Generalized edema with acute renal failure in a patient with diabetes
Article information
A 68-year-old male patient visited the hospital for the management of bilateral lower extremities edema. He had a 20-year history of diabetes mellitus, complicated by diabetic retinopathy. Laboratory investigations revealed a serum creatinine level of 0.98 mg/dL, hemoglobin 6.6 g/dL, total protein 6.4 g/dL, albumin 2.9 g/dL, and globulin 3.5 g/dL. Urinalysis indicated significant proteinuria with 3+ protein with hematuria and a urine protein-creatinine ratio of 2,221.59 mg/g. After admission, his renal function slowly declines to serum creatinine of 1.33 mg/dL and worsens bilateral lower extremities edema. To address other possible causes of anemia and proteinuria, we evaluated the serum and urine protein electrophoresis with immunofixation and identified a monoclonal lambda subtype of immunoglobulin M (IgM). Further evaluation included a bone marrow biopsy, establishing a hematological lymphoplasmacytic lymphoma (LPL) diagnosis (Fig. 1). The renal biopsy revealed light chain cast nephropathy alongside diabetic nephropathy. Congo red staining yielded negative results, ruling out amyloidosis (Fig. 2). Consequently, a diagnosis of cast nephropathy in the context of LPL was confirmed. We treated with six cycles of bendamustine (70 mg/m2) in combination with rituximab (375 mg/m2), and the patient is currently complete remission state.

Peripheral blood smear and bone marrow biopsy. (A) The peripheral blood smear shows scattered lymphocytes (white arrow) that are small with round nuclei, condensed chromatin, and small amounts of cytoplasm. Red blood cells show rouleaux formation (× 400). (B) Bone marrow aspiration cytology shows increased atypical lymph plasmacytes (× 400). (C, D) Immunohistochemical staining results show positively in CD138 (C) and λ light chain (D).
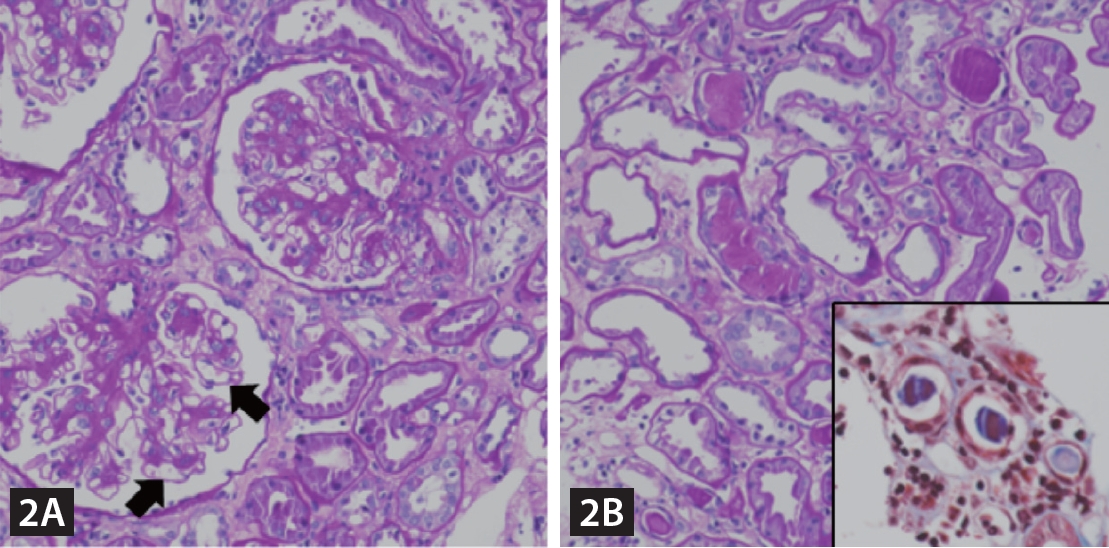
Histologic features of renal biopsy. (A) Glomeruli show diffuse mesangial matrix expansion with microaneurysm formation (arrows) (Periodic acid Schiff stain, original magnification: × 400). (B) High-power view of the tubules and interstitium showing intratubular casts with fractured appearance (Periodic acid Schiff stain, original magnification: × 400). The intratubular casts show metachromatic appearance by trichrome staining (inset, trichrome stain, original magnification: × 400).
Waldenström’s macroglobulinemia (WM), a type of LPL, is characterized by the presence of IgM monoclonal protein [1]. Light chain cast nephropathy is a form of acute or chronic kidney disease that arises from the excessive production and filtration of toxic light chains [2]. While renal biopsy-confirmed cases of cast nephropathy are commonly linked to multiple myeloma, their occurrence in WM is comparatively infrequent [3].
This case highlights the necessity of a comprehensive diagnostic approach in patients with a history of diabetes and hypothyroidism, emphasizing the need to look beyond diabetic nephropathy. Additionally, it illuminates the possibility of cast nephropathy manifesting in LPL, expanding its known association beyond multiple myeloma.
Notes
CRedit authorship contributions
Yujin Shin: data curation, investigation, formal analysis, writing- original draft; Chang-Hoon Lee: data curation, formal analysis, validation; Kyoung Min Kim: data curation, formal analysis, validation; Yong Gon Cho: data curation, formal analysis, validation; Kyung Pyo Kang: conceptualization, data curation, formal analysis, investigation funding acquisition, validation, supervision: writing- review & editing
Conflicts of interest
The authors disclose no conflicts.
Ethical statement
None
Funding
Ethical approval was obtained from the Jeonbuk National University Hospital Institutional Review Board (CUH 2024-12-023) and written informed consent was waived.
