Cancer treatment-induced bone loss
Article information
Abstract
Cancer treatment-induced bone loss (CTBL) is associated with anti-tumor treatments, including endocrine therapies, chemotherapeutic treatments, radiotherapy, glucocorticoids, and tyrosine kinase inhibitors. Osteoporosis, characterized by the loss of bone mass, can increase the risk of fractures, leading to mortality and long-term disability, even after cancer remission. Cancer and osteoporosis have marked clinical and pathogenetic similarities. Both have a multifactorial etiology, affect the geriatric population, and markedly influence quality of life. Lifestyle management, including calcium and vitamin D supplementation, is recommended but the supporting evidence is limited. Oral and injectable bisphosphonates are effective for osteoporosis and malignant bone disease. Bisphosphonates increase bone mineral density (BMD) in patients with CTBL. Denosumab is also used in the management of CTBL; in clinical trials, it improved BMD and reduced the risk of fracture. Currently, there are no bone anabolic therapies for patients with cancer. Appropriate therapies are necessary to maintain optimal bone health, particularly in patients at heightened risk.
INTRODUCTION
The life expectancy of patients with cancer has been increased by advances in diagnostics and treatment resulting from an increased understanding of cancer biology. However, long-term therapeutic interventions typically have a high incidence of lasting adverse effects, which can substantially diminish the quality of life and have notable social and economic ramifications. Cancer treatment-induced bone loss (CTBL) is frequently associated with anti-tumor treatments [1].
Breast and prostate cancer are frequently linked to therapeutic interventions that affect bone metabolism [2]. The latest position statement issued by eight esteemed international societies states that women prescribed aromatase inhibitors (AIs) are at risk for fracture comparable to individuals on glucocorticoids (GCs) [3]. Chemotherapeutics reduce bone mass by direct mechanisms, such as disruption of osteoblast (OB) and osteoclast (OC) function and differentiation. In addition, indirect effects may be caused by chronic renal disorders, electrolyte imbalances, and hypogonadism. Promotion of the apoptosis of OBs and osteocytes, as well as the accelerated differentiation of bone marrow stromal cells into adipocytes, are among the supplementary mechanisms [4,5]. Radiotherapy (RT), GCs, and tyrosine kinase inhibitors (TKIs) have deleterious effects on bone health [1]. Immune checkpoint inhibitors (ICIs) have transformed the management of advanced solid tumors [6]. However, a considerable proportion of patients manifest severe immune-related adverse events (irAEs) [7]. ICIs may have an adverse effect on bone metabolism [8]. Osteoporosis, characterized by loss of bone mass, can increase the risk of osteoporotic fracture. These fractures are linked to fatal outcomes and can result in disability that persists after recovery [9]. Therefore, severe bone loss can occur during cancer treatment and persist after cancer remission. Consequently, patients who experience a fracture after cancer treatment may have to cope with permanent disability [10].
PATHOPHYSIOLOGY OF CTBL (Fig. 1)

Pathophysiology of cancer treatment-induced bone loss. ICIS, Immune checkpoint inhibitor; TKI, tyrosine kinase inhibitor.
Bone metabolism
The skeletal system undergoes physiological remodeling, which is facilitated by the harmonious functioning of OCs and OBs. OCs are large syncytial cells originating from monocytes/macrophages that mediate bone resorption by releasing enzymes, including cathepsin K, phosphatase, and collagenase. OBs are derived from mesenchymal stem cells and fill the cavities formed by OCs. They deposit morphogenic bone proteins in the mineralized matrix [11]. Following bone formation, they adopt a flattened morphology and enter a quiescent state. Subsequently, a subset of them becomes embedded in the mineralized bone matrix, assuming the identity of OCs. Based on their extensive dendritic network, OCs can detect mechanical stimuli and release mediators that regulate bone formation and resorption [12].
Systemic and local factors maintain the bone balance, particularly the receptor activator of the nuclear factor kB-ligand (RANKL)/RANK/osteoprotegerin (OPG) axis. The production of TNF-related RANKL is attributed to the activity of OBs and stromal cells. RANKL activates the nuclear factor-kB and Jun N-terminal kinase pathways, thereby facilitating the differentiation of osteoclast precursors. Following the binding of RANKL, OBs secrete OPG, which decoys RANKL and prevents the formation of OCs and bone resorption. Local factors such as IL-6, IL-1, M-CSF, and prostaglandins stimulate the growth and activity of OCs. However, inhibitors of osteoclastogenesis such as IL-4, IL-18, and IFN-c counteract these pro-osteoclastogenic factors [13].
Several systemic factors influence calcium and bone turnover. Parathyroid hormone (PTH) regulates the calcium level in blood and stimulates OB to release cytokines that promote OC growth and activity. Dual hydroxylation in the hepatic and renal systems results in the formation of 1–25-dihydroxy vitamin D, thereby promoting intestinal calcium and phosphate absorption [14].
Estrogen receptors (ERs) on OBs and OCs regulate bone resorption by stimulating OPG, IGF-1, and TGF-β synthesis by OBs and blocking pro-osteoclastogenic factors. This interaction promotes bone growth and reduces resorption. Testosterone indirectly regulates bone turnover by increasing OB proliferation and suppressing apoptosis after aromatization into estradiol. Estrogens and androgens decrease the levels of pro-osteoclastogenic cytokines such as IL-6 [15,16].
