No benefit of hypomethylating agents compared to supportive care for higher risk myelodysplastic syndrome
Article information
Abstract
Background/Aims
This study evaluated the role of hypomethylating agents (HMA) compared to best supportive care (BSC) for patients with high or very-high (H/VH) risk myelodysplastic syndrome (MDS) according to the Revised International Prognostic Scoring System.
Methods
A total of 279 H/VH risk MDS patients registered in the Korean MDS Working Party database were retrospectively analyzed.
Results
HMA therapy was administered to 205 patients (73.5%), including 31 patients (11.1%) who then received allogeneic hematopoietic cell transplantation (allo-HCT), while 74 patients (26.5%) received BSC or allo-HCT without HMA. The 3-year overall survival (OS) rates were 53.1% ± 10.7% for allo-HCT with HMA, 75% ± 21.7% for allo-HCT without HMA, 17.3% ± 3.6% for HMA, and 20.8% ± 6.9% for BSC groups (p < 0.001). In the multivariate analysis, only allo-HCT was related with favorable OS (hazard ratio [HR], 0.356; p = 0.002), while very poor cytogenetic risk (HR, 5.696; p = 0.042), age ≥ 65 years (HR, 1.578; p = 0.022), Eastern Cooperative Oncology Group performance status (ECOG PS) 2 to 4 (HR, 2.837; p < 0.001), and transformation to acute myeloid leukemia (AML) (HR, 1.901; p = 0.001) all had an adverse effect on OS.
Conclusions
For the H/VH risk group, very poor cytogenetic risk, age ≥ 65 years, ECOG PS 2 to 4, and AML transformation were poor prognostic factors. HMA showed no benefit in terms of OS when compared to BSC. Allo-HCT was the only factor predicting a favorable long-term outcome. The use of HMA therapy did not seem to have an adverse effect on the transplantation outcomes. However, the conclusion of this study should be carefully interpreted and proven by large scale research in the future.
INTRODUCTION
Based on current guidelines, there is no specific recommended bridge or frontline therapy including hypomethylating agent (HMA), cytotoxic therapy or supportive care for the subgroup of patients with high or very high (H/VH) risk myelodysplastic syndrome (MDS) eligible for allogeneic hematopoietic cell transplantation (allo-HCT) [1]. However, when considering the practical aspects of allo-HCT, there may be no appropriate donor or it may take more than 5 months from identifying an appropriate stem cell source to performing allo-HCT [2].
The use of HMA such as azacitidine and decitabine has been quite successful for MDS in terms of improving the hematologic response or survival duration [3,4]. Thus, for higher risk MDS, the use of HMA therapy while waiting for allo-HCT can be an attractive option, offering the potential for successful cytoreduction before allo-HCT and improved HCT outcome [5,6].
Accordingly, the current study retrospectively compared HMA therapy and supportive care in terms of the allo-HCT outcomes for high and very high risk MDS based on the Revised International Prognostic Scoring System (IPSS-R).
METHODS
A total of 572 patients diagnosed with MDS and registered in the Korean MDS Working Party database from October 1992 to July 2013 were classified into five subgroups according to IPSS-R: very low, low, intermediate, high (H), and very high (VH) risk [7]. The clinical characteristics and treatment outcomes were retrospectively reviewed for the 279 patients with H or VH risk MDS. A standard regimen of azacitidine (75 mg/m2/day for 7 days every 4 weeks) or decitabine (20 mg/m2/day for 5 days every 4 weeks) was used. The response to HMA was estimated after three to six cycles of HMA treatment [8]. The responses were coded according to the 2006 International Working Group guidelines [9].
Definition
The IPSS-R prognostic risk categories were determined by combining the scores of main five features: cytogenetics, bone marrow (BM) blast, hemoglobin (Hb), platelets, and absolute neutrophil count (ANC). High risk category was defined score from 4.5 to 6 and very high risk category was defined score 6 or more. The responses were categorized as complete remission (CR), partial remission (PR), marrow CR (mCR) with or without hematologic improvement (HI), and HI. Stable disease was defined as the failure to achieve at least PR yet without evidence of progression for 8 weeks. Progressive disease was defined as the progression to a higher risk MDS category, transformation to acute myeloid leukemia (AML), or loss of response. The best response was defined as the best response achieved by a patient at any time point. Engraftment was defined as the first of three consecutive days when the ANC exceeded 0.5 × 109/L. Graft failure was defined as the lack of myeloid engraftment in patients surviving in remission for at least 28 days after transplantation. The criteria used for the diagnosis and grading of acute and chronic graft-versus-host disease (GVHD) were as previously described [10].
