Hemoptysis due to pulmonary infarction in COVID-19
Article information
A previously healthy man in his 50s was admitted to our hospital with fever and hemoptysis in late 2020. He had developed fever 17 days before and was subsequently diagnosed with coronavirus disease 2019 (COVID-19). On admission, his oxygen saturation was 96% on room air and D-dimer level was 5,410 ng/mL. Unenhanced chest computed tomography (CT) showed peripheral consolidations with ground-glass opacities and pleural effusion (Fig. 1A and 1B). He was treated with methylprednisolone, favipiravir, and edoxaban.
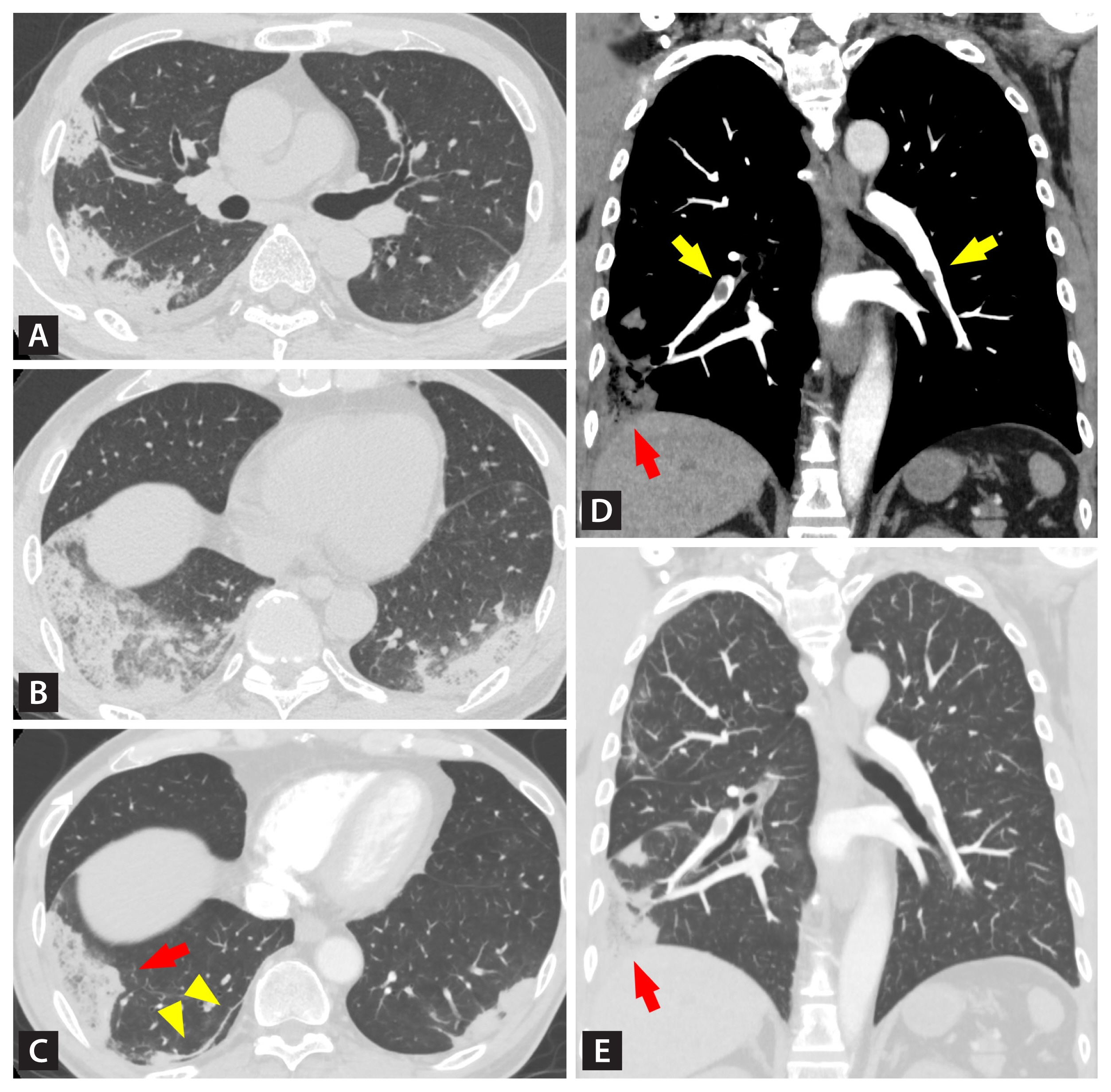
Chest computed tomography (CT) images on admission (A, B) and on day 5 (C, D, E). (A) Axial unenhanced CT obtained at the level of the right pulmonary artery showed peripheral consolidations and bilateral pleural effusion. (B) At the level of the lung base, consolidations admixed with ground-glass opacities were present. (C) Axial contrast-enhanced CT obtained at the same level as (B) showed a subpleural curvilinear line (yellow arrowheads) and a wedge-shaped consolidation with internal lucencies (red arrow). (D) A coronal image revealed pulmonary embolism (yellow arrows). One of the emboli was proximal to the remaining consolidation (red arrow). (E) The consolidation in (C) also exhibited the wedge-shaped appearance (red arrow).
Hemoptysis persisted and contrast-enhanced CT was performed on day 5. Most consolidations were resolving with a residual subpleural curvilinear line. A wedge-shaped consolidation with internal lucencies persisted suggesting pulmonary infarction (Fig. 1C). Coronal images revealed bilateral pulmonary emboli, one of which corresponded to the remaining consolidation (Fig. 1D and 1E). The pulmonary infiltrates disappeared after 3 months of edoxaban therapy.
Pulmonary embolism is common in patients with COVID-19, while hemoptysis and pulmonary infarction are infrequent. Physicians should perform contrast-enhanced CT for COVID-19 patients with hemoptysis and can continue anticoagulation for pulmonary infarction causing hemoptysis.
Written informed consent was obtained from the patient for publication.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
