Reduced-intensity chemotherapy with tyrosine kinase inhibitor followed by allogeneic transplantation is effective in patients with Philadelphia chromosome-positive acute lymphoblastic leukemia
Article information
Abstract
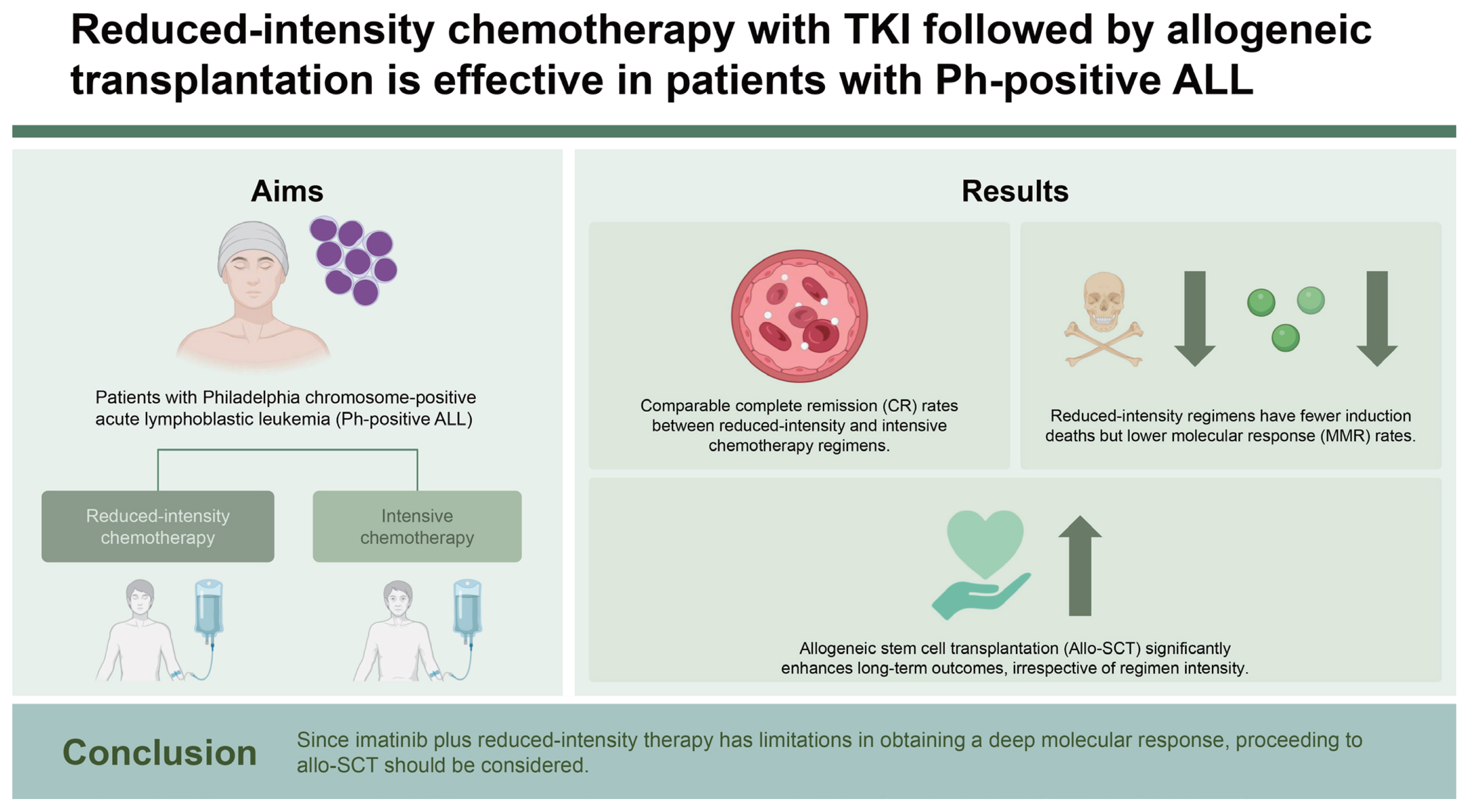
Background/Aims
To determine the effectiveness of tyrosine kinase inhibitor (TKI) plus reduced-intensity therapy in adult patients with newly diagnosed Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph-positive ALL), this retrospective study compared treatment outcomes and induction mortality according to backbone regimen intensity.