Statistical analysis
The categorical data were analyzed using chi-square tests. The overall survival (OS) rate was analyzed using the Kaplan-Meier method, and the treatment groups were compared using log-rank tests. The OS was calculated from the date of diagnosis to the date of death from any cause or last follow-up. Leukemia-free survival (LFS) was defined as from the date of diagnosis to time of leukemic transformation or last contact/death for LFS. Multivariate stepwise analysis was used to determine independent prognostic importance of several clinical factors, especially, IPSS-R, treatment group. The significances of the covariates affecting OS and LFS were determined using a Cox proportional hazard model. The statistical analyses were performed using IBM SPSS Statistics for Windows version 20.0 (IBM Corp., Armonk, NY, USA).
RESULTS
The patient characteristics are summarized in Table 1. The median age was 65 years (range, 15 to 86) and 136 patients (48.7%) were under 65 years. The Eastern Cooperative Oncology Group performance status (ECOG PS) was 0 to 1 in 215 patients (77.1%) and 2 to 4 in 64 patients (22.9%). The IPSS-R H and VH risk groups included 160 patients (57.3%) and 119 patients (42.7%), respectively. The cytogenetic risk groups based on IPSS-R were as follows: very good (five patients, 1.8%), good (116 patients, 41.6%), intermediate (58 patients, 20.8%), poor (42 patients, 15.1%), and very poor (58 patients, 20.8%). The percentage of BM blasts was below 2 in 20 patients (7.2%), 2 to 5 in 36 patients (12.9%), 5 to 10 in 102 patients (36.6%), and more than 10 in 121 patients (43.4%). The ANC was < 0.8 × 109/L in 158 patients (58.6%), the Hb level was < 8 g/dL in 150 patients (53.8%), and the platelet count was < 50 × 109/L in 120 patients (43.4%). A total of 205 patients (73.5%) were treated with a median of four cycles of HMA (range, 1 to 63 cycles), including 31 patients (11.1%) who received allo-HCT following HMA therapy. Seventy-four patients (best supportive care [BSC], 69; allo-HCT, 5) were not previously treated with HMA therapy. The patients characteristics was similar except ECOG PS 0 to 1 (No HMA: n = 40, 54.1% vs. HMA: n = 175, 85.4%; p < 0.001).
A response to HMA was observed in 97 of the 205 patients (47.3%) who received HMA therapy, where 27 patients (13.2%) achieved CR, 19 (9.3%) PR, 17 (8.3%) mCR, and 34 (16.6%) HI. Eleven (one patient in CR, four in PR, four in mCR, and one in HI) of the 31 transplanted patients who received HMA therapy showed a response to HMA at the time of allo-HCT (Table 2). The median time to the transplantation of the patients transplanted without HMA was 140 days (range, 90 to 253). There was no significant difference in the time to HCT according to HMA therapy by independent t test (p = 0.123). Matched sibling donor (n = 8, 32%) and matched unrelated donor (n = 14, 56%) were included in a group of patients treated with HMA followed by HCT.
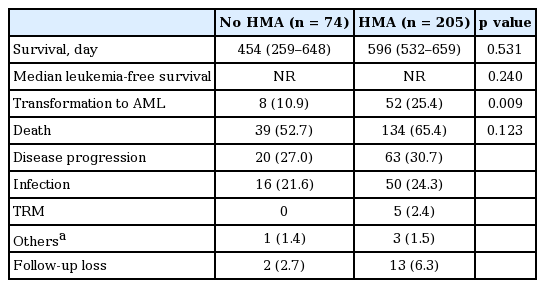
AML transformation was observed in 46 of the 174 patients (26.5%) who received HMA therapy and no allo-HCT, and in six of the 31 patients (19.4%) who received HMA therapy followed by allo-HCT. In the BSC only group, eight patients (11.5%) transformed to AML (Table 3). There was no case of AML transformation in the group who received allo-HCT without HMA therapy. The median survival duration was 1,113 days (range, 755 to 1,471) for allo-HCT with HMA, 537 days (range, 455 to 619) for HMA only, and 361 days (range, 169 to 553) for the BSC only group. The median survival duration was not reached by the allo-HCT without HMA group. Even if there was no statistical significance according to HMA therapy, median survival was longer in the HMA group than no HMA group (454 days vs. 596 days, p =0.531). So, the incidence of AML transformation may have been observed higher because of the prolonged survival duration.
