Predictive value and optimal cut-off level of high-sensitivity troponin T in patients with acute pulmonary embolism
Article information
Abstract
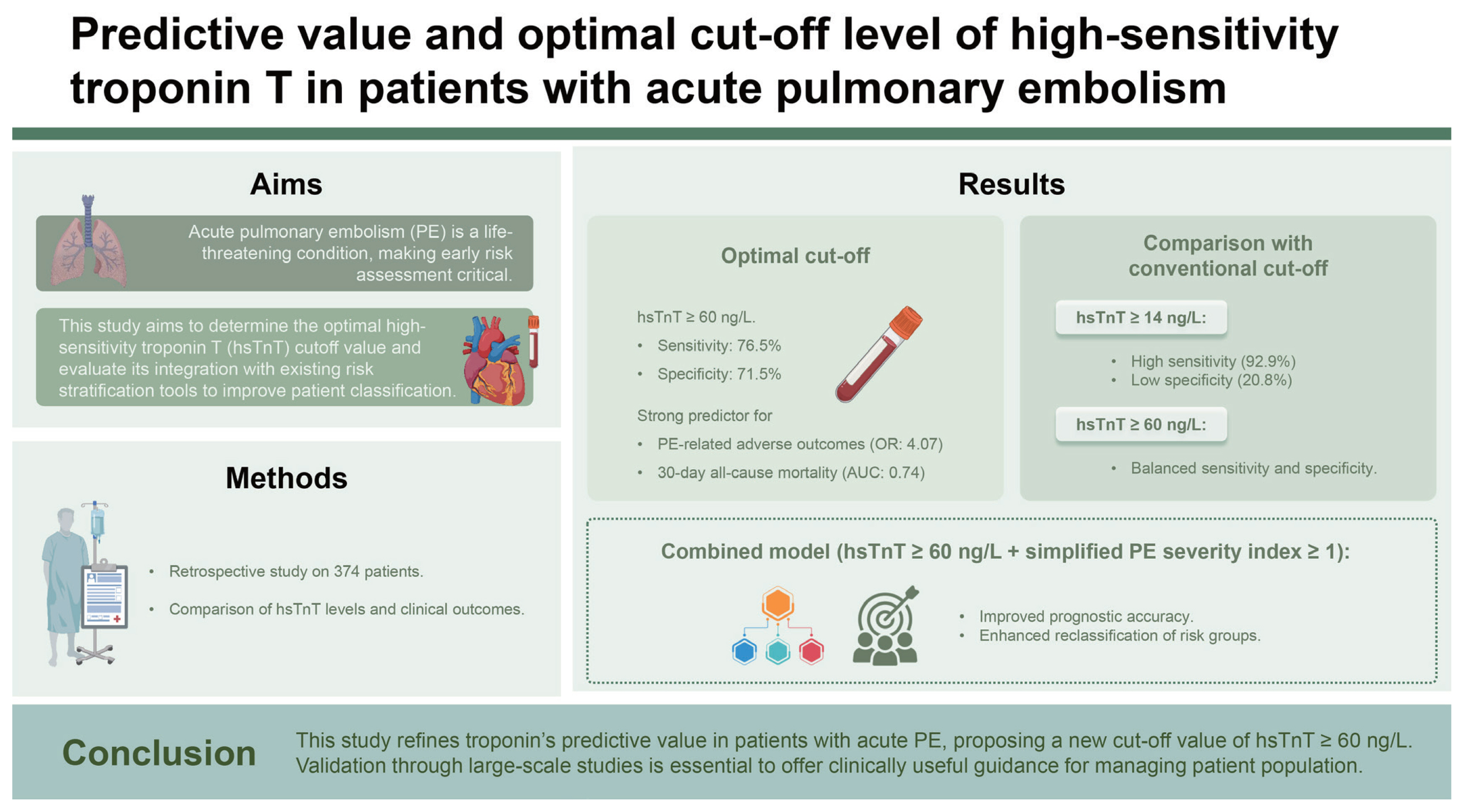
Background/Aims
Elevated troponin levels predict in-hospital mortality and influence decisions regarding thrombolytic therapy in patients with acute pulmonary embolism (PE). However, the usefulness of high-sensitivity troponin T (hsTnT) regarding PE remains uncertain. We aimed to establish the optimal cut-off level and compare its performance for precise risk stratification.
