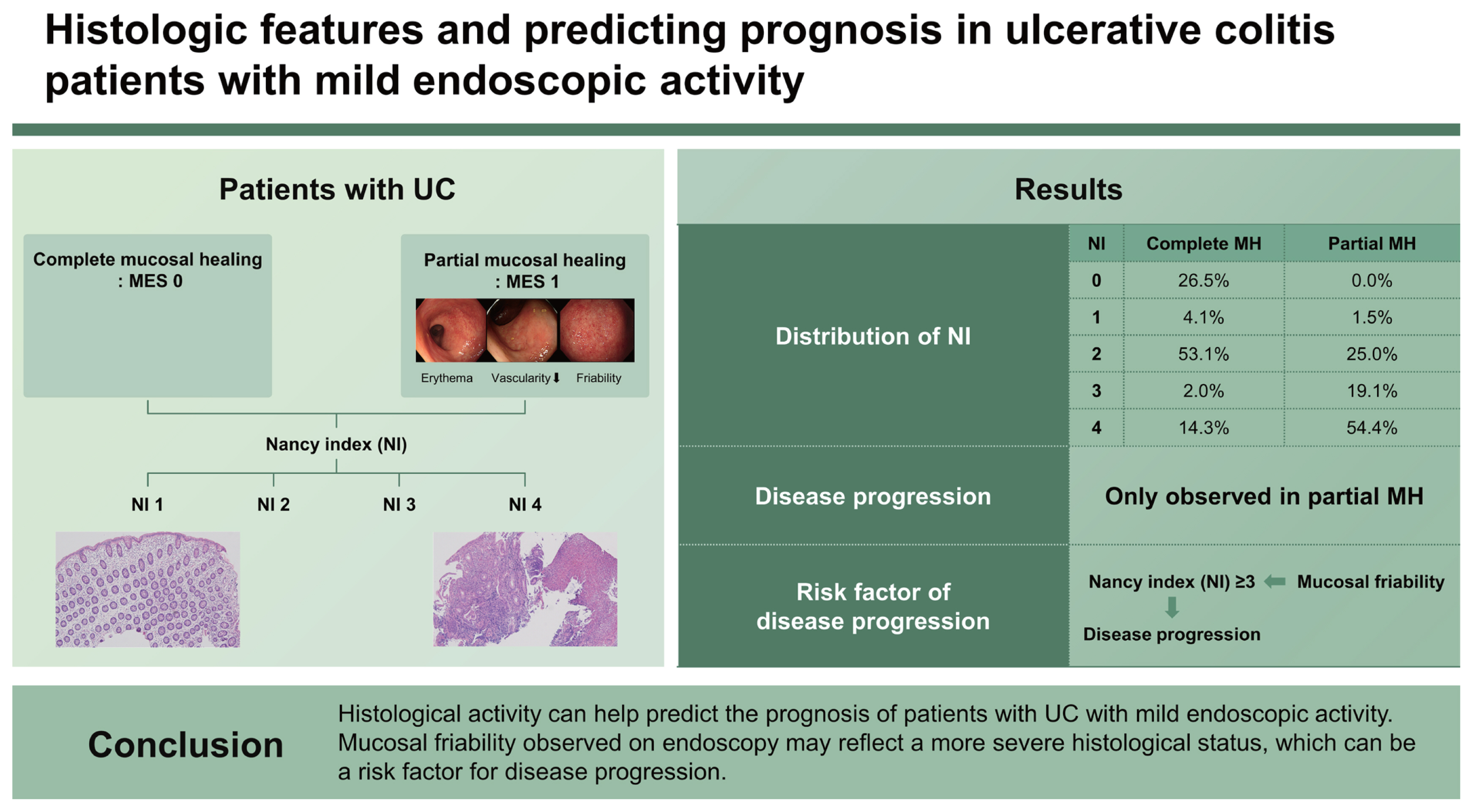
Histologic features and predicting prognosis in ulcerative colitis patients with mild endoscopic activity
Article information
Abstract
Background/Aims
We aimed to evaluate the histologic features predictive of prognosis and correlate them with endoscopic findings in patients with ulcerative colitis (UC) having complete or partial mucosal healing (MH).
Methods
We prospectively collected and reviewed data from patients with UC who underwent colonoscopy or sigmoidoscopy with biopsy. Complete and partial MH were defined as Mayo endoscopic subscores (MESs) of 0 and 1, respectively. Histologic variables, including the Nancy index (NI), predicting disease progression (defined as the need for medication upgrade or hospitalization/surgery), were evaluated and correlated with endoscopic findings.
