Minimizing radiation exposure in endoscopic retrograde cholangiopancreatography: a review for medical personnel
Article information
Abstract
Fluoroscopy is used frequently during endoscopic procedures, such as endoscopic retrograde cholangiopancreatography (ERCP). However, exposure to radiation is an important health concern, primarily because of the potential increase in the lifetime risk of malignancy. This consideration is important for patients and staff exposed to radiation during ERCP. Thus, an understanding of how radiation doses are measured during ERCP and the potential risks of this radiation is important. Additionally, staff must be educated about methods used to minimize the radiation dose, such as the use of different imaging techniques, the general principles of fluoroscopy, and advances in hardware and software. The use of personal protective equipment is also essential to minimize occupational exposure. However, no comprehensive ERCP guideline on the use of X-ray systems in clinical settings or on radiation protection for operators has been established. This review focuses on the properties of fluoroscopy systems and methods of radiation protection for physicians and assistants participating in ERCP.
INTRODUCTION
Fluoroscopy is used widely for diagnosis and treatment in the clinic. Excessive and prolonged exposure to radiation has multiple detrimental effects. Most endoscopic retrograde cholangiopancreatography (ERCP) procedures involve fluoroscopy for the examination of bile- and pancreatic-duct structure and abnormalities. Fluoroscopy is associated with radiation exposure, which has long-term adverse effects, for physicians and assistants [1,2]. The risk of radiation exposure is recognized as important for radiologists, but also exists for gastroenterologists performing ERCP.
Physicians should be aware of the cumulative risks of radiation exposure. Furthermore, the use of methods that reduce the radiation dose are important to mitigate harmful effects on physicians and assistants, who may perform several hundred procedures annually. This review highlights radiation exposure and safety considerations for medical staff performing ERCP.
BIOLOGICAL EFFECTS OF RADIATION
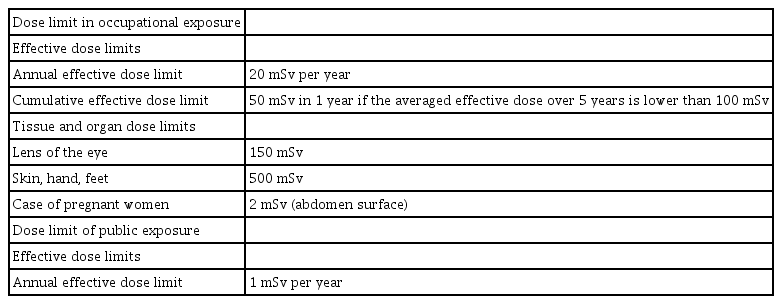
Radiation exposure has a deterministic effect that causes radiation-induced cell death, such as by tissue necrosis, and a stochastic effect that causes cancer or genetic mutations not associated with cell death. Tissue necrosis occurs when the starting dose is exceeded, and its severity increases with the dose. The threshold dose is not an absolute value, but is determined on a person-by-person basis. Conversely, the stochastic effect can lead to cancer or genetic mutations, even at low doses. The dose limit for radiation-related workers is 50 mSv annually, based on the effective dose; the 5-year cumulative dose limit is 100 mSv (Table 1).
EXPRESSION OF THE RADIATION DOSE DURING ERCP
The amount of radiation used during ERCP should be measured using a dosimeter. The entrance surface dose, which is the amount of radiation injected into the skin, and the absorptive dose in tissue should be measured. However, the direct measurement of these doses is nearly impossible. Thus, the fluoroscopy time (FT), air kerma (AK), and dose-area product (DAP; AK-area production, Gy·cm2) are used to express radiation doses used during ERCP. The kerma (derived from “kinetic energy released in material”) is the amount of energy carried by radiation; it is the initial kinetic energy of charged particles per unit mass generated by ionizing radiation [3,4].