Methods
374 patients diagnosed with acute PE were reviewed. PE-related adverse outcomes, a composite of PE-related deaths, cardiopulmonary resuscitation incidents, systolic blood pressure < 90 mmHg, and all-cause mortality within 30 days were evaluated. The optimal hsTnT cut-off for all-cause mortality, and the net reclassification index (NRI) was used to assess the incremental value in risk stratification.
Results
Among 343 normotensive patients, 17 (5.0%) experienced all-cause mortality, while 40 (10.7%) had PE-related adverse outcomes. An optimal hsTnT cut-off value of 60 ng/L for all-cause mortality (AUC 0.74, 95% CI 0.61–0.85, p < 0.001) was identified, which was significantly associated with PE-related adverse outcomes (OR 4.07, 95% CI 2.06–8.06, p < 0.001). Patients with hsTnT ≥ 60 ng/L were older, hypotensive, had higher creatinine levels, and right ventricular dysfunction signs. Combining hsTnT ≥ 60 ng/L with simplified pulmonary embolism severity index ≥1 provided additional prognostic information. Reclassification analysis showed a significant shift in risk categories, with an NRI of 1.016 ± 0.201 (p < 0.001).
Conclusions
We refined troponin’s predictive value in patients with acute PE, proposing a new cut-off value of hsTnT ≥ 60 ng/L. Validation through large-scale studies is essential to offer clinically useful guidance for managing patient population.
INTRODUCTION
Early prognostic stratification is crucial for patients with symptomatic acute pulmonary embolism (PE) to determine appropriate therapeutic interventions and optimize clinical outcomes [1]. According to the 2019 European Society of Cardiology (ESC) guidelines for acute PE, patients presenting with clinical symptoms and signs indicative of hemodynamic instability are classified as having a high risk of early (in-hospital or 30-day) death. Subsequently, the remaining patients are further stratified into intermediate-high, intermediate-low, and low-risk groups. Risk indicators include the pulmonary embolism severity index (PESI) or simplified PESI (sPESI) score, right ventricular (RV) dysfunction through echocardiography or computed tomography pulmonary angiography (CTPA), and elevated biomarker levels [1]. While several biomarkers, such as cardiac troponin, B-type natriuretic peptide (BNP), and creatinine, have demonstrated individual or additive predictive values, only cardiac troponin has been incorporated into management guidelines based on extensive research.
Troponin elevation is thought to result from a sudden increase in pulmonary vasculature resistance, leading to RV dilatation and subsequent alteration of the contractile properties of the myocardium. The extent of troponin release appears to be dependent on the severity of PE [1–3]. However, previous validation studies did not provide separate cut-off values for troponin I or troponin T and were all conducted using their normal upper limits. In particular, the advent of the high-sensitivity troponin T (hsTnT) assay in 2009 significantly enhanced the detection of troponin levels that fell below the detection limits of conventional assays [4]. Therefore, debates surrounding whether elevated hsTnT levels, defined by the 99th percentile upper reference limit (URL) of 14 ng/L, can effectively identify patients at a heightened risk of short-term adverse outcomes and guide the administration of thrombolytic therapy.
In this study, we aimed to investigate the prognostic relevance of hsTnT, establish the optimal hsTnT cut-off level, and compare its performance in the risk stratification of patients with acute PE.
METHODS
Study participants and designs
This study retrospectively examined 394 consecutive patients diagnosed with acute PE between July 1, 2020, and September 30, 2023, at Gyeongsang National University Hospital in Jinju, Republic of Korea. Exclusions were made of patients with end-stage renal disease requiring hemodialysis (n = 2) and those with missing hsTnT levels on admission (n = 18). Consequently, 374 patients were included in the analysis. The diagnoses of all the patients were confirmed using CTPA. This study was approved by the Institutional Review Board of Gyeongsang National University Hospital (IRB No. GNUH-2023-08-015) and the requirement for informed consent was waived.