Methods
The data of 132 patients diagnosed with Ph-positive ALL were retrospectively collected from five centers. Patients received imatinib plus intensive chemotherapy (modified VPD, KALLA1407, or hyper-CVAD) or reduced-intensity chemotherapy (EWALL) for curative purposes. This study analyzed 117 patients, of which 35,22,46, and 14 received modified VPD, KALLA1407, hyper-CVAD, and EWALL, respectively. All patients used imatinib as a TKI.
Results
The median age of the patients who received reduced-intensity chemotherapy was 64.4 years, while that of the patients with intensive regimens was 47.5 years. There was no induction death in the reduced-intensity group, while nine patients died in the intensive therapy group. Major molecular response achievement tended to be higher in the intensive chemotherapy group than in the reduced-intensity group. More patients in the intensive chemotherapy group received allogeneic stem cell transplantation (allo-SCT). There was no statistically significant difference in long-term survival between the two groups in terms of relapse-free survival and overall survival rates.
Conclusions
When imatinib plus reduced-intensity therapy was used as a frontline treatment, there was no inferiority in obtaining complete remission compared to imatinib plus intensive chemotherapy or significant difference in long-term survival. Since imatinib plus reduced-intensity therapy has limitations in obtaining a deep molecular response, proceeding to allo-SCT should be considered.
INTRODUCTION
The Philadelphia chromosome is one of the most common cytogenetic abnormalities in patients with B-cell precursor acute lymphoblastic leukemia (ALL) [1,2]. Approximately 30–40% of newly diagnosed adults ALL patients present the Philadelphia chromosome, which has been indicated as an unfavorable factor for chemotherapy and prognosis [1]. Prior to the use of a tyrosine kinase inhibitor (TKI) to treat Philadelphia chromosome-positive (Ph-positive) ALL, long-term survival was very poor [3]. Previous trials reported that 70–90% of patients who received intensive chemotherapy achieved complete remission (CR). However, most patients relapsed and died within 6–11 months of treatment [3–5]. Kantarjian et al. showed that the 5-year survival rate for patients who received the hyper-CVAD regimen for Ph-positive ALL was only 7%, although the CR rate was 91% [4]. In the study of the Cancer and Leukemia Group B (CALGB), the 3-year overall survival (OS) rate was 19% [5]. Since the introduction of TKIs in the treatment of Ph-positive ALL, significant improvements in treatment outcomes have been confirmed [3,6,7]. For example, patients who received intensive chemotherapy plus imatinib showed a 5-year OS rate of over 40% [8]. In patients with nilotinib plus multiagent chemotherapy, 2-year relapse-free survival (RFS) and OS rates of over 70% were also reported [9]. However, with the introduction of TKIs as the first-line treatment for newly diagnosed Ph-positive ALL patients, controversy has arisen about the effectiveness of the intensive chemotherapy used as the basis. Intensive regimens reported induction mortality rates of 5–10% [10,11]. Moreover, some patients, even those who achieved remission, discontinued the treatment or died due to the toxicities of chemotherapy [10,11]. Although it is difficult to achieve a deep molecular response, reduced-intensity chemotherapy was not inferior to intensive chemotherapy in achieving hematologic CR [12–14]. In the Gruppo Italiano Malattie Ematologiche dell’Adulto (GIMEMA) trial, elderly patients who received imatinib plus dexamethasone achieved a CR rate of 100% [12]. In addition, dasatinib combined with reduced-intensity chemotherapy showed a 96% CR rate, and 65% of patients achieved a 3-log reduction in BCR-ABL1 levels in the European Working Group on Adult ALL (EWALL) study [13]. Reduced-intensity chemotherapy has the advantage of not only achieving CR but also allowing allogeneic stem cell transplantation (allo-SCT) under favorable conditions with a low risk of toxicity [15]. A low- or reduced-intensity regimen with TKIs followed by allo-SCT in patients with CR is a viable option for adult Ph-positive ALL patients [16].