Fluoroscopy time
The FT (minute) refers to the amount of time during which X-rays are used during the ERCP procedure. It contributes to radiation exposure during fluoroscopy, is measured easily, and indirectly reflects exposure. However, the FT is less accurate as a measure of independent patient exposure and does not include doses used for image acquisition. Nevertheless, the FT is typically proportional to the radiation dose; thus, its measurement and reduction may be the easiest and most effective means of reducing radiation exposure during ERCP.
Air kerma
The AK at the reference point (Gy) is the overall cumulative AK value and is used for dose monitoring in interventional procedures involving ionizing radiation. The interventional reference point is the point at which the patient’s incident surface is predicted to be located during X-ray exposure, assuming that the patient is lying on a table. Typically, this point is a point in space along the central X-ray beam, 15 cm back from the isocenter toward the X-ray generator and may be referred to as the virtual incident surface dose. However, this measure is not accurate because the scattering radiation generated by the patient’s incident surface or surrounding objects is not considered.
Dose-area product
The DAP (AK-area production, Gy·cm2) is the cumulative value of the product of the AK and the irradiated area when radiation is introduced into the air. It is used to monitor patient doses and predict the risk of probabilistic effects of radiation in recent radiation-generating devices. The DAP is also used in research to represent the total radiation dose transmitted to patients. Indeed, it provides a good estimation of the total radiation transmitted to physicians and patients, and is correlated with the FT [5].
Effective dose
Human tissues have different sensitivities to radiation. At the same equivalent dose, the risk and symptoms (e.g., degree and risk of burns on the chest and palms) differ according to the tissue/organ exposed. Thus, the effective dose (Sv), which reflects the difference in risk according to the tissue/organ, was introduced to prevent probabilistic effects. This value is the average of radiation doses received by the different organs or tissues, weighted for the relative biological effectiveness of the type of ionizing radiation and for the respective organ/tissue sensitivities. The effective dose was introduced to express the detrimental effects of radiation exposure and is calculated by multiplying the equivalent dose (HT) in all tissues and organs by the tissue weight (WT), with consideration of the radiation sensitivity of the tissues and organs. The International Commission on Radiological Protection (ICRP) recommends the use of the effective dose as a unit to evaluate the radiation exposure of medical personnel.