GCs may cause bone resorption. Indirectly, they decrease intestinal calcium absorption and stimulate calcium excretion in urine, lowering the serum level of calcium and increasing PTH synthesis. GCs decrease osteoblastogenesis, reducing bone cell formation and damaging bone health by having cytotoxic effects on OBs and OCs, which are crucial for maintaining bone integrity [17].
Cancer and osteoporosis have notable clinical and pathogenetic similarities. Both conditions primarily impact the geriatric population and have a multifactorial etiology that includes chronic inflammatory pathologies. The presence of cancer and subsequent therapeutic interventions significantly decrease quality of life via a combination of psychophysical deterioration and a notable decline in mobility. Osteoporotic bone creates an environment conducive to the proliferation and colonization of metastatic cancer cells, thereby establishing a deleterious cycle [1].
Endocrine therapy for breast cancer and bone loss
Endocrine therapy for breast cancer primarily impedes the transmission of estrogen signals in estrogen-dependent breast cancer cells by inhibiting estrogen production or obstructing ER binding sites [18]. For premenopausal patients, it is typically advised to administer tamoxifen or an AI (letrozole, anastrozole, or exemestane) with or without a luteinizing hormone-releasing hormone (LHRH) agonist (goserelin or leuprorelin). Conversely, for postmenopausal patients, it is recommended to administer an AI for 5 years (with an option of an additional 3–5 yr) or tamoxifen for 2–3 years, followed by an AI for 2–3 years (or 5 yr) [19]. Cyclin-dependent kinase (CDK) 4/6 inhibitors, namely, palbociclib, abemaciclib, or ribociclib, in combination with endocrine treatment, have promising outcomes for patients with metastatic breast cancer [20]. Furthermore, the efficacy of adjuvant therapy (AI with abemaciclib) confers marked benefits [21].
Tamoxifen has been the preferred treatment option for over three decades and is the gold standard for managing hormone receptor-positive early-stage and advanced breast cancer; it has agonistic and antagonistic effects on ERs. It protects the skeletal system of postmenopausal women while having a detrimental effect on their bone health. In one study, tamoxifen resulted in a decrease in 2.76% in lumbar spine bone mineral density (BMD) and 4.27% in total hip BMD in premenopausal women [22]. Conversely, postmenopausal women on tamoxifen experienced a 4.65% increase in BMD in the lumbar spine and 3.58% increase in the hip. In another study, tamoxifen was associated with an elevated risk of fracture in premenopausal women diagnosed with breast cancer [23].
AIs reduce the estrogen level in postmenopausal women. In one study, AIs performed better than tamoxifen for treating advanced and early breast cancer [24]. In another study, an LHRH agonist was effective against breast cancer in premenopausal patients [25]. AIs also substantially reduce estrogen levels in bone, resulting in osteoporosis [26]. In most controlled studies involving postmenopausal patients [27–29], adjuvant therapy led to an increased fracture rate. In a meta-analysis of seven randomized studies [30], AI therapy increased the fracture risk by 47% compared to tamoxifen. In a recent meta-analysis of 30 trials, the rates of osteoporotic fractures increased by 35%, hip fractures by 18%, vertebral fractures by 84%, and nonvertebral fractures by 18% [31]. In a 5-year the Arimidex, Tamoxifen, Alone or in Combination (ATAC) study of anastrozole and tamoxifen, anastrozole was associated with a fracture frequency of 5.9% in the first year, compared to 3.7% for tamoxifen [32]. In a substudy, the 5-year BMD in patients on tamoxifen was minimally changed or slightly elevated (LS +2.8%, femur +0.7%) but linearly decreased with anastrozole (LS −6.1%, femur −7.2%) [27].
Several studies that have compared extended long-term AI use to placebo or no medication have revealed increases in disease-free life expectancy and fracture risk; one showed that treatment with AI for 2.5–5 years increased the risk of fracture by 34% [33].
Bilateral oophorectomy has been used to treat premenopausal breast cancer for more than a century. Goserelin and leuprorelin, which are LHRH agonists, also inhibit ovarian function. In one study, after 2 years, the BMD decreased in premenopausal patients with breast cancer by 0.3% without therapy, 1.5% with tamoxifen alone, 1.4% with goserelin + tamoxifen, and 5.0% with goserelin alone [34]. An LHRH agonist with AI degrades the bone microarchitecture [35]. An LHRH agonist alone or combined with tamoxifen does not increase the fracture risk. In one study, an LHRH agonist + AI resulted in greater bone loss than LHRH + tamoxifen in premenopausal women (13.6% vs. 9% after 3 yr) [36] but no increase in fractures. The TEXT and SOFT studies showed that an LHRH agonist with AI (exemestane) exacerbated osteoporosis (38.6% vs. 25.2%) and increased fractures (6.8% vs. 5.2%) compared to LHRH plus tamoxifen [37].
ER-induced cell cycle progression requires a CDK4/6 signal; hence, CDK4/6 inhibitors and endocrine therapy are used to treat advanced and early breast cancer [8,9]. There is no clinical evidence on the effects of CDK 4/6 inhibitors and bone metabolism. Iuliani et al. [38] reported that three CDK4/6 inhibitors suppressed OC differentiation and reduced the levels of bone resorption markers but did not affect OB activity in vitro.