The Adult Acute Lymphoblastic Leukemia Working Party of the Korean Society of Hematology (KAALLWP) has suggested the benefits of imatinib plus modified VPD or imatinib plus KALLA 1407. In addition, imatinib plus hyper-CVAD was also used as a frontline therapy for newly diagnosed adult Ph-positive ALL patients. However, there are still a few studies evaluating the effectiveness of imatinib plus reduced-intensity chemotherapy compared to imatinib plus intensive chemotherapy for transplant-eligible patients in Korea. Thus, the current retrospective study compared treatment outcomes and induction mortality according to regimen intensity. It also compared the outcomes of combination chemotherapy regimens used over the past 10 years and analyzed the role of allo-SCT in the TKI era.
METHODS
Patients
Five centers retrospectively collected the data of 132 patients diagnosed with Ph-positive ALL from January 2011 to December 2022. Patients who were diagnosed with Ph-positive ALL according to the World Health Organization’s classification via bone marrow (BM) examination and cytogenetic studies and received TKI plus intensive chemotherapy or TKI plus a reduced-intensity regimen for curative purposes were enrolled [17]. Patients who did not have adequate organ function (cardiac function [ejection fraction > 45%] assessed by echocardiogram, kidney function [creatinine < 1.5 mg/dL], and liver function [bilirubin < 1.5 mg/dL; transaminase levels < three times the upper normal limit]) before starting the chemotherapy were excluded. Patients who had uncontrolled infections or illnesses treated with other investigational agents were also excluded. All procedures in this study that involved human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. This study was approved by the Institutional Review Board of Kyungpook National University Hospital (2024-06-016) and each other participating center.
Treatments
Patients received imatinib plus intensive chemotherapy or reduced-intensity chemotherapy for curative purposes. Intensive chemotherapy included modified VPD, KALLA1407, and hyper-CVAD regimens [4,9–11]. The EWALL regimen was used as the reduced-intensity chemotherapy [13]. Each chemotherapy schedule was implemented according to previous studies [4,9–11,13]. Central nervous system (CNS) prophylaxis was performed using 15 mg of intrathecal methotrexate with 50 mg of hydrocortisone during each chemotherapy course, considering the patients’ conditions. After achieving CR, patients with a human leukocyte antigen (HLA)-matched sibling or unrelated donor proceeded to allo-SCT according to the clinician’s discretion.
Response definitions
The BM study was performed on the 28th day after the initiation of chemotherapy to determine the response to induction. CR was achieved when the following criteria were met: < 5% blasts in the BM, ≥ 20% cellularity in the BM biopsy with normal trilineage hematopoiesis, the disappearance of BM chromosomal abnormality, the absence of leukemia blasts in the peripheral blood (PB), an absolute neutrophil count (ANC) ≥ 1,000/μL, platelets ≥ 100,000/μL, and no evidence of extramedullary involvement of the CNS or soft tissue. CR with incomplete hematologic recovery (CRi) was achieved when the patient achieved all the criteria for CR except recovery of ANC (< 1,000/μL) or recovery of platelet count (< 100,000/μL) [18–20]. Major molecular response (MMR) was defined as a BCR-ABL1:ABL1 ratio ≤ 0.1% on the International Scale for p210 BCR-ABL1 or a 3-log reduction in transcripts for p190 BCR-ABL1 but not meeting the criteria for complete molecular response (CMR, BCR-ABL1 ≤ 0.01%) [21]. Relapse was defined as disease recurrence after achieving CR or CRi with ≥ 5% blasts in the BM, blasts in the PB, or evidence of new extramedullary involvement.