FLUOROSCOPIC SYSTEMS AND RADIATION DOSE MANAGEMENT
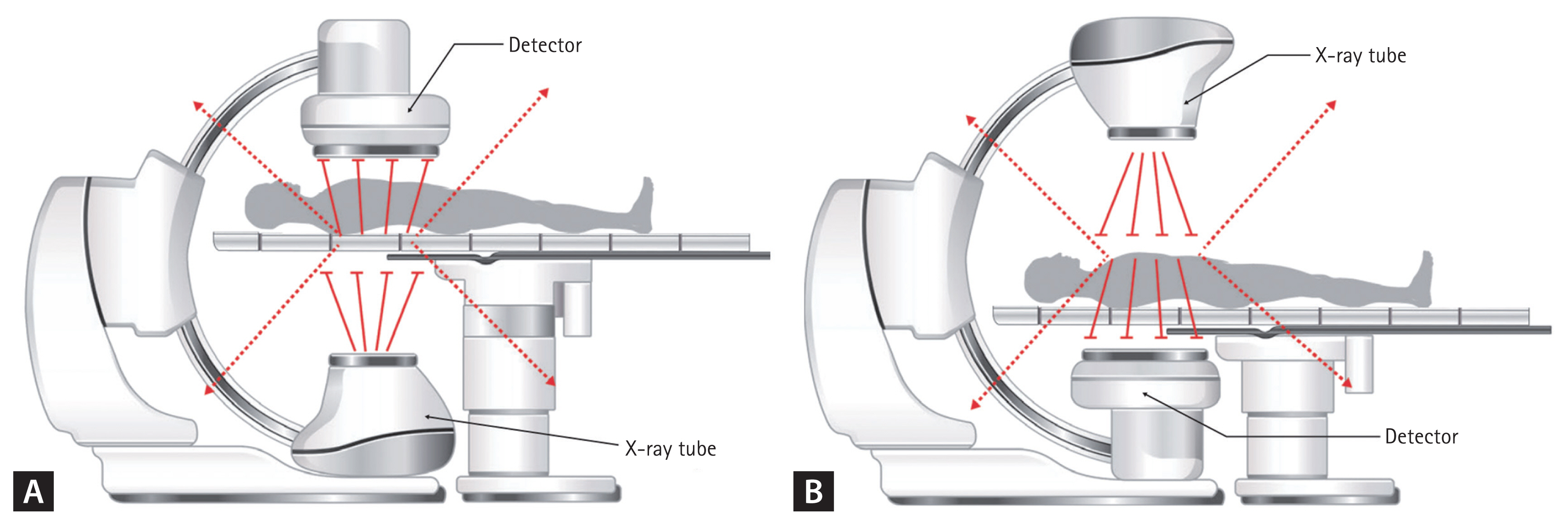
A commonly used stationary fluoroscopy system for ERCP has a combined and fixed patient table, with an under-table X-ray tube and an image receptor above the patient (under-couch system) (Fig. 1A). Another stationary system has the reverse design, with an over-table X-ray tube and an image receptor under the table (over-couch system) (Fig. 1B). In a mobile fluoroscopy system, the X-ray tube and image receptor are mounted on a C-arm positioner that allows angulation of the image chain around the patient. Radiation exposure starts from above the patient and transitions to below the patient in over-couch systems, whereas it starts under the patient and moves to above the patient in under-couch systems [6]. Bowsher and Blott [7] showed that the radiation dose delivered to the body parts of the physician above the table by an over-couch system is five- or six-fold greater than that delivered by an under-couch system, likely because of the increased radiation scatter above (instead of below) the patient in the latter case.
The location of the patient relative to the X-ray tube and image receptor affects the radiation dose and exposure of medical staff. The X-ray intensity is inversely proportional to the inverse square of the distance from the X-ray tube. Thus, the patient should be positioned as far as possible from the X-ray tube. The reduction of the source–image receptor distance by positioning the image receptor as close as possible to the patient’s exit surface will also reduce the patient dose. For example, when using an under-couch system, the image receptor should be attached as closely as possible to the patient’s body.
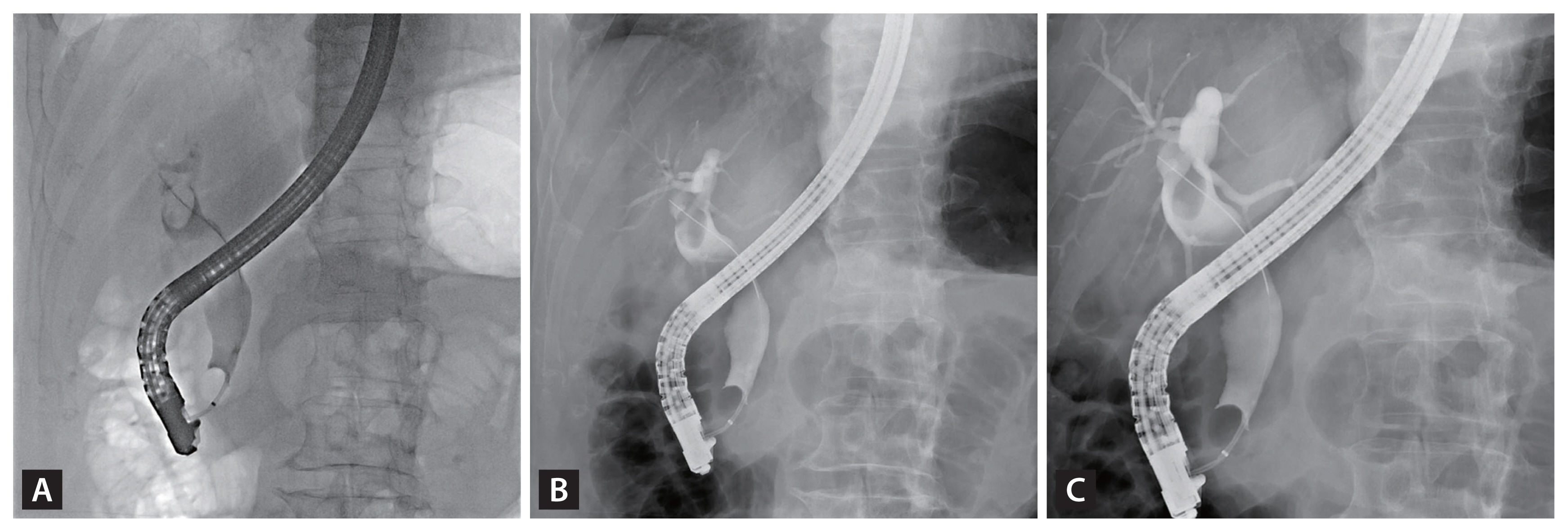
Compared with continuous fluorography, pulsed fluorography generates significantly smaller radiation doses (Fig. 2). Thus, the low-pulse-rate fluoroscopy mode should be used as much as possible, whereas the use of high-level control fluoroscopy should be limited. A retrospective analysis of 400 ERCP procedures showed that successful ERCP was possible with single-frame fluoroscopy, and that this approach resulted in less radiation exposure than reported previously [8]. In addition, the use of the last-image-hold method instead of image acquisition may be beneficial (Fig. 3A and 3B). Image magnification is useful for the visualization of lesions and guidewires during ERCP; however, it requires increased radiation doses (Fig. 3C). Thus, image enlargement only when necessary is recommended. In addition, the proactive use of a collimator is recommended because it reduces the amount of radiation generated and allows for increased scattering of waves by adjustment of the area of interest.