Endocrine therapy for prostate cancer and bone loss
Androgen deprivation therapy (ADT) for prostate cancer induces marked bone loss. LHRH agonists are the standard ADT, replacing surgical orchiectomy. Combined androgen blockade or maximal androgen blockade in conjunction with an antiandrogen drug is a common therapeutic strategy. Drugs recently approved for metastatic or non-metastatic castration-resistant prostate cancer (CRPC) [39] include the CYP17 inhibitor abiraterone acetate and second-generation AR antagonists (enzalutamide, apalutamide, and darolutamide). In combination with ADT, certain medications have been approved for the treatment of metastatic castration-sensitive prostate cancer. Androgens also affect bone cells containing AR. The AR signal stimulates OB proliferation and inhibits apoptosis and OC bone resorption. A low testosterone level leads to an elevated RANKL level and bone resorption [40]. In a study on patients with prostate cancer, ADT decreased bone density by 2–5% in the lumbar spine and 1.5–2.5% in the femoral neck [18]. BMD decreases early in patients with ADT but declines significantly after 10 years compared to after 2 years [41].
In a retrospective analysis of 50,613 individuals [42], ADT-treated patients with prostate cancer had a fracture frequency of 19.4% compared to 12.6% for those on placebo. In a cohort study of 179,744 Swedish men, treatment of prostate cancer with ADT increased the incidence of any fracture and hip fracture. ADT-free patients with prostate cancer did not have an increased risk of fracture [43]. In a cohort study, fracture risk increased with ADT treatment duration (significant for > 1 yr; not significant for 1 yr) [44]. In another study, long-term treatment with ADT (> 1 yr) increased the fracture risk in patients with prostate cancer without metastases [45].
There is little information on the effects of novel AR-targeting agents on bone. In preclinical studies, abiraterone has been found to inhibit OC differentiation, as does ADT + abiraterone [46,47]. Enzalutamide decreases axial but not appendicular bone mass in male rodents [48]. In a study on patients with non-metastatic CRPC, apalutamide increased the fracture rate (11.7% vs. 6.5%) and decreased the metastatic risk (40.5 vs. 16.6 mo) [49]. In another study, compared to placebo, darulotamide improved metastasis-free survival (40.4 vs. 18.4 mo) but did not increase the fracture rate (4.2% vs. 3.6%) [50]. In a third study, enzalutamide-treated patients had more fractures (10% vs. 5%) and longer survival without metastasis (36.6 vs. 14.7 mo) [51]. The fracture risk associated with abiraterone and non-metastatic CRPC is unknown.
Chemotherapies
Antineoplastic medications with renal toxicity can indirectly have detrimental effects on the skeletal system [1]. Platinum compounds, notably cisplatin, accumulate in the renal cortex and damage proximal tubules, causing kidney failure. Cisplatin is associated with electrolyte imbalances, specifically acute and chronic hypomagnesemia, which can have detrimental effects on bone health [52]. A retrospective analysis based on dual-energy X-ray absorptiometry (DXA) data was conducted to examine the bone health of premenopausal women who underwent bilateral oophorectomy for benign pathologies or gynecological cancers [53]. The prevalence of bone deterioration was markedly increased among women who received cisplatin compared to those who underwent ovariectomy for benign pathologies. However, in an open-label randomized phase 3 trial that compared first-line cisplatin plus gemcitabine to paclitaxel plus gemcitabine in patients with triple-negative breast cancer, 1 of 118 patients on cisplatin plus gemcitabine developed a pathological bone fracture [54].
Ifosfamide, a nephrotoxic chemotherapeutic agent, can induce tubular damage, resulting in glycosuria and the excretion of electrolytes, amino acids, and low-molecular-weight proteins. In severe cases, this can cause Fanconi syndrome, which is common in pediatrics and can have long-term consequences, including rickets and growth retardation [55].
Cyclophosphamide, a potent inducer of premature ovarian failure, produces its effects through the metabolite phosphoramide mustard. This metabolite damages ovarian follicles in a dose-dependent manner [56]. Cyclophosphamide directly impacts bone turnover by inhibiting the division of pre-OBs and OCs, thereby suppressing bone formation and resorption [55].
Doxorubicin may affect bone health by inducing OC differentiation and reducing the formation of fibroblasts and OBs derived from BMSCs, as demonstrated in an in vitro study [57]. The effects are influenced by oxidative stress, as indicated by the downregulation of superoxide dismutase. An anti-TGF-β antibody can partially counteract these effects, indicating hyperactivation of the TGF-β pathway in cells treated with doxorubicin. In a preclinical murine model of breast cancer, doxorubicin markedly reduced the total bone volume (TBV) and increased the levels of serum markers of bone resorption. These phenomena were also observed in mice without tumors, indicating that the impairment of bone health was not influenced by the presence of tumors [57]. Doxorubicin may compromise bone health by inducing ovarian failure in a dose-dependent manner [58].