Clinical characteristics
Baseline demographic and clinical data were obtained through individual chart reviews in the institution’s electronic medical record system. The following clinically relevant comorbidities were analyzed: diabetes mellitus, hypertension, dyslipidemia, chronic kidney disease, history of cancer, and history of chronic pulmonary disease. Additionally, recent immobilization and surgery within the last 4 weeks were considered. A history of cancer was defined as a known malignant disease or treatment received within the past five years. Chronic pulmonary disease encompasses various conditions, including heart failure, asthma, chronic obstructive pulmonary disease, emphysema, chronic bronchitis, and interstitial lung disease.
Laboratory parameters
Among the 374 eligible patients, 341 underwent transthoracic echocardiography (TTE) during hospitalization, and all measurements adhered to the recommendations of the American Society of Echocardiography [5]. Because of various specificity and sensitivity of the individual TTE parameter, RV dysfunction was defined as the presence of one or more of the following echocardiography findings: decreased peak systolic velocity of tricuspid annulus (< 9.5 cm/s), decreased tricuspid annular plane systolic excursion measured with M-mode (< 16 mm), and decreased fractional area contraction (< 35 %), and a right/left ventricle diameter ratio ≥ 1.0 from the apical or subcostal view.
All patients underwent an initial 12-lead electrocardiographic (ECG) assessment. RV strain was defined as the presence of one or more of the following ECG findings: incomplete or complete right bundle branch block (RBBB), T-wave inversions in leads V1–V3, and S1Q3T3 pattern. Routine laboratory parameters, including hsTnT levels, were measured directly after blood withdrawal when initial diagnostic tests for suspected PE were started, ensuring a timely and accurate assessment of the acute phase response. The concentrations of hsTnT were analyzed using the Roche Cobas® 8000 analyzer (Roche Diagnostics, Mannheim, Germany) with an analytical range of 3–10,000 ng/L. A concentration of 14 ng/L has been identified as the 99th percentile URL for a healthy reference population, with a coefficient variation of less than 10%.
Clinical outcomes
PE-related adverse outcomes and all-cause mortality within 30 days were assessed. PE-related adverse outcomes were defined as a composite of (1) PE-related death, (2) incidence of cardiopulmonary resuscitation (CPR), and (3) systolic blood pressure (SBP) < 90 mmHg. All-cause mortality encompassed deaths related to acute PE or other causes, including malignancy or septic shock, within 30 days of PE diagnosis. Specifically, PE-related death was determined in the absence of an alternative diagnosis, and all clinical outcomes were assessed within 30 days of hospitalization. For the risk assessment, the sPESI score was calculated for each patient. This index assigned one point for the presence of each of the following variables: (1) age > 80 years; (2) history of cancer; (3) history of chronic cardiopulmonary disease; (4) heart rate ≥ 110 beats per minute; (5) SBP < 100 mmHg; and (6) oxygen saturation < 90% at the time of diagnosis [6].
Statistical analysis
Categorical variables are expressed as absolute numbers with percentages and compared using the chi-squared test or Fisher’s exact test, as appropriate. Continuous variables not adhering to a normal distribution are presented as medians with interquartile ranges (IQRs). The non-parametric Mann–Whitney U test was used to compare continuous variables. The Kruskal–Wallis test, a non-parametric alternative to analysis of variance (ANOVA), was used to compare normotensive subgroups and high-risk patients with PE, followed by pairwise Wilcoxon post-hoc tests for detailed group comparisons. Youden’s index was used to identify and select the optimal hsTnT cut-off level for predicting all-cause mortality. Receiver operating characteristic (ROC) curve analyses were performed to determine the area under the curve (AUC) with corresponding 95% confidence intervals (CIs). The efficacy of the newly defined levels was assessed by calculating the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), accuracy, and positive likelihood ratio. The prognostic relevance of dichotomous/dichotomized variables regarding study outcomes was assessed using univariate logistic regression analysis. After adjusting for confounders such as age, sex, history of cancer, and history of chronic pulmonary disease, a multivariable logistic regression analysis was performed. Notably, the variables used to calculate sPESI scores were not included. Harrell’s C-statistic was used to assess the accuracy of correctly classifying patients into different risk categories, as outlined in the 2019 ESC guidelines, following the application of the newly defined hsTnT cut-off level. The net reclassification index (NRI) with the corresponding standard error was assessed using the incremental value when elevated cardiac troponin levels were specifically aligned with the newly defined hsTnT cut-off level. A two-sided significance level of 5% was defined as appropriate to indicate statistical significance. All statistical analyses were performed using R software (R: A language and environment for statistical computing; R Foundation for Statistical Computing, Vienna, Austria; https://www.r-project.org/).