PROTECTION FROM OCCUPATIONAL RADIATION EXPOSURE
The three principles of radiation protection are distance, time, and shielding [9]. Scattered X-rays emitted from patients are the main source of radiation exposure for physicians and assistants during ERCP. Thus, efforts must be made to reduce exposure to these scattered X-rays. To minimize radiation exposure, the operator and assistant must determine the distribution of the scattered radiation levels in the procedure room. Johlin et al. [10] reported that the endoscopist and assistant were exposed to the highest dose near the patient’s head. Thus, to ensure safety, the physician and assistant should be located as far from the patient as possible, as scattering decreases rapidly with distance. The distribution of scattering waves differs depending on the type of stationary X-ray fluoroscopy system used. For example, with an over-couch system, scattering waves are concentrated on the upper body of the operator; thus, the shielding device should be placed above the table.
The use of the shortest possible FT is recommended; the limiting of the FT is the most direct dose-reduction technique. Moreover, the system must be turned off when not in use. The occupational dose can be reduced by limiting the FT or by displaying the FT and radiation doses to the operator in real time [11].
The most effective means of protecting medical staff from radiation exposure is the use of personal protective equipment and facilities. Various types of shielding device can be used to protect the operator and assistants in the ERCP room [12–15]. These devices include aprons, neck and thyroid protectors, and leaded goggles (Fig. 4). Aprons can significantly reduce radiation exposure, but no clear recommendation on their thickness has been established. Although the protective effect of aprons varies slightly among studies, protection from scattered radiation reflected at a right angle is expected to be similar for lead aprons of ≥ 0.25 mm thickness [14]. The protection of the eyes from radiation exposure is particularly important for physicians who routinely perform fluoroscopy procedures using over-table X-ray tube systems, to minimize the cataract risk. Protective shielding to reduce exposure of the eyes to scattered radiation includes leaded goggles and mobile or ceiling-suspended shields. Mobile shield barriers are useful for the reduction of radiation exposure and can be mounted on the floor or ceiling or on a table (Fig. 5). Various types of mobile shield have been developed, and several of them can be combined to reduce exposure from scattering waves [16–20].