Results
Overall, 441 biopsy specimens were collected from 194 patients. The average follow-up duration was 14.7 ± 7.4 months. There were 49 (25.3%) and 68 (35.1%) patients with MESs of 0 and 1, respectively. Disease progression occurred only in patients with an MES of 1. NI ≥ 3 was significantly correlated with disease progression during follow-up. Mucosal friability on endoscopy was significantly correlated with NI ≥ 3 (61.1% in NI < 3 vs. 88.0% in NI ≥ 3; p = 0.013).
Conclusions
Histological activity can help predict the prognosis of patients with UC with mild endoscopic activity. Mucosal friability observed on endoscopy may reflect a more severe histological status, which can be a risk factor for disease progression.
INTRODUCTION
Ulcerative colitis (UC) is a chronic inflammatory bowel disease characterized by both relapses and remissions [1]. Currently, several available treatment options exist, and clinical decision-making to determine the appropriate medical therapy is based mainly on clinical and endoscopic assessments [2,3]. It is generally accepted that clinical response, i.e., improvement of rectal bleeding and stool frequency, is a short-term treatment goal in patients with UC; endoscopically visualized mucosal healing, in contrast, is a reasonable long-term treatment target [4,5]. Together with the normalization of C-reactive protein (CRP), erythrocyte sedimentation rate, and fecal calprotectin levels [5,6], these assessments are used to determine whether a patient with UC should maintain current treatment. With various validated clinical and endoscopic scoring systems available, endoscopic mucosal healing is considered the mainstay of treatment for UC. It is commonly defined as a Mayo endoscopic subscore (MES) [7] of 0 or 1 (more strictly, 0) [8,9]. Achieving endoscopic mucosal healing is associated with lower rates of disease relapse and better long-term outcomes [10–12].
A substantial number of recent studies have focused on histologic activity in patients with UC. It can be an independent risk factor for clinical relapse, hospitalization, colectomy, and neoplasia. Histological remission has been recognized as a potential treatment target, even in patients with UC having endoscopic mucosal healing [4,13–17]. It has also been suggested that histological healing should be assessed for the assessment of deep remission [5]. However, due to a lack of prospective randomized controlled studies, histological remission is still under debate as a reasonable treatment target. Additionally, as histological assessment is both invasive and time-consuming, the cost and risk must be balanced against the added benefit of extending the treatment goal. Although fecal calprotectin is a useful alternative for assessing the degree of inflammation [18], it is not entirely free from these limitations.
As an increasing number of studies have focused on histologic activity, which has become a major area of interest in this disease, the need to address the serious clinical issues listed above has become more apparent. Therefore, this study aimed to evaluate the histologic features predicting clinical outcomes and their relationship with the corresponding endoscopic findings in patients with UC having mucosal healing.
METHODS
Patients and study design
This prospective study was conducted at a single academic institution (Chung-Ang University Hospital, Seoul, Korea). Patients with UC aged >18 years who were regularly followed up and underwent colonoscopy or sigmoidoscopy with biopsy between September 2018 and December 2020 were included. Endoscopic examinations were performed in accordance with the clinical practice. Patients lost to follow-up and those with insufficient data were excluded. The medical records of each enrolled patient, including endoscopic and histological findings, were prospectively collected and analyzed. In this study, UC was diagnosed according to conventional clinical, endoscopic, and histological criteria [19]. Disease progression was defined during follow-up after endoscopic biopsy when a patient was started on immunomodulators, corticosteroids, biologics, or small molecular agents; switched to different biologics or small molecular agents; or underwent a surgical procedure and hospitalization for UC exacerbation.
Written informed consent was obtained from all patients included in the study. This study was approved by the Ethical Committee of Chung-Ang University Hospital (IRB No. 2105-001-19365), and all research was carried out in compliance with the Ethical Principles for Medical Research Involving Human Subjects outlined in the Helsinki Declaration of 1975 (revised in 2013).
Assessment of endoscopic findings
Endoscopic findings were evaluated based on MES [7] using a high-definition magnification colonoscope (CF-HQ290L; Olympus, Tokyo, Japan). MESs of 0 and 1 indicated complete and partial mucosal healing, respectively [20]. For each patient with an MES of 1, typical endoscopic findings of mild disease, such as erythema, decreased vascularity, or friability (the term used to describe mucosa that is easily damaged by direct contact with the endoscope or endoscopic devices), were recorded (Fig. 1). A consensus on activity and each endoscopic finding was achieved by three experienced endoscopists (who performed 500–1000 colonoscopies each year during the 3-year study) working in our department, who were blinded to the patients’ disease status. To minimize interobserver variability, the endoscopists involved in this study met regularly to discuss possible discrepancies.