Statistical analyses
Continuous variables were reported as medians with ranges, and categorical variables were summarized by counts with proportions. Fisher’s exact test was employed for categorical variables, while the Wilcoxon rank-sum test was utilized for continuous variables in between-group comparisons. RFS was calculated from the date of diagnosis to either the date of relapse, disease progression, death from any cause, or last follow-up. OS was measured from the date of diagnosis to the date of death from any cause or last follow-up. The probabilities of RFS and OS rates were calculated using the Kaplan–Meier method and compared using the log-rank test. The Cox regression model was used for identifying the factors for long-term survival. Factors with a p value of ≤ 0.1 in the univariate analysis were included in the multivariate analysis. The hazard ratio (HR) and 95% confidence interval (CI) were estimated for each factor. A p value of < 0.05 was considered to be statistically significant. The study used R statistical software program version 4.4.0 (R Foundation for Statistical Computing, Vienna, Austria: available at https://www.r-project.org/).
RESULTS
Patient characteristics
This retrospective study analyzed 117 patients from five centers in total. As a backbone chemotherapy, 35, 22, 46, and 14 patients received modified VPD, KALLA1407, hyper-CVAD, and EWALL, respectively. All patients included in the analysis used imatinib as a TKI. The median age of patients who received EWALL therapy was significantly higher than that of patients who received intensive chemotherapy (p = 0.001). The EWALL group had a higher proportion of patients over 50 years of age (85.7%) than the intensive chemotherapy groups. Patients with CNS involvement were not included in this study. More than half of the patients who received intensive chemotherapy could proceed to allo-SCT, while only 21.4% of patients who received reduced-intensity chemotherapy were eligible for transplantation. The baseline patient characteristics are summarized in Table 1.
Response to induction therapy and long-term outcomes according to each regimen
Table 2 shows the response to induction chemotherapy according to each regimen. The CR rate of the patients administered the EWALL regimen plus imatinib was 85.7%, while that of those administered intensive regimens plus imatinib was 85–91%. The MMR rates of the modified VPD, KALLA1407, and hyper-CVAD regimens were 68.6%, 72.7%, and 80.4%, respectively. The MMR rate of the patients who received the EWALL regimen plus imatinib was lower than that of the patients who received intensive therapy at 57.1%. However, there was no death during induction therapy in the EWALL plus imatinib group.
The 3-year RFS and OS rates of all enrolled patients were 33.0% and 38.7%, respectively (Supplementary Fig. 1). Supplementary Table 1 summarizes the long-term survival outcomes according to chemotherapy type. The 3-year RFS and OS rates of the KALLA1407 regimen were 54.2% and 54.5%, respectively, showing that it was superior to other regimens. In the Kaplan–Meier curve, the KALLA1407 regimen tended to be superior to other regimens in RFS rate, but there was no statistical difference in terms of OS rate (Supplementary Fig. 2).
Comparison of intensive vs. reduced-intensity chemotherapy
Table 3 summarizes the characteristics and treatment outcomes of patients who used the reduced-intensity regimen and intensive regimens as their frontline therapy. The median age of the patients who received reduced-intensity chemotherapy was 64.4 years, compared to 47.5 years for those who received intensive regimens. The proportion of patients over 50 years of age was also higher in the reduced-intensity group (85.7% vs. 45.6%, p = 0.011). During induction chemotherapy, no patient died in the reduced-intensity group, but nine patients (8.7%) died in the intensive therapy group. MMR achievement tended to be higher in the intensive chemotherapy group than the reduced-intensity group (74.8% vs. 57.1%, p = 0.072). More patients in the intensive chemotherapy group received allo-SCT. The 3-year RFS rates of the intensive chemotherapy group and reduced-intensity regimen group were 34.3%, and 23.8%, respectively. The 3-year OS rate was 38.7% in both groups. There was no statistically significant difference in long-term survival in terms of RFS or OS rates between the two groups (Fig. 1).

Kaplan–Meier curves according to the intensity of regimens. There was no statistically significant difference in long-term survival in terms of relapse-free survival (RFS) (A) or overall survival (OS) (B) between the two groups.