Correct wearing of protective equipment (apron, neck and thyroid protector, leaded glasses/goggles) for radiation shielding.

Various types of protective shield. (A) Ceiling-type protector shield. (B) Mobile rolling shield on wheels. (C) Lower protector.
The use of protective lead shields with over-couch systems is beneficial [17,21,22]. A phantom study conducted by Morishima et al. [23] showed that radiation scattering was decreased by 89.1% with the use of an additional protective shield. In a prospective study conducted by Chung et al. [16], the use of a mobile shield barrier during ERCP led to a significant reduction in radiation exposure to medical personnel.
All staff participating in ERCP should be aware of the risk of radiation exposure and should have a comprehensive understanding of the fluoroscopy system and how to reduce radiation exposure.
COMPLEXITY OF ERCP
With prolonged or difficult procedures and cases in which various procedures are performed simultaneously, the duration of radiation use increases. The radiation exposure is also likely to increase, depending on the complexity and difficulty of the procedure. Indeed, complex therapeutic interventions are associated with increased FTs [24–26].
In a retrospective study of 197 patients undergoing 331 ERCP procedures, significant increases in all radiation parameters were observed with each increment in procedure complexity [27]. In addition, in a retrospective analysis of 269 ERCP procedures, the mean fluoroscopy duration was significantly longer for more complex therapeutic procedures (p = 0.002); overall, increased fluoroscopy duration was associated with procedure complexity [24]. A recent retrospective study showed that ERCP performed using mechanical lithotripsy or a needle knife or in patients with malignant biliary construction involved a significantly increased fluoroscopy duration [26].
Thus, the operator and assistant must be aware that radiation exposure may be prolonged with long, difficult, or complex procedures. In cases in which such procedures cannot be avoided, efforts should be made to reduce the generation of radiation by using a low-pulse-rate fluoroscope and collimator, minimizing image enlargement, and using the last-image-hold method.
EXPERIENCES OF LOW- AND HIGH-VOLUME ENDOSCOPISTS
Although endoscopist experience and procedural volume are associated with lower adverse event and failure rates in ERCP [28–30], the impact of endoscopist experience on patients’ radiation exposure during ERCP is unclear. The radiation dose to the patient has been found to decrease with increasing endoscopist experience [24,31–33]. In a retrospective study, ERCP performed by less-experienced endoscopists involved significantly more radiation exposure than did that performed by experienced operators, despite the fact that experienced endoscopists typically perform more complex ERCP procedures [27].
By contrast, radiation exposure did not differ between procedures performed by low-volume endoscopists (LVEs) and high-volume endoscopists (HVEs) [34]. This finding was attributed to the fact that HVEs typically perform more complex and difficult procedures than do LVEs.
PATIENT POSITION AND BODY MASS INDEX
ERCP can be performed with the patient in the prone or left lateral decubitus (LLD) position, depending on the endoscopist’s preference [35]. Because the vertical body thickness is lesser in the prone position than in the LLD position, beam adjustment of the X-ray tube is less likely to be required in the former case [36]. Moreover, a greater distance between the image intensifier and the X-ray tube or patient could increase radiation scattering. In a prospective study, the ocular lens equivalent doses of ERCP personnel were reduced by 37.5% and 59.0%, respectively, by changing the patient position from LLD to prone [37].
Higher body mass indices (BMI) increase the FT, but ERCP-specific data on this factor are sparse [38,39]. For instance, Smuck et al. [40] reported that the mean FT during a spinal procedure increased by 30% for overweight patients. The authors suggested that good-quality images of obese patients were difficult to obtain, and that the precise positioning of such patients required more time, thereby increasing the overall procedure duration. In a recent retrospective analysis of 797 ERCPs, the FT tended to be longer for patients with higher BMIs [26]. These findings were attributed to delays caused by patient sedation and movement, image degradation due to the body thickness, and increased radiation generation due to automatic exposure control in fluoroscopy.