Assessment of histologic activity
Two or more biopsy specimens were collected from the most severely inflamed area in each segment if several segments of the colon were inflamed. In the case of no inflammation (MES: 0), two biopsy specimens each were collected from the sigmoid colon and rectum. The Nancy index (NI) was used to assess the histological activity. The NI classification ranges from grade 0 (no histologically relevant disease) to grade 4 (severely active disease), according to the presence of ulceration, acute inflammatory cell infiltration, and chronic inflammatory infiltrates [21]. NI enables correlation with the corresponding endoscopic presentation and clinical outcomes by helping classify the UC histologic activity into five domains. In addition to NI, we performed additional histological assessments based on preliminary work, expert opinions, and a literature review. These assessments consisted of eight histological items with good intrareader reliability and interreader reliability (κ value > 0.6) and were the basis for the development of NI [21–23]. Along with the NI parameters (acute inflammatory cells, chronic inflammatory cells, and ulceration), neutrophils in the epithelium or lamina propria, mucin depletion, basal plasmacytosis, and serrated architectural abnormalities (the presence of dilated crypts showing a scalloped lumen) were included (Supplementary Table 1) [21–23]. All histologic assessments were performed by an expert pathologist who had worked as a gastrointestinal pathologist for more than 20 years and was blinded to the endoscopic findings. Representative histological findings at NI 0 and NI 4 are shown in Figure 2. When biopsy specimens from multiple sites displayed variable histology, the highest grade for each histological variable was assessed. All histological parameters, including NI, were assessed to accurately evaluate the severity of inflammation at the time of examination and were then analyzed.

Representative histologic findings of (A) Nancy index of 0 and (B) Nancy index of 4. (A) Biopsy with Nancy index 0 shows only mild degree lymphoplasma cell infiltration in the lamina propria without findings of crypt damage (H&E, ×100) (B) Biopsy with Nancy index 4 shows ulcer, moderate lymphoplasma cell infiltration, mild cryptitis, and moderate crypt distortion (H&E, ×100).
Statistical analyses
All statistical analyses were performed using the SPSS software (version 19.0; IBM Corp., Armonk, NY, USA). Continuous variables are summarized as means ± standard deviations or interquartile ranges, and categorical variables as absolute (n) and relative frequencies (%). Kaplan–Meier curves were used to assess the risk of disease progression throughout the follow-up period. Univariate and multivariate regression analyses were performed to evaluate the histological variables associated with disease progression. Statistical significance was set at p < 0.05.
RESULTS
Baseline characteristics of patients
In total, 194 patients with UC were included in this study. Of these, 49 (25.3%) had an MES of 0 and 68 (35.1%) had an MES of 1. The mean patient age was 44.3 years, and the mean disease duration was 84.7 months. Of the enrolled patients, 58.8% were male. Among the patients, 89.2% received 5-aminosalicylates, and 32.0% received biologics or small molecular agents. The average follow-up period after biopsy was 14.7 ± 7.4 months. The clinical and demographic characteristics of the patients are summarized in Table 1.
Histologic activity index according to endoscopic severity in all patients with UC
Table 2 shows NI according to the MES in patients with UC. Most patients with an MES of 2 or 3 had NIs of 3 or 4. A total of 74.1% of patients with an MES of 2 had an NI of 4, and all patients with an MES of 3 had an NI of 4, indicating a severely active histologic disease. However, mild or more severe histological activity was also observed, even in patients with an MES of 0 or 1. Among the biopsy specimens from 49 patients with an MES of 0, 34 (69.4%) had histological activity consistent with an NI of 2 (mildly active disease). Of the 68 biopsy specimens collected from patients with an MES of 1, 50 (73.5%) had an NI of 3 or 4 (moderately or severely active disease).
Histologic activity and endoscopic findings associated with disease progression in patients with mild endoscopic activity
Of the 117 patients with complete or partial mucosal healing (MES of 0 or 1), 15 (12.8%) experienced disease progression during the follow-up period. None of these 15 patients had an MES of 0, and disease progression occurred only in patients with an MES of 1. Therefore, we analyzed the histological and endoscopic findings related to disease progression in patients with an MES of 1. The average Mayo scores of patients with MES of 0 and 1 were 0.1 ± 0.3 and 3.67 ± 3.4, respectively.
Figure 3 shows the Kaplan–Meier curve of time-to-disease progression stratified by histological activity in patients with an MES of 1. Patients with an NI of 2 (mildly active disease) tended to have a higher rate of disease progression than those with NI ≤ 1 (no acute inflammatory infiltrate) (p = 0.193). Patients with NI ≥ 3 (moderately to severely active disease) had a significantly higher rate of disease progression than patients with NI ≤ 2 (p = 0.009).