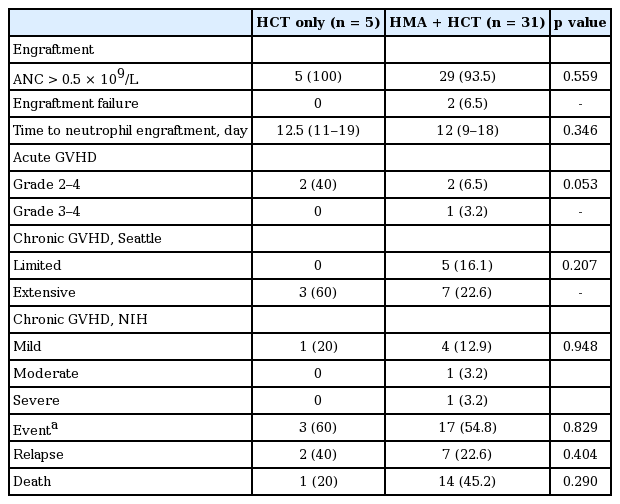
The 3-year OS rate for the HCT group overall was 61.6% ± 9.7%, which was significantly higher than that for the BSC and HMA groups (17.8% ± 3.1%, p < 0.001). The 3-year OS rate was 53.1% ± 10.7% for allo-HCT with HMA, 75% ± 21.7% for allo-HCT without HMA, 17.3% ± 3.6% for the HMA group, and 20.8% ± 6.9% for BSC group (p < 0.001) (Fig. 1). There was no significant differences by pairwise comparison in the 3-year OS rate between allo-HCT group according to HMA therapy (p = 0.256). There was no statistical difference in OS between the BSC and HMA groups (p = 0.531). The transplant outcomes are shown in Table 4 and Fig. 2. The incidence of acute or GVHD was not statistically different between the HMA-HCT and no HMA-HCT groups (p = 0.093).

Overall survival curves according to treatment plan. Allo-HCT, allogeneic hematopoietic cell transplantation; OS, overall survival; HMA, hypomethylating agents; BSC, best supportive care.

Incidence of acute (A) and chronic (B) graft-versus-host disease (GVHD). HMA, hypomethylating agents; aGVHD, acute GVHD; cGVHD, chronic GVHD.
In the multivariate analysis, for the H/VH risk patients, only allo-HCT was related to a favorable OS (hazard ratio [HR], 0.356; 95% confidence interval [CI], 0.186 to 0.681, p = 0.002), while very poor cytogenetic risk according to IPSS-R (HR, 5.696; 95% CI, 1.068 to 30.374; p = 0.042), age ≥ 65 years (HR, 1.578; 95% CI, 1.067 to 2.334), ECOG PS 2 to 4 (HR, 2.837; 95% CI, 1.852 to 4.346; p < 0.001), and transformation to AML (HR, 1.901; 95% CI, 1.310 to 2.757; p = 0.001) all had an adverse effect on OS (Table 5).
DISCUSSION
There is currently no consensus on a specific therapy for newly diagnosed higher risk MDS patients awaiting allo-HCT or those not eligible for allo-HCT. While early allo-HCT is a standard approach for HCT-eligible patients with higher risk MDS [1], in practice, some patients may require cytoreductive therapy before allo-HCT due to concerns of AML progression or a delayed search for an optimal donor. HMA can be an attractive option as a bridge therapy for higher risk MDS patients with a low toxicity profile, as it has a response rate of around 50% [11-13]. It is also not yet known whether posttransplant outcomes can be modified with pretransplant therapy with intensive chemotherapy or HMA. Randomized data are lacking. Some study showed the benefit of HMA, especially in elderly patients or patients with higher disease burden [14]. However, this study included 116 patients (49.2%) under the age of 65 years, and applied IPSS-R. IPSS-R put more weight on cytogenetics than BM blast cut-off.