Methotrexate, a competitive inhibitor of dihydro-folate reductase, inhibits BMSC-to-OB differentiation [56] and OB proliferation in vitro. In vivo, MTX-treated adult rats have decreased metaphyseal TBV and increased marrow adipose mass. The upregulation of pro-adipogenic transcription factors in BMSCs leads to a decrease in their osteogenic differentiation potential and an increase in their adipogenic differentiation potential [59]. MTX inhibits the canonical wingless (Wnt)/β-catenin pathway, which regulates BMSC commitment and bone degradation. An increased Wnt antagonist mRNA level and decreased nuclear β-catenin level are observed in BMSCs. In rodents treated with MTX, a glycogen synthase kinase-3b inhibitor and an activator of Wnt/β-catenin signaling can partially reverse these effects and decreased marrow adiposity [60]. MTX also increases the caspase-3 level and causes retraction of dendritic processes in osteocyte-like MLO-Y4 cells. In mononuclear precursors grown in medium from MTX-treated MLO-Y4 cells, MTX-exposed osteocytes stimulate OC development via MCSF and RANKL. In vivo, rodents administered a high dose of MTX show increased osteocyte mortality in the metaphyses of long bones and an increased number of OCs in trabecular bone [61]. This pro-OC effect may be mediated by increased levels of pro-inflammatory cytokines (TNF, IL-1, IL-6), as determined by real-time PCR and ELISA in bone and plasma of MTX-treated animals [62]. Long-term therapy with high-dose MTX for inflammatory diseases such as rheumatoid arthritis causes damage to bone [63].
GCs
In onco-hematology, GCs are used in chemotherapy regimens and as analgesics and antiemetics, and in the long-term can cause iatrogenic osteoporosis [64]. GCs damage trabecular bone, causing rapid BMD loss because of bone resorption and delayed demineralization as a result of reduced OB activity [65]. Patients with primary and secondary brain tumors require ongoing GC therapy to ameliorate neurological sequelae and peritumoral edema [66].
Several chemotherapy regimens, notably for lymphomas and multiple myeloma, use substantial dosages of GCs [1]. A prospective single-center study examined BMD in lymphoma patients at baseline and 1 year after starting chemotherapy and prednisone. Four patients (12.5%) developed new osteoporotic fractures during follow-up, and female sex, lower creatinine clearance, alkaline phosphatase (ALP) and albumin levels at baseline, a high serum level of calcium, and autologous stem cell transplantation were predictive of fracture [67].
TKIs and ICIs
Targeted therapy has higher efficacy and lower toxicity than chemotherapy [68,69]. TKIs compete with the adenosine triphosphate-binding site in the catalytic domain of oncogenic tyrosine kinase [70]. Imatinib selectively inhibits the kinase breakpoint cluster region-Abelson (BCR-ABL), which is constitutively active in 40–90% of patients with chronic myeloid leukemia (CML) as a result of Philadelphia chromosome development [71]. Imatinib is the gold standard treatment for gastrointestinal stromal tumors (GISTs) in patients with the c-KIT gene mutation in exon 9 or 11 [72,73] and is approved as a high-risk post-surgery adjuvant therapy and first-line treatment for metastatic GIST [74].
The effect of imatinib on bone turnover is controversial. One study found that inhibiting the MCSF receptor c-KIT, carbonic anhydrase II, and platelet-derived growth factor receptor (PGFR) enhanced bone strength and TBV but decreased OC differentiation and activity. This medication may cure osteomalacia and osteoporosis because downregulation of the PGFR pathway activates OB and induces bone matrix deposition [75,76]. However, a previous study found that imatinib reduced TBV and the serum level of osteocalcin in healthy rats [77]. A prospective study showed that BMD decreased in 28 patients with CML or GIST [78] but the levels of bone turnover markers (osteocalcin, bone ALP, and serum N-terminal telopeptide) were unaffected. In another clinical study, imatinib-treated patients had hypocalcemia, D hypovitaminosis, secondary hyperparathyroidism, hypophosphatemia, and elevated fracture risk [79].
New TKIs may affect bone metabolism. Sorafenib, sunitinib, vandetanib, and cabozantinib inhibit OB differentiation in vitro and RANKL synthesis, which is necessary for OC activation. Dasatinib, another BCR-ABL inhibitor, inhibits Rous sarcoma kinase, which regulates OC differentiation and bone resorption [80].
Exploratory analyses in the BOLERO-2 trial showed that everolimus combined with exemestane for HR+ breast cancer spared bone [81]. Mammalian target of rapamycin inhibitors are used clinically for neuroendocrine tumors and kidney and breast cancers. Everolimus directly prevents bone resorption in vitro and in vivo [82].
ICIs have improved the prognosis of patients with metastatic cancer by increasing cytotoxic T-cell activity via the programmed cell death protein 1/programmed cell death ligand 1 axis [6]. IrAEs are associated with ICIs due to an overactive immune system. These toxicities can affect all host tissues [7], although only a few small case series that have evaluated their effects on the skeleton have been published [83,84]. These studies have reported significant vertebral fractures in patients with ICI, some in numerous locations. The level of C-terminal telopeptide I (CTX-I), a bone resorption marker, is increased, accompanied by a concurrent declining pattern in the reduction of procollagen type 1 N-terminal propeptide, a bone formation marker, following 3 months of ICI treatment. Interestingly, an increased CTX-I level is associated with an unfavorable prognosis in terms of both treatment response and overall survival. There are correlations among ICIs, heightened osteoclast function, and increased susceptibility to fracture [8].