IMPORTANCE OF EDUCATIONAL PROGRAMS
It is important that medical staff participating in ERCP are not only familiar with the principles of radiation exposure but also ensure that such exposure is minimized. However, formal curricula related to radiation exposure are uncommon in endoscopic training programs. Radiologists are ahead of us in terms of safety measures for radiation exposure and the generation of evidence on the comparative use of radiation across institutes, as well as national averages, to facilitate improvements in clinical practice. Radiologists have also emphasized the importance of educational programs to reduce radiation exposure. In a recent online survey, 56.6% of endoscopists at university hospitals who had performed ERCP for > 5 years reported that they had received no formal training on the minimization of radiation exposure [41].
In a prospective study, Barakat et al. [42] highlighted an important safety issue and associated it with endoscopists’ lack of formal education on radiation exposure. Their educational program, which emphasized the use of optimal fluoroscopy and X-ray parameters, significantly reduced ERCP-associated radiation exposure. The authors recommended that advanced endoscopy training programs include radiation exposure protocols.
CONCLUSIONS
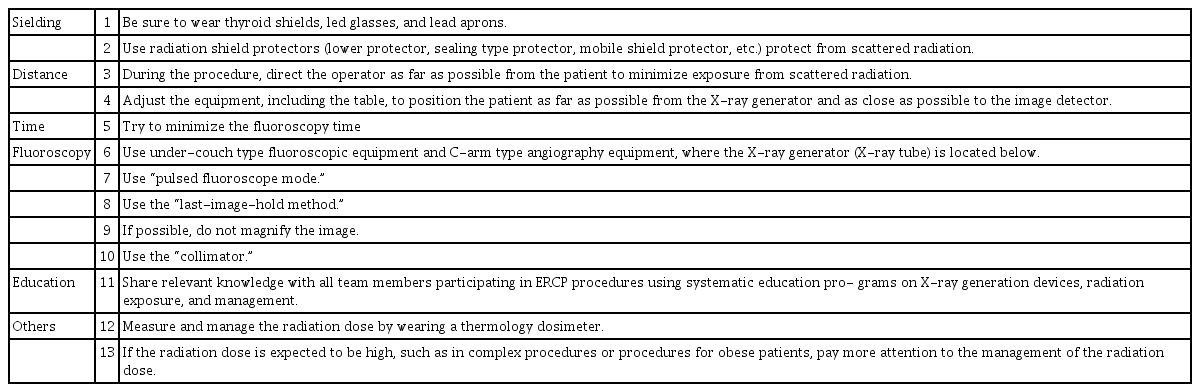
ERCP is an essential diagnostic and therapeutic procedure for patients with pancreatic and biliary-tract diseases. Endoscopists performing ERCP use fluoroscopic systems to obtain real-time images of the pancreatobiliary system. Fluoroscopy introduces the risk of radiation exposure for the patient, physician, assistant nurse, and other staff in the ERCP room. We reviewed current methods for radiation protection (Table 2). In complex cases, radiation exposure is expected to be high during the procedure. However, because the complexity of ERCP required for a given case can be difficult to predict, the operator should be aware of the possibility of high radiation exposure and the steps that can be taken to minimize this risk. The use of pulsed fluoroscopy, minimization of the FT, limiting of the number of radiographs and use of enlarged images, use of shielding walls, and wearing of complete protective clothing (protective apron, thyroid shield, and leaded glasses) can reduce occupational radiation exposure. Most importantly, not only endoscopists but also other staff participating in the procedure should be educated on the risks of radiation exposure and methods of radiation protection. The reporting and recording of patient radiation doses in a national database is needed to determine the mean radiation exposure for each procedure type and for the formulation of guidelines and recommendations for appropriate doses.
Notes
No potential conflict of interest relevant to this article was reported.