4 with BA, 2 with COPD, 1 with TDL and 1 with BE) showed a 10% or more increase in the FEV1. For 11 of the 22 patients with an increased FEV1, their FEV1 was more than 40% of the predicted value. The distribution of these patients was 5 BE patients, 4 COPD patients, 1 TDL patient and 1 idiopathic pulmonary fibrosis patient. The number of patients for whom their FEV1 was decreased was 13 (31%); there were 7 COPD patients, 3 BA patients and 3 TDL patients (Table 3).
Clinical progress of the pulmonary disability
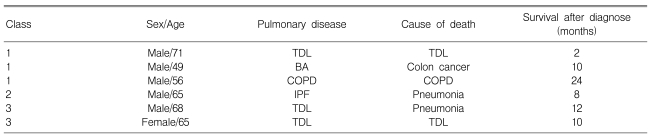
During the follow-up observation period (a median period of 16 months) after the pulmonary disability diagnosis, 6 patients died; these were 3 class 1 patients, 1 class 2 patients and 2 class 3 patients. The cause of death for 3 patients was the worsened underlying pulmonary disease, for 2 the cause of death was combined pneumonia and for 1 it was colon cancer (Table 4).
DISCUSSION
In this study, the clinical characteristics and the progress of the patients who had been decided to have pulmonary disability were observed along with their causal underlying diseases. The most important diseases that caused the decreased pulmonary function were chronic airway diseases such as COPD and BA. The airway obstruction causes a decreased FEV1 and inevitably, a respiratory locomotive disability, and it can cause pulmonary disability. For the cases that some legal claims were raised because of the pulmonary disability, the most frequent causal disease was COPD7). The next important causal diseases were TDL and BE. It seems that this is because of the high prevalence rate of tuberculosis among Koreans. TDL is a disease that causes severe destruction of the lung parenchyma due to far advanced tuberculosis, and it usually results in the chronic airflow obstruction8). It is known that the patients with chronic airflow obstruction due to a TDL have a lower FVC and FEV1 and higher airway resistance8). So, it can easily cause a disabling respiratory condition. In addition, some restrictive pattern pulmonary disorders such as interstitial lung disease or the post-pneumonectomy state could decrease the FVC and FEV1 and so they might cause pulmonary disability.
Pulmonary disability is decided when the pulmonary function decline due to chronic pulmonary disease is severe enough to interfere with the walking ability of the patient. Therefore, an index to objectively determine the locomotive disability of the patient is necessary. In Korea, the FEV1 of the PFT is the only index. It is based on that for the patients with the chronic airflow obstruction, the FEV1 testing is non-invasive and simple, and it can objectively reflect the locomotive disability of a patient6,9-12). But in other countries, especially according to the standards of pulmonary disability presented by the ATS in 1982 and 1986, 'severe pulmonary disability' is defined when the FVC on the PFT is less than 50% of the predicted value, or the FEV1 is less than 40% of the predicted value, or the ratio of the FEV1/FVC is less than 40%, or the DLco is less than 40% of the predicted value3, 4). In addition to these, if more discrimination is necessary, a pulmonary exercise test or the ABGA should be done to objectify the decision of pulmonary disability. For the case of the reversible airway obstruction such as BA or a restrictive pattern pulmonary disorder such as interstitial lung disease, another standard would be applied to decide the pulmonary disability5, 13). In case of the BA, the ATS recommends deciding on the pulmonary disability through comprehensive tests on the peak expiratory flow rate (PEFR), the PC20 of the methacholine bronchoprovocation test or the required medicines to control the symptoms of BA, as well as the FEV1 5). For the case of the interstitial lung disease, an FVC that's less than 50% of the predicted value and a DLco less than 40% of the predicted value is considered as severe disability13). In Korea, even though they are not as frequent as airway obstructive diseases, other diseases that cause a restrictive pattern pulmonary disorder like interstitial lung diseases or lobectomy or pneumonectomy seem to need another pulmonary disability standard than just the FEV1.
The most frequently used test to diagnose pulmonary disability has been the PFT. This is because determining the FEV1 via PFT is very simple and noninvasive compared with the ABGA. Before the implementing regulation of the Handicapped-person Welfare Law, the patients who had been treated for a long time were considered to be fixed in their diseases in spite of their medical treatments, and their pulmonary disability used to be decided only with the PFT and without any follow-up test. Yet when the class of the pulmonary disability was decided only through the FEV1, there were many cases that the PaO2 on the ABGA of the patient was greater than the PaO2 of the corresponding class. Therefore, when the data of the patients who were decided to have pulmonary disability is better accumulated in the future, it seems necessary to adjust the standard in order to match the PaO2 of the ABGA with the FEV1 of the PFT.
In this study, 42 patients were followed up with PFT after the diagnosis of the pulmonary disability. Of them, 22 patients showed an increased FEV1 on PFT. When deciding on the pulmonary disability, the pulmonary subspecilists confirmed that the PFT was similar to or decreased compared to the previous PFTs of the last 2 years or more. Because of the clause, "Of the repetitive test results for more than 2 months, the lowest level is used", it seems that there would be some variation of the FEV1 within a class. However, there were 8 patients whose FEV1 increased by 10% or more. Thus, if there is a FEV1 change over two classes, then the decision on the class of the pulmonary disability may have been erroneous. Such patients should be decided again, and a physician should make doubly sure not to make any errors. Moreover, for the 11 of 22 patients whose FEV1 was increased, their FEV1 increased up to more than 40% of the predicted value, which hardly allows them to be classified as having pulmonary disability. Of these 11 patients, for the 2 patients who had belonged to class 3 according to the regulation, "Of the repetitive test results for more than 2 months, the lowest level is used", their FEV1 increased a little bit later on. And, for 9 patients, their FEV1 increased by 10% or more to reach 40% of the predicted value. The disability class for these patients should also be decided again. Thus, it is necessary to carefully diagnosis the patients' disability and to follow up their conditions.
Six patients died during the clinical progress. Three of them had belonged to the class 1 of pulmonary disability, and 5 of them died of the worsened underlying pulmonary diseases or the combined pneumonia. Thus, it is highly probable that patients with the pulmonary disability will die of pulmonary diseases. Except their mortality, the other aspects of the patients such as their quality of life or the clinical features have not been analyzed for each class of pulmonary disability. In the future, it seems necessary to check the relationship of the quality of life with the disability class through a questionnaire on the quality of life or by comparison of the clinical features.
In conclusion, when deciding the pulmonary disability, it is necessary to decide it after sufficient treatment has been done and to perform periodic follow-up testing even after the disability decision for confirming that the disability is stable and also to adjust the disability class. Moreover, additional diagnostic criteria are needed in the case of BA or interstitial lung diseases. It is necessary to gather all the data when making the decision on disability by performing other additional tests