Radiotherapy/radiometabolic treatment
Indirect effects such as iatrogenic hypogonadism, hyperparathyroidism, electrolyte disorders, direct toxicity from OB/OC imbalance, periarticular fibrosis, and cartilage degeneration cause RT-induced bone damage [85]. After external- beam RT to the pelvis for urological and gynecological malignancies, gonadal damage [55] and bone toxicity can cause fracture. A retrospective cohort analysis of 6,428 women aged ≥ 65 years undergoing pelvic RT for cervical, anal, or rectal cancer reported a significantly increased risk of fracture, mainly at the hip [86]. However, a recent study of 8,507 women exposed to radiation for gynecological cancers found no increased risk for total hip arthroplasty compared to patients with breast cancer [87].
Based on in vivo studies showing an increased incidence of parathyroid adenomas in irradiated animals, several retrospective reports have indicated the emergence of hyperparathyroidism after head-and-neck irradiation [88]. In childhood malignancies, the effect of RT on BMD has been studied. Growth hormone deficit caused by cranial irradiation- induced disruption of the hypothalamic-pituitary axis may lower BMD and affect sex hormone release [89].
MANAGEMENT OF CTBL
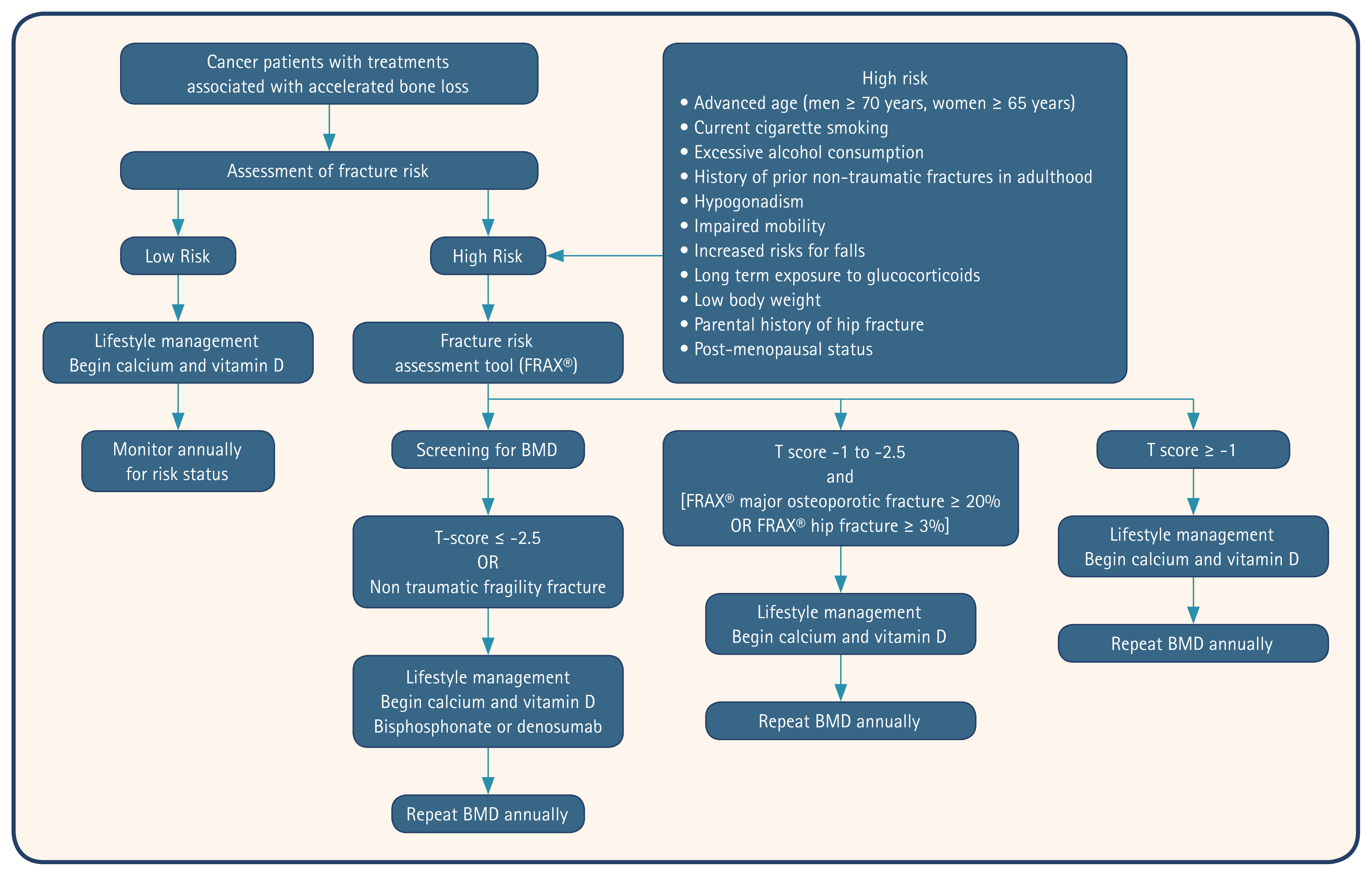
Assessment of fracture risk
It is recommended to assess fracture risk, particularly for patients at high risk for fracture in the context of CTBL. This includes women diagnosed with breast cancer and undergoing treatment with AI and men with prostate cancer receiving ADT [18]. DXA is used to evaluate BMD, for which it is the gold standard diagnostic tool [90]. The FRAX® tool was designed to estimate the 10-year risk of major osteoporotic fracture and in combination with BMD assessment can identify individuals at significant risk for fracture [91]. However, the FRAX® tool was not specifically developed to assess the susceptibility of cancer patients to fracture [92].