Kaplan–Meier curve of time to disease progression stratified by histologic activity in patients with UC having mild endoscopic activity. The risk of disease progression, defined as starting or switching to a corticosteroid, biologic, or small-molecule agent or undergoing a surgical procedure and hospitalization for UC exacerbation during the post-endoscopy (with biopsy) follow-up, was analyzed according to histologic activity (NI) in patients with mucosal healing. (A) NI < 2 versus 2, (B) NI < 3 versus ≥ 3. NI, Nancy index; UC, ulcerative colitis.
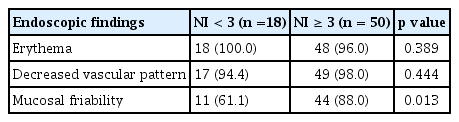
Based on these results, we searched for endoscopic findings that might help predict an NI of ≥ 3 in patients with an MES of 1. Among the endoscopic features listed in the Mayo endoscopic scoring system, mucosal friability was observed at a significantly higher rate in patients with NI ≥ 3 compared to those with NI < 3 (61.1% vs. 88.0%, p = 0.013) (Table 3).
Individual histologic findings predicting disease progression in patients with mild endoscopic activity
Individual histologic items were analyzed to evaluate their relevance to disease progression. On univariate analysis, the presence of serrated architectural abnormalities (0.98 ± 0.91 vs. 1.80 ± 0.89, p = 0.002) and ulceration (0.33 ± 0.47 vs. 0.80 ± 0.41, p = 0.001) were significantly correlated with disease progression. Multivariate analysis indicated that although not statistically significant, NI tended to be associated with disease progression (odds ratio 2.071, 95% confidence interval 0.964–4.447, p = 0.062) (Supplementary Table 2, 3).
DISCUSSION
This prospective study assessed the role of histology as a risk factor for disease progression and analyzed the endoscopic features predictive of active histologic inflammation in patients with UC having complete (MES of 0) or partial (MES of 1) mucosal healing. In patients with an MES of 1, indicating mild endoscopic activity, NI ≥ 3 was found to be correlated with a high likelihood of disease progression. A similar result was found at NI = 2, although the difference was not statistically significant. Patients with mucosal friability observed endoscopically had significantly higher rates of NI ≥ 3. NI also revealed the possibility of independent histological risk factors associated with disease progression.
Current guidelines on UC recommend clinical response or remission, endoscopic mucosal healing, and normalization of biomarkers, such as CRP and fecal calprotectin, as treatment targets [4,5]. Histological remission is not yet recommended as a treatment target for UC; however, current guidelines suggest that it could be used as an adjunct to other treatment targets [5,13,14]. Accumulating evidence has indicated that persistent histological activity can be observed in patients with endoscopic mucosal healing [13,14,24]. It has been estimated that 14–40% of patients with mucosal healing have histological activity [10,16]. Truelove and Richards observed that 37% of patients with no remarkable endoscopic findings had histological inflammation [25]. In our study, 69.4% of the patients with an MES of 0 had at least mild active disease or worse histologically. Although the inconsistent definitions of histologic activity among individual studies caused differences in proportions, our findings are consistent with those of previous studies.
Several studies have been conducted on histological activity and its prognostic value in clinical outcomes. In a systematic review and meta-analysis, Pai et al. [13] observed that histology accurately predicts clinical relapse, hospitalization, steroid use, and cancer development and that histological disease activity is more predictive than other measures of important clinical outcomes in UC. In a cohort study with long-term follow-up, Bryant et al. [14] suggested that histologic remission predicts clinical outcomes better than other treatment targets and encouraged the inclusion of histologic indices in future clinical trials and practice. While several indices have been developed to assess histological disease activity, none have been fully validated [13,14,26]. Due to the increasing need for a validated, consistent scoring system, Marchal-Bressenot et al. [21] developed the NI in 2017. The NI is composed of three histologic items yielding a five-grade classification for histologic disease activity in UC [21], and the European Crohn’s and Colitis Organisation (ECCO) has recommended its use in clinical practice [27]. Our study incorporated NI because of its excellent intra-and interobserver reliability, simplicity, and practicality [26,27]. Our data indicated that in patients with mild endoscopic activity (MES of 1), NI ≥ 3 was a predictor of poor clinical outcomes. NI = 2 was not free from poor outcomes, although statistical significance was not achieved. These findings not only confirm the predictive value of the scoring system but also provide a cutoff value to assess active histologic disease in patients with UC. Incomplete validation of index systems and the need to change the type or dose of agents based on histological activity in patients with mucosal healing are clinical issues that may arise when using histological remission as a therapeutic goal and require further attention. However, accumulating evidence suggests a strong relationship between histological activity and disease prognosis in patients with UC.