RESULTS
Optimal cut-off hsTnT level in normotensive patients
According to the 2019 ESC guidelines [1], patients were categorized into two groups: hemodynamically unstable patients, classified as the high-risk group, and hemodynamically stable and normotensive patients. The latter group necessitated further assessment using RV dysfunction on TTE or CTPA and cardiac troponin evaluation. Hence, only normotensive patients (n = 343) were isolated from a distinct group, and the optimal hsTnT cut-off level was determined for this study. Among normotensive patients, a total of 17 (5.0%) experienced all-cause mortality. An AUC of 0.74 (95% CI 0.61–0.85) was calculated using ROC analysis, demonstrating a sensitivity of 76.5% and specificity of 71.5%. The optimal cut-off for this prediction was an hsTnT level of 60 ng/L, which was subsequently used for all analyses (Fig. 1). An AUC for PE-related adverse outcomes was also 0.75 (95% CI 0.68–0.83).
Baseline clinical characteristics of the study population
The median age of the study participants was 76 years (IQR 66–83 yr), and 43.3% were male. The initial hsTnT levels ranged from 3 to 1,140 ng/L, with a median of 34.0 ng/L (IQR 16.0–80.0 ng/L). In the study population, 31 (8.3%) patients were hemodynamically unstable at the time of PE diagnosis. The majority, comprising 343 (91.7%) patients, were normotensive. Among the normotensive patients, 106 (30.9%) exhibited hsTnT levels exceeding the pre-defined cut-off level of 60 ng/L, accounting for 28.3% of all patients. When three groups were compared (normotensive patients with hsTnT < 60 ng/L and ≥ 60 ng/L and high-risk patients), significant differences were observed in age and recent immobilization or surgery rates. Among normotensive patients, those with hsTnT ≥ 60 ng/L had lower SBP and exhibited hypoxemia more frequently. The levels of creatinine, lactic acid, NT-proBNP, and hsTnT, indicative of tissue or myocardial ischemia, were significantly stratified among the three groups. Thrombolytic therapy was administered to 7.0% of the total patients and to 16.1% of high-risk patients (p = 0.004). Additionally, 21 normotensive patients who experienced deterioration during hospitalization received thrombolytic therapy. At discharge, most patients were prescribed oral anticoagulation. However, patients who died, those identified to be at increased risk of active bleeding, or those in whom thromboprophylaxis was contraindicated for other reasons were managed without anticoagulants (Table 1).
Comparison of prognostic factors, and clinical outcomes
Regarding prognostic factors, patients with hsTnT ≥ 60 ng/L exhibited a higher prevalence of adverse indicators, including sPESI ≥ 1 point (63.7% vs. 75.5%, p = 0.043), NT-proBNP ≥ 600 pg/mL (42.6% vs. 67.9%, p < 0.001), and RV dysfunction on TTE (23.2% vs. 51.9%, p < 0.001) (Table 2). The composite measure of RV strain on ECG, which included T-wave inversions in V1–V3, RBBB, and the S1Q3T3 pattern, demonstrated a substantial difference as well (33.3% vs. 46.2%, p = 0.031). The detailed baseline TTE and ECG findings are summarized in the Supplementary Table 1 and 2. Regarding clinical outcomes, within the group of 31 high-risk patients, 9 did not recover their blood pressure and eventually died after CPR. Among the normotensive patients, the number of all-cause mortality was 17 (5.0%), showing significant differences between hsTnT < 60 ng/L and ≥ 60 ng/L, with 4 (1.7%) and 13 (12.3%) patients, respectively. Notably, all PE-related adverse outcomes occurred exclusively in the hsTnT ≥ 60 ng/L group. Specific causes of death are shown in Supplementary Table 3.