Lifestyle management
Most clinical guidelines and recommendations advocate calcium and vitamin D supplementation. However, the available evidence on the efficacy of calcium and vitamin D in CTBL is sparse and inconclusive. In a systematic analysis of clinical trials involving patients with prostate cancer treated with ADT, calcium (500–1,000 mg) and vitamin D (200–500 IU) supplementation did not protect BMD [93]. However, a blood level of 25-OHD < 12 ng/mL increased the fracture risk [94]. Regular resistance training and weight-bearing activity can lead to modest improvement in BMD. However, there is no clear evidence that exercise improves the BMD of patients with cancer [95]. In other medical settings, it is important to motivate and assist patients to cease smoking and decrease alcohol intake, which are risk factors for fractures [90].
Bisphosphonates
Bisphosphonates have long been used to treat osteoporosis and malignant bone disease. Oral and injectable bisphosphonates have received regulatory approval. Few studies have investigated bisphosphonates for preventing bone loss in patients on endocrine treatment. Such studies have been complicated, with patients assigned to treatment groups by BMD, and most have been underpowered for evaluating fracture prevention [2].
Oral bisphosphonates improve BMD in AI patients (Table 1). In a previous study, oral alendronate was examined in 303 postmenopausal breast cancer patients taking anastrozole, stratified by baseline T score [96]. Alendronate enhanced BMD by 15.6% in women with osteoporosis after 3 years. Osteopenic individuals randomly allocated to alendronate had a 6.3% increase in the BMD of the lumbar spine compared to −5.4% in placebo-treated patients. In the SABRE study, oral risedronate was investigated in postmenopausal women with hormone receptor-positive early breast cancer treated with adjuvant anastrozole and a moderate risk for fragility fracture (baseline BMD T-score > −2.0) [97]. Risedronate (35 mg weekly, oral) or placebo was given for 2 years. At 24 months, risedronate increased BMD in the lumbar spine (+2.2% vs. −1.8%) and whole hip (+1.8% vs. −1.1%) compared to placebo.
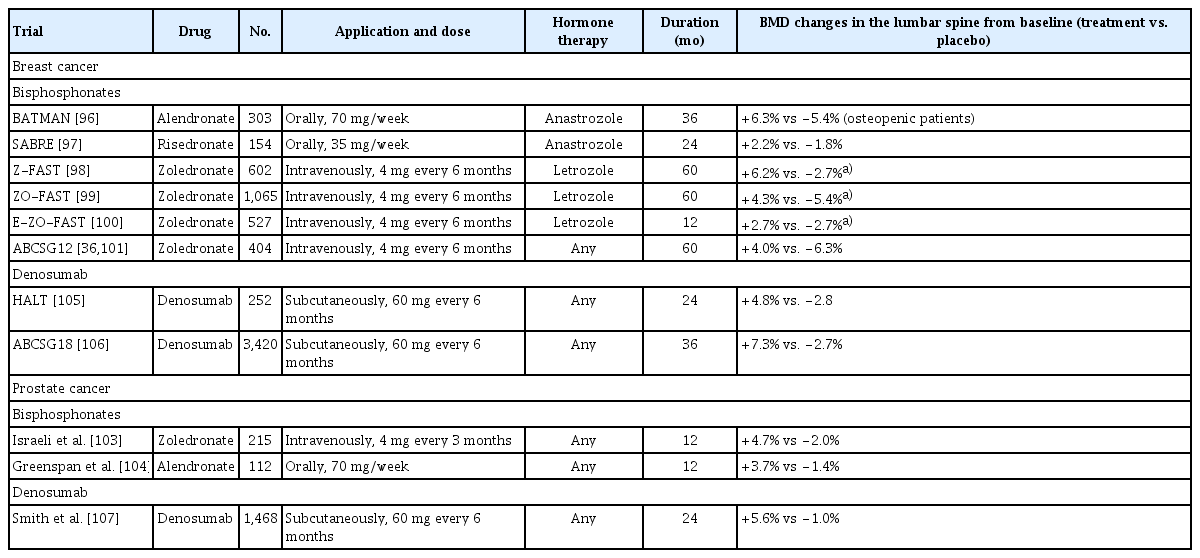
Randomized controlled trials of antiresorptive agents for cancer treatment-induced bone loss in patients with breast and prostate cancer on hormone therapies
Parenteral bisphosphonates can prevent aromatase-induced bone loss in postmenopausal patients with breast cancer (Table 1). Three independent and similarly designed trials (Z-FAST [98], ZO-FAST [99], and E-ZO-FAST [100]) involved postmenopausal women receiving adjuvant letrozole (2.5 mg daily) who were randomly assigned to receive zoledronic acid (4 mg every 6 months) immediately or delayed (until the T-score decreased to < −2.0 or a non-traumatic fracture). In the ZO-FAST trial [99], immediate zoledronic acid increased, whereas delayed zoledronic acid decreased, the BMD of the lumbar spine, resulting in a BMD differential of 5.7% at 24 months. In the ZO-FAST trial [99], the immediate zoledronic acid group showed an increase in BMD of 4.3% at 60 months, compared to a 5.4% decrease in the delayed intervention group. The 5-year Z-FAST study [98] showed that initial zoledronic acid improved BMD by 8.9% in women with early breast cancer. Immediate zoledronic acid was beneficial in the E-ZO-FAST trial [100]. The ABSCG-12 trial [101] examined the benefit of adjuvant intravenous bisphosphonates in premenopausal patients with breast cancer and included a subset analysis of effects on bone (n = 404) [36]. At 2 years after therapy, patients who had not received zoledronic acid had a lower BMD in the lumbar spine (−6.3%) and trochanter (−4.1%) relative to baseline. Zoledronic acid stabilized BMD values after 36 months and enhanced BMD by +4.0% in the lumbar spine and +3.9% in the trochanter at 60 months compared to baseline [36].