When targeting patients over 50 years of age, 12 patients received reduced-intensity regimen while 47 patients received intensive chemotherapy. The 2- and 3-year RFS rates for patients treated with reduced-intensity regimen were 33.3% and 16.7%, while those for patients with intensive chemotherapy were 27.3% and 23.9%, respectively. The 2- and 3-year OS rates for patients treated with a reduced-intensity regimen were 41.2% and 20.6%, while those for patients with intensive chemotherapy were 29.6% and 26.6%, respectively. In Kaplan–Meier survival curves, there was no significant difference in RFS and OS between the two groups (Supplementary Fig. 3).
Factors affecting long-term outcomes
Cox regression analyses were conducted to identify factors affecting long-term survival in terms of RFS and OS rates. Table 4 shows the results of the univariate and multivariate analyses. In the multivariate analysis, proceeding to allo-SCT was a favorable factor for RFS rate (HR, 0.338; p < 0.001) and OS rate (HR, 0.477; p = 0.004), whereas older age (≥ 50 yr) at the time of diagnosis was an unfavorable predictor for OS rate (HR, 1.732; p = 0.037) (Table 4). The intensity of the regimen was not an independent factor that affected RFS or OS rates.
Considering all enrolled patients, patients who received allo-SCT showed significantly better RFS and OS rates than those who did not receive allo-SCT (Fig. 2A, B). Furthermore, even when targeting only patients who achieved CR/CRi after induction therapy, patients who received transplantation showed superior outcomes in RFS and OS rates compared to patients who did not receive transplantation (Fig. 2C, D).

Comparison of survival outcomes between patients who received allogeneic stem cell transplantation (allo-SCT) and those who did not. For all patients, the group of patients who received allo-SCT showed significantly better relapse-free survival (RFS) (A) and overall survival (OS) (B) than those who did not receive allo-SCT. When targeting only patients who achieved complete remission after induction therapy, those who received transplantation showed superior outcomes in RFS (C) and OS (D) compared to patients who did not receive transplantation.
DISCUSSION
The current study used modified VPD, KALLA1407, hyper-CVAD, and EWALL as the backbone regimens and added a first-generation TKI, imatinib. There was no significant difference in long-term survival between the patients with intensive chemotherapy and the patients with the reduced-intensity regimen. Notably, there were no deaths during induction in patients treated with reduced-intensity therapy. Although there may be a selection bias that patients who received transplantation may have better performance, our data suggests that allo-SCT still has the potential role to improve survivals even after the introduction of TKIs in patients with Ph-positive ALL.
Previous studies on the reduced-intensity therapy using imatinib plus vincristine and dexamethasone-based regimens showed a CR rate of over 90%, but the CMR was found to be 25–40%. The 3-year OS rate in one study was 74%, and the 5-year OS rate in another study was 43% [16,22]. In the current study, the CR/CRi rate of the patients with EWALL plus imatinib was 85.7%, and the MMR rate was 57.1%. The 3-year OS rate was 38.7%. Compared to previous studies, the long-term survival of our study was relatively low because most of the patients who received reduced-intensity therapy in this study were elderly (median age of 64.4 years) and could not receive transplantation or intensive chemotherapy.
Although previous studies have shown the benefits of reduced-intensity therapy for newly diagnosed Ph-positive ALL, limitations must be considered when using first- or second-generation TKIs. Relapses were the main cause of treatment failure due to the emergence of the T315I mutation, reflecting insufficient disease control. In a study on Ph-positive ALL, BCR-ABL kinase domain mutations, mainly the T315I mutation, were detected in 70% of imatinib-resistant patients, and among the patients with imatinib failure, 78% of patients reported to be resistant to second-generation TKIs [23]. To overcome genetic mutations that indicate adverse prognosis, such as the T315I mutation, there was no alterative but to attempt an allo-SCT. Patients who are ineligible for transplantation or do not have an HLA-matched donor are bound to experience poor treatment outcomes. However, ponatinib was found to be the most potent BCR-ABL1 inhibitor in leukemias with both wild-type and mutated BCR-ABL1, including the T315I mutation [24,25]. Research on the necessity of intensive chemotherapy and allogeneic transplantation in the treatment of adult Ph-positive ALL patients has intensified since the introduction of ponatinib. Administering ponatinib and intensive chemotherapy as frontline therapy may not further improve treatment outcomes with allo-SCT. In a clinical trial with ponatinib plus the hyper-CVAD regimen in newly diagnosed Ph-positive ALL, the 3-year OS rate of patients who did not receive a transplantation was 87%, while that of patients who proceeded to allo-SCT was 70% [26,27]. In this ponatinib plus intensive chemotherapy study, nine patients died in CR. Among them, three died from severe infections. Studies are also being attempted to treat newly diagnosed patients with ponatinib and reduced-intensity therapy or a chemo-free regimen instead of intensive chemotherapy. The PhALLCON study (NCT 03589326) showed that ponatinib was superior to imatinib in combination with reduced-intensity therapy with a significantly higher minimal residual disease-negative CR rate [28]. In particular, benefits of the ponatinib group were observed in patients ≥ 60 years and in patients with the BCR/ABL1 p190 variant [29]. Recently, the use of ponatinib and blinatumomab as first-line treatments yielded the most encouraging results. Ponatinib in combination with blinatumomab may overcome the negative prognostic effect of genomic changes such as Ikaros (IKZF1) or IKZF1plus [29–31] deletion.