Predictors of PE-related adverse outcomes and all-cause mortality
Univariable logistic regression analysis showed that hsTnT ≥ 60 ng/L and NT-proBNP ≥ 600 pg/mL were associated with PE-related adverse outcomes and all-cause mortality. After adjusting for age, sex, history of cancer, and history of chronic pulmonary disease, only hsTnT ≥ 60 ng/L remained as an independent predictor of PE-related adverse outcomes. Regarding all-cause mortality, hsTnT ≥ 60 ng/L and NT-proBNP ≥ 600 pg/mL retained significance (Table 3). By the ROC curve analysis of the various predictors, hsTnT ≥ 60 ng/L was identified as the most powerful predictor, with its AUC comparable with that of sPESI score ≥ 1 (0.67 vs. 0.66, p = 0.772, Fig. 2).

Receiver operating characteristic curves illustrating the binary performance of various predictors for all-cause mortality in 343 normotensive patients. hsTnT, high-sensitivity troponin T; AUC, area under the curve; sPESI, simplified pulmonary embolism severity index; RV, right ventricular; TTE, transthoracic echocardiography; NT-proBNP, N-terminal pro-B-natriuretic peptide; ECG, electrocardiogram.
sPESI score and hsTnT for prediction of all-cause mortality
The assessment of the prognostic performance for all-cause mortality is shown in Table 4, incorporating the sPESI score, hsTnT levels, and their combinations. sPESI ≥ 1 point was observed in 261 (69.8%) patients and demonstrated the highest sensitivity and NPV. A combined model of sPESI ≥ 1 point and hsTnT ≥ 60 ng/L was observed in 96 (25.7%) patients, representing the lowest prevalence among other parameters. However, this model exhibited the highest AUC and positive likelihood ratio for the clinical outcomes. When comparing the conventional hsTnT level of 14 ng/L with the proposed hsTnT level of 60 ng/L, sensitivity decreased from 92.9% to 75.0%, while specificity increased from 20.8% to 70.8%. A comparison of the prognostic values for PE-related adverse outcomes confirmed the additional utility of an hsTnT level of 60 ng/L on sPESI (Supplementary Table 4). The clinical outcomes according to sPESI and hsTnT levels are illustrated in Supplementary Table 5.
Risk reclassification by hsTnT ≥ 60 ng/L
If the elevated cardiac troponin levels, identified as a risk indicator in the 2019 ESC classification of PE severity [1], were specifically defined as hsTnT ≥ 60 ng/L instead of conventional hsTnT ≥ 14 ng/L, the Harrell’s C-index significantly improved from 0.72 to 0.80 (p = 0.008). The Hosmer-Lemeshow goodness-of-fit test remained non-significant for both hsTnT ≥ 60 ng/L and ≥ 14 ng/L models (p = 0.685 and p = 0.519, respectively). Furthermore, a Sankey diagram was used to quantitatively depict patients’ transition across different risk categories (Fig. 3). Among the 103 patients initially classified into the intermediate-high risk category, 50 (48.5%) underwent reclassification into the intermediate-low risk category. Similarly, among the 204 patients initially classified as intermediate-low risk, 30 (14.7%) patients were reclassified to the low-risk category. This visual representation underscores how the revised hsTnT threshold redistributes the patients into distinct risk categories. The reclassification led to a substantial increase in the mortality rate within the intermediate-high-risk group, rising from 4.9 to 9.4%, significantly improving the overall NRI analysis (1.016 ± 0.201, p < 0.001).
DISCUSSION
Our findings can be summarized as follows: (1) an hsTnT level of ≥ 60 ng/L was associated with an elevated risk for PE-related adverse outcomes and all-cause mortality following the diagnosis of acute PE; (2) hsTnT demonstrated additive value when integrated into a combined model with sPESI ≥ 1; and (3) in comparison to the conventional hsTnT level of 14 ng/L, an hsTnT level of 60 ng/L proved to be a more effective indicator in risk stratification.