In a single-center study in South Korea, BP medication mitigated cortical bone loss at critical sites in the proximal femur in cases of bone loss associated with AIs. Bisphosphonates BP increased the cortical mass surface density at important anatomical sites in the hip region, including the superior aspect of the femur neck and the greater trochanter. The cortical mass surface density increased by up to 15% in these areas [102].
Three studies on CTBL [97,103,104] have failed to demonstrate that bisphosphonates reduce the incidence of fracture during endocrine therapy for breast cancer. However, in the AZURE trial fractures were reduced by postoperative administration of zoledronic acid. The 5-year fracture rate was 3.8% compared to 5.9% in controls [105]. The fracture rate among menopausal patients was 2.93%, compared to 4.23% for controls. A meta-analysis of 3,984 patients across seven studies showed that zoledronic acid reduced the incidence of fracture [106].
Bisphosphonates have been evaluated in endocrine-treated male patients (Table 1). Although small, these trials have consistently shown prevention of BMD loss relative to placebo. In the first year of androgen ablation treatment, zoledronic acid (4 mg every 3 months) increased spine BMD by 4.7% compared to a 2.0% decrease in the placebo group [107]. In one study, the effect of alendronate (70 mg weekly) on androgen deprivation was studied in 112 prostate cancer patients [108]. Over 1 year, alendronate increased the spine BMD by 3.7% compared to 1.4% in the placebo group, and the femoral neck BMD by 1.6% compared to 0.7%. According to an analysis of the phase 2/3 STAMPEDE trial (NCT00268476) presented at the 2023 Annual Meeting of the American Urological Association, patients with metastatic hormone-sensitive prostate cancer who received zoledronic acid had a significantly reduced risk of fracture; zoledronic acid decreased the risk by 64% in patients with metastatic disease. In another study, there were no significant correlations between the administration of zoledronic acid and a decrease in the risk of fracture among patients without metastasized disease [109].
Denosumab
Denosumab, a monoclonal antibody targeting RANKL, is used in the management of osteoporosis at a dose of 60 mg administered via subcutaneous injection every 6 months. In addition, it is used to treat bone metastases at a monthly dose of 120 mg [2]. In a clinical trial (Table 1) that involved approximately 250 patients with reduced bone mass but without osteoporosis who were undergoing AI therapy, the administration of denosumab at 60 mg every 6 months resulted in a significant increase in BMD at the lumbar spine (5.5%) and hip (7.6%) compared to the placebo group [110]. The ABCSG-18 trial [111] (Table 1) compared the effects of denosumab and placebo on fracture incidence among 3425 postmenopausal women diagnosed with breast cancer and undergoing AI therapy. In the denosumab cohort, female patients had a decreased likelihood of clinical fracture compared to those in the placebo cohort. The denosumab group showed a significant reduction in the incidence of vertebral fractures and the progression of existing vertebral fractures for 36 months compared to the placebo group. Fracture rates decreased at all anatomical sites in patients administered denosumab compared to those on placebo. The forearm fracture rate was 2.6% in the denosumab group and 1.5% in the placebo group.
The femur-and-pelvis fracture rate was 1.1% in the denosumab group, compared to 0.3% in the placebo group. The humerus fracture rate was 1.3% in the denosumab group and 0.6% in the placebo group. The fracture incidence was decreased irrespective of the initial T score (< −1 or > −1) or age (< 65 or > 65 yr). There was no reported instance of osteonecrosis of the jaw or atypical femur fracture, and the overall incidence of adverse events was comparable across all groups [111].
The impact of denosumab on fracture occurrence and BMD was evaluated in a placebo-controlled trial [112] involving male patients with prostate cancer undergoing treatment with a GnRH analog (Table 1). After 24 months, the BMD of the lumbar spine increased 5.6% in the denosumab group but decreased 1.0% in the placebo group. The changes were consistent for 36 months, and there were improvements in BMD at all other assessed locations. The incidence of vertebral fractures decreased at 36 months in the denosumab cohort (1.5%) compared to the placebo cohort (3.9%). The incidence of fractures at any anatomical location was nonsignificantly lower in the denosumab group (5.2%) than in the placebo group (7.2%) [112].