In this study, patients receiving KALLA1407 regimen showed better 3-year RFS and OS rates than others. According to the previous study related to the KALLA regimen, Ph-positive ALL patients under 40 years of age showed significantly superior long-term survivals compared to patients over 40 years of age when they received KALLA1407 regimen [10]. Our data showed that the proportion of younger patients in the KALLA1407 group was relatively higher than that of other chemotherapy groups, which might affect the RFS and OS rates. Although our retrospective analysis did not show inferiority in long-term survival in patients with reduced-intensity therapy compared to patients with intensive chemotherapy, the results in this study should be cautiously interpreted due to certain limitations. First, the current study is retrospective. Second, the number of patients who received the reduced-intensity regimen was relatively small, and few young patients eligible for transplantation have received reduced-intensity therapy as a frontline treatment. Furthermore, among the patients administered the EWALL regimen, the number of patients who received transplantations was too small, making it difficult to analyze the transplant effect in reduced-intensity therapy. Finally, this study failed to address the impact of genetic abnormalities other than the Philadelphia chromosome.
In conclusion, when imatinib plus reduced-intensity therapy was used for newly diagnosed Ph-positive ALL patients as a frontline treatment, there was no inferiority in obtaining CR compared to imatinib plus intensive chemotherapy, and there was no significant difference in long-term survival. Since imatinib plus reduced-intensity therapy has limitations in obtaining a deep molecular response, proceeding to allo-SCT should be considered.
KEY MESSAGE
1. When used as a frontline treatment for newly diagnosed Ph-positive ALL patients, imatinib plus reduced-intensity therapy showed no inferiority in achieving CR compared to imatinib plus intensive chemotherapy, and there were no deaths during induction in patients treated with reduced-intensity therapy.
2. There was no significant difference in long-term survival between the patients with intensive chemotherapy and the patients with the reduced-intensity regimen.
3. Since imatinib plus reduced-intensity therapy has limitations in obtaining a deep molecular response, proceeding to allo-SCT should be considered.
Notes
CRedit authorship contributions
Jung Min Lee: resources, data curation, writing - original draft, writing - review & editing; Do Young Kim: resources, data curation, writing - original draft, writing - review & editing; Hee Jeong Cho: resources, data curation, writing - review & editing; Joon Ho Moon: data curation, writing - original draft, writing - review & editing; Sang Kyun Sohn: resources, data curation, writing - original draft, writing - review & editing; Ho Jin Shin: resources, data curation, writing - original draft, writing - review & editing; Young Rok Do: resources, data curation, writing - original draft, writing - review & editing; Mi Hwa Heo: resources, data curation, writing - original draft, writing - review & editing; Min Kyoung Kim: resources, data curation, writing - original draft, writing - review & editing; Young Seob Park: resources, data curation, writing - original draft, writing - review & editing; Dong Won Baek: conceptualization, resources, data curation, writing - original draft, writing - review & editing
Conflicts of interest
The authors disclose no conflicts.
Funding
None