Pitfalls and new proposals in hsTnT for risk stratification in acute PE
The prognostic significance of cardiac troponin levels in patients diagnosed with PE has been increasingly recognized. The conventional troponin I or T assay is the standard for detecting myocardial injury, which relies on elevated levels that exceed the 99th percentile URL. However, the landscape of troponin testing underwent a transformative shift with the introduction of hsTnT in 2009 [4], which significantly improved detection sensitivity, revealing troponin levels previously undetectable in earlier assays. Including hsTnT in the 2019 ESC guidelines emphasize its crucial role in risk stratification, particularly in intermediate- and low-risk patients. However, considerable uncertainty remains regarding the clinical utility of adopting the 99th URL in identifying patients who may be at an increased risk of short-term complications precisely, as the guideline does not explicitly outline the extent to which such elevations should be deemed clinically significant. Therefore, it is imperative to establish an optimal threshold instead of relying solely on the conventional hsTnT level of 14 ng/L. Jiménez et al. [6] initially validated hsTnT combined with the sPESI score to predict adverse outcomes in hemodynamically stable PE patients, using the 14 ng/L cut-off. They reported that while this cut-off level was useful for risk stratification, there was a need for more specific values tailored to PE patients to improve prognostic accuracy and clinical utility. Lankeit et al. [7,8] and others [9–13] applied an hsTnT level of 14 ng/L and demonstrated high prognostic sensitivity and NPV for the 30-day mortality risk. Although this threshold has been widely used for risk stratification and identifying patients suitable for early discharge, its initial intent was to distinguish between normal and elevated biomarker levels in coronary artery disease rather than in the specific context of PE [14]. In addition, almost two-thirds of patients presented with hsTnT ≥ 14 ng/L upon admission, leading to low specificity and PPV of the biomarker [7]. In contrast to previous studies using hsTnT, our findings indicate the clinical need for a new cut-off value. The new cut-off level of 60 ng/L exhibits remarkable performance, providing moderate specificity (71.0%) and a robust NPV (94.0%) for predicting PE-related adverse outcomes as well as all-cause mortality. This higher threshold allows for more precise risk stratification and enables targeted therapeutic interventions, potentially improving patient outcomes. While the AUC significantly increased compared to hsTnT at 14 ng/L, accompanied by a substantial change in the mortality rate within the intermediate-high risk group in the reclassification analysis, concerns may arise regarding improvement of PPV at the expense of NPV and sensitivity when adopting an hsTnT cut-off level of 60 ng/L, as opposed to the conventional 14 ng/L. This shift could lead to overlooking many at-risk patients. However, a lower hsTnT cut-off level with elevated sensitivity may result in more false positives, leading to unnecessary hospital admissions, testing, and treatments for patients not significantly at risk of adverse outcomes. While it may seem counterintuitive to sacrifice NPV to increase PPV, in the context of acute PE management, accurately identifying high-risk patients who need immediate intervention is paramount. Additionally, a combined model with sPESI ≥ 1 was identified as a particularly valuable tool for prognostic purposes. Standardized cut-off levels for different troponin assessment methods should be established in future studies involving broader patient selection.
Factors influencing hsTnT variability
Advanced age is commonly associated with chronic comorbidities that may contribute to elevated baseline hsTnT levels. The discussion of age-dependent troponin levels has been extensive in various studies conducted in acute and non-acute settings [15–19], with debates as to whether these increases are pathological or physiological [17,20,21]. In 2014, Kaeberich et al. [22] proposed a cut-off level of 45 ng/L for predicting adverse 30-day outcomes in patients aged ≥ 75 years while maintaining a level of 14 ng/L for patients aged < 75 years. In our study, a noteworthy elevation in the threshold level of hsTnT was observed, also set at 60 ng/L, specifically for predicting all-cause mortality in patients aged 75 years and older. However, it is important to note that, as of now, age-dependent cut-off levels are not recommended for clinical use [23].
These recommendations propose utilizing sex-specific 99th percentiles for identifying myocardial injury [4,24]. In our study, no significant difference was observed between male and female patients (33.0 ng/L [IQR 15.0–72.0 ng/L] vs. 30.0 ng/L [IQR 15.0–81.0 ng/L]; p = 0.676). Even after adjusting for age and sex in the multivariable model, hsTnT levels ≥ 60 ng/L remained significant in predicting clinical outcomes, underscoring the strength of their association with the observed outcomes.