Anabolic agents
The therapeutic options are limited to bisphosphonates or denosumab because there are no bone anabolic therapies for use in cancer patients. Despite FDA approval, use of the anabolic bone drugs teriparatide and abaloparatide in patients with cancer is hampered by potential cancer development and recurrence [2]. Other bone anabolic pharmaceutical agents under investigation include monoclonal antibodies targeting the Wnt inhibitors dickkopf-1 and sclerostin [113]. Dickkopf-1 antibodies are under investigation for their effects on metastatic bone disease and myeloma. However, more advanced sclerostin antibodies have not been tested in the context of endocrine therapy-induced osteoporosis [2]. The requirement for bone anabolic medications is unfulfilled in patients experiencing fracture and those at heightened risk for fractures because of endocrine therapy. However, safety should be the priority when considering medications for these individuals. Consequently, well-executed clinical trials addressing this concern are needed.
Guidelines for CTBL
Medical societies and professional organizations have formulated guidelines for the management of women undergoing treatment with AIs. The Expert Group of the United Kingdom has advocated the use of bisphosphonates for women of ages ≥ 75 years with risk factors for osteoporotic fracture irrespective of BMD [114]. Postmenopausal women who have ceased menstruating, who are < 75 years of age, and have a T-score < −2.0 can be started on bisphosphonates. If the rate of bone loss is > 4% annually, bisphosphonates should be considered for women with preexisting osteopenia (T-score −1.0 to −2.0).
A GnRH agonist, in combination with an AI, curtails ovarian function in premenopausal women, thereby accelerating bone demineralization. Bisphosphonates should be considered for patients with a T-score < −1.0. After 24 months, it is recommended that women initially deemed ineligible for bisphosphonate therapy undergo a DXA scan. If they satisfy these criteria (T-score < −1.0), the administration of bisphosphonates is warranted. FRAX® can underestimate the extent of bone loss induced by AIs or other cancer medications. However, the National Comprehensive Cancer Network (NCCN) incorporated FRAX into its guidelines. According to the NCCN recommendations, patients with a 10-year risk of 20% for major fractures or 3% for hip fractures should start on therapy. When the T-score falls below −2.0, treatment is advised [115]. Bisphosphonates and denosumab are recommended as antiresorptive therapies for patients with breast cancer undergoing AI treatment to preserve their bone health.
Seven international societies recommend bone-directed therapy for individuals undergoing treatment with AIs. This recommendation applies to those with a T-score < −2.0 or −1.0 standard deviation and one risk factor. Individuals with two or more risk factors without BMD information should also consider bone-directed therapy [3,116]. Denosumab shows superior efficacy in terms of reducing fractures and bisphosphonates reduce bone metastases by approximately 28%.
In female patients presenting with lumbar spine, femoral neck, or total hip T-scores < 2.5, the American Society of Clinical Oncology (ASCO) recommends the administration of bisphosphonates or denosumab to prevent fracture. Women at heightened risk for osteoporosis-related fracture, as determined by clinical examination or using risk assessment tools, may also be eligible for this therapeutic intervention [117]. Biennial assessment of BMD is imperative.
A CTBL position statement was published by the esteemed Japanese Society for Bone and Mineral Research [118]. This statement pertains to the heightened susceptibility to fracture of CTBL patients and their limited access to therapy per the Japanese Osteoporosis Prevention and Treatment Guidelines. Pharmacological intervention is advised for patients with a BMD T score of −2.0 to −1.5 and those with a familial background of hip fracture and a FRAX® 10-year probability > 15% for major osteoporotic fractures. Drug therapy should be considered for patients with BMD T-scores < −2.0.
The available national and international guidelines do not provide detailed recommendations for managing CTBL in male patients undergoing treatment for PC. According to the Clinical Guidelines of the United Kingdom National Institute for Clinical Excellence (NICE), it is advised to consider the risk of fracture in men undergoing ADT and all patients diagnosed with osteoporosis should receive appropriate treatment [119].
Recommendation
Unfortunately, there are no comprehensive management guidelines for CTBL in South Korea. Given the limited data available on the management of osteoporosis in patients with cancer in South Korea, it is appropriate to consider a dosing schedule similar to that for osteoporosis. The timely recognition and management of CTBL are imperative to mitigate the risk of fracture. Patients should be advised to optimize their calcium and vitamin D intake, engage in regular exercise, and make necessary modifications to their lifestyle behaviors that contribute to bone loss. Patients with high-risk CTBL are recommended to undergo treatment with bisphosphonate (administered orally or via injection) or denosumab. Patients at risk for CTBL should undergo annual monitoring of BMD (Fig. 2).
CONCLUSIONS
The increased survival rates of patients with cancer has heightened the importance of maintaining optimal bone health. Several cancer treatments influence bone metabolism, mainly by affecting the levels and functions of reproductive hormones. Therefore, it is crucial to maintain bone health, particularly in patients at high risk, and provide appropriate interventions for maintaining bone health.
Notes
Conflicts of interest
The author discloses no conflicts.
Funding
This study was supported by grants from the National Research Foundation, Korea (NRF-2022R1C1C1006818).