None of the patients with MESs of 0 experienced disease progression during the follow-up period. These results imply that patients with UC having an MES of 0 have favorable clinical outcomes regardless of histologic activity. This is consistent with previous studies reporting that more stringent criteria, that is, targeting an MES of 0 for treatment, are associated with better clinical outcomes and lower relapse rates [9,28]. We still need to emphasize this point. A previous meta-analysis showed that the estimated annual risk of clinical relapse in patients who achieved clinical remission with an MES of 0 was 13.7% [29]. Considering the clinical course of patients with an MES of 1, future disease relapses might occur in patients with an MES of 0 if the NI is ≥ 3. Therefore, conducting further long-term follow-up research with a greater focus on patients with an MES of 0 would be helpful.
A correlation between the histological index and endoscopic findings was observed in our study. Interestingly, our data indicated that mucosal friability was predictive of active histological inflammation in patients with UC having an MES of 1. However, this finding may be somewhat limited owing to the lack of detailed and objective definitions of “mucosal friability,” and endoscopic findings may be subject to significant inter-observer variability. Validation through large-scale studies is required to offer important implications for the development of endoscopic systems that can predict histological activity. Assessing histological activity through NI using biopsy would help better predict patient prognosis and endoscopic findings are still considered an alternative.
Individual histological features associated with disease prognosis have been widely studied [12,17,30]. Although none of these features are reliable on their own, some of these features are noteworthy. Riley et al. [31] found that acute inflammatory cell infiltration, crypt abscesses, and mucin depletion were statistically significant predictors of clinical relapse. The presence of basal plasmacytosis has been suggested to have a substantial predictive value for clinical relapse, with excellent reproducibility, although some recent studies have failed to demonstrate its value as a prognostic factor [32–34]. A serrated architectural abnormality is a histological finding described relatively recently in patients with UC, and some studies have indicated that its presence is associated with an increased risk of high-grade dysplasia and colorectal neoplasia [35,36]. In our study, although multivariate analysis revealed that a serrated architectural abnormality could not be an independent individual histologic risk factor for disease progression, a serrated architectural abnormality may be associated with a disease related to chronic mucosal inflammation. Further studies are required to establish the role of serrated architectural abnormalities in patients with UC.
A key limitation of our study was that patients with proctitis were included, which may have led to a lower disease progression rate. Another limitation was that not all patients were evaluated using colonoscopy; approximately 40% were evaluated using sigmoidoscopy. Further limitations include being a single-center study, which is partially compensated for by the minimal interobserver variation in pathology. The lack of long-term follow-up data and relatively small sample size are also limitations of this study. Because the number of patients with an MES of 0 in our study was not sufficiently large and the follow-up period was not long enough, the usefulness of NI in these patients needs to be investigated in larger-scale and long-term follow-up studies.
In conclusion, our study suggests that patients with UC having more severe histologic activity (NI ≥ 2) observed on histology may require closer monitoring, even if they have mild endoscopic activity (MES of 1). Mucosal friability on endoscopy may be a clue to suspect a more severe histological status. These findings may help identify patients with UC who require closer monitoring.
KEY MESSAGE
1. Patients with UC having more severe histologic activity showed a poor prognosis, even if they had mild endoscopic activity.
2. Mucosal friability on endoscopy was associated with a more severe histologic status.
3. Histologic and endoscopic assessment can help predict prognosis of patients with UC patients having mild endoscopic activity.
Notes
CRedit authorship contributions
Seung Yong Shin: resources, investigation, data curation, formal analysis, validation, writing - original draft; Hee Sung Kim: conceptualization, methodology, writing - review & editing, supervision; Kisung Kim: investigation, data curation, formal analysis, writing - original draft; Chang Won Choi: investigation, data curation, formal analysis; Jung Min Moon: resources, investigation, data curation; Jeong Wook Kim: resources, investigation, data curation; Hyun Jin Joo: resources, investigation, data curation; Jeongkuk Seo: resources, investigation; Muhyeon Sung: resources, investigation; Chang Hwan Choi: conceptualization, methodology, supervision, funding acquisition
Conflicts of interest
The authors disclose no conflicts.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIP [NRF-2020R1F1A1075489]). This research was also supported by the Chung-Ang University Research Grants in 2021.