A role of NT-proBNP as a biomarker in risk stratification
Like cardiac troponins, elevated NT-proBNP levels may occur because of RV strain caused by the increased pulmonary artery pressure associated with acute PE [25,26]. Meta-analyses of 12 studies conducted by Klok et al. [27] and 23 studies by Lega et al. [28] demonstrated that higher NT-proBNP levels were associated with an elevated risk of adverse outcomes, with all-cause mortality being a significant factor. However, despite its established prognostic value, the role of NT-proBNP has not yet been integrated into guiding treatment decisions in the context of randomized controlled trials as per the 2019 ESC guidelines. While an NT-proBNP cut-off level of 600 pg/mL has been recommended as the optimal concentration to distinguish low and intermediate risks of adverse outcomes and all-cause mortality within 30 days [29], our multivariable analysis demonstrated that it was only significantly associated with all-cause mortality; it did not emerge as an independent predictor of PE-specific adverse outcomes. Possible reasons for this disparity could include the dynamics of NT-proBNP release, variations in patient characteristics, comorbidities, and the presence of other clinical conditions that may not have been fully captured in the proposed cut-off. Therefore, precise evaluation of hsTnT as a prognostic factor for PE is crucial.
Limitations
This study had several limitations. First, it was a single-center retrospective study with a limited number of patients, which may affect the generalizability of the results. Further investigations with larger cohorts are necessary to validate these findings. Second, the inclusion of SBP < 90 mmHg in the PE-related adverse outcomes could potentially lead to confounding results owing to their elevated baseline risk in these patients. In high-risk patients, low SBP at admission is indeed a critical marker of hemodynamic instability and simultaneously an adverse clinical outcome in this study. The majority of PE-related adverse outcomes in high-risk patients occurred in those with low SBP at admission. reinforcing the need for immediate therapeutic interventions in this subgroup to mitigate potential adverse outcomes. This study referenced previous works [13,30] that included hypotension or “need vasopressor” as an adverse outcome. Furthermore, being retrospective in design, the reflects the results of preventing the risk of death through appropriate thrombolytic therapy in the early hemodynamic instability state; therefore, a criterion of SBP < 90 mmHg was added to the adverse outcomes. Third, the study’s reliance solely on initial hsTnT levels may pose a limitation, as it remains unclear whether peak levels or serial follow-ups offer additional insights. Furthermore, excluding comorbidities may not be comprehensive, especially if some conditions are subclinical. Some study patients may have had significant coronary artery disease, which could have potentially affected the specificity of the troponin levels.
Conclusion
Our results confirmed the prognostic value of defined hsTnT level of 60 ng/L in patients with acute PE. Patients surpassing this cut-off level exhibited a heightened risk of both PE-related adverse outcomes and all-cause mortality within 30 days. With the implementation of this new threshold, patients initially classified as intermediate-high or intermediate-low risk may have a lower risk. Early identification and stratification of patients using hsTnT testing can offer valuable insights into personalized and timely management interventions.
KEY MESSAGE
1. The receiving operating characteristics analysis identified an optimal hsTnT cut-off level of 60 ng/L for predicting all-cause mortality within 30 days (AUC 0.74, 95% CI 0.61–0.85, p < 0.001).
2. The combined model of hsTnT ≥ 60 ng/L and sPESI ≥ 1 provided additive prognostic information.
3. Compared to the conventional hsTnT level of 14 ng/L, an hsTnT level of 60 ng/L demonstrated superior efficacy in risk stratification.
Notes
CRedit authorship contributions
Moojun Kim: conceptualization, methodology, investigation, data curation, formal analysis, writing - original draft, writing - review & editing; Chang-Ok Seo: investigation, data curation; Yong-Lee Kim: investigation, data curation; Hangyul Kim: data curation, validation; Hye Ree Kim: data curation, validation; Yun Ho Cho: formal analysis, visualization; Jeong Yoon Jang: formal analysis, visualization; Jong-Hwa Ahn: formal analysis, visualization; Min Gyu Kang: data curation, validation; Kyehwan Kim: writing - review & editing; Jin-Sin Koh: writing - review & editing; Seok-Jae Hwang: writing - review & editing, supervision; Jin Yong Hwang: writing - review & editing, supervision; Jeong Rang Park: conceptualization, methodology, investigation, validation
Conflicts of interest
The authors disclose no conflicts.
Funding
None