In the current study, a very poor cytogenetic risk at presentation was identified as a significant indicator predicting poor survival, while a higher percentage of BM blasts was not. However, allo-HCT with or without HMA was the only therapeutic approach for overcoming a worse prognosis. When choosing a frontline therapy for high-risk MDS, HMA should be preferentially recommended for the purpose of cytoreduction in specific cases of unfavorable cytogenetics or the presence of blasts at a certain level in the presenting BM. According to Sekeres and Cutler [15], a frontline therapy with HMA may be required to minimize the relapse risk after allo-HCT in MDS patients with blast counts > 5% to 10% and/or an unfavorable cytogenetic profile at presentation. Lubbert et al. [16] recently demonstrated in a randomized phase III trial that HMA therapy with decitabine improved progression-free survival in high-risk MDS patients with complex karyotypes harboring two or more autosomal monosomies when compared to BSC. In addition, Brierley and Steensma [17] suggested that MDS with more than 10% blasts should be considered for cytoreductive therapy using either chemotherapy or HMA, especially before reduced-intensity HCT, while patients with less than 10% blasts should proceed directly to allo-HCT. Notwithstanding, up-front allo-HCT is particularly recommended for patients with life-threatening cytopenias, as any attempt to reduce the disease burden before allo-HCT exposes a patient to the risk of complications, such as severe infection, which may then prevent them from undergoing allo-HCT [18].
In the current study, HMA therapy did not show a favorable impact on OS when compared to BSC in the H/VH risk group. Yet, based on Kaplan-Meier survival curves, HMA therapy did show a survival advantage during the first 2 years of treatment when compared to BSC. Thus, while HMA therapy as a bridge to allo-HCT has a questionable benefit for high-risk MDS, it seems to be practically acceptable as an immediate therapy immediately after diagnosis; thus, and allo-HCT then needs to be performed as soon as possible for certain H/VH risk patients. HMA could bring a significant benefit as a bridge to allo-HCT in patients with the TET2 mutation or a less aggressive disease, whereas aggressive chemotherapy is preferred for medically fit patients with an aggressive disease [19,20]. Wermke et al. [21] suggested that up-front allo-HCT could be considered for patients with slowly progressing MDS if a donor is readily available.
In a previous survey of Korean clinicians, 88% chose HMA as a pre-HCT frontline therapy for high-risk MDS, while only 6% chose supportive care or no specific treatment before HCT [22]. In terms of the benefit of HMA as a bridging therapy for high-risk MDS patients eligible for allo-HCT, 58% of the Korean clinicians believed that HMA therapy can stabilize the disease status more safely, in terms of the side-effect profile, than intensive chemotherapy, while 27% considered that HMA therapy could ultimately improve the HCT outcome. Yet, there is still a practical dilemma when selecting a pre-HCT strategy for high-risk MDS.
Notwithstanding, it still remains whether the pretransplant use of HMA can negatively impact the outcome of a subsequent HCT as a result of damaging the patient’s performance or delaying HCT. According to a previous study comparing BSC, chemotherapy, and HMA as pretransplant therapies, HMA showed no negative impact on HCT outcome compared to BSC or chemotherapy [23].
In the present study, the incidence of acute or GVHD was not statistically different between the HMA-HCT and no HMA-HCT group (Fig. 2). However, it is still unclear whether pretransplant HMA can affect immunological function in the recipient. A previous study suggested that pretransplant HMA could augment the graft-versus-leukemia effect without harm in terms of GVHD by increasing the number of T regulatory cells and inducing a cytotoxic CD8+ T-cell response [24]. Although no definitive conclusions can be drawn from the present study due to the small number of patients included in the retrospective analysis, the pretransplant use of HMA did not seem to have a negative impact on the HCT outcomes in the H/VH risk MDS group when compared with historical HCT outcomes.
In conclusion, HMA showed no benefit in terms of OS in the H/VH risk group when compared with BSC. Allo-HCT was the only factor predicting a favorable long-term outcome for the patients with H/VH risk MDS. The use of HMA for higher risk MDS did not seem to have an adverse effect on the HCT outcomes when compared with historical HCT data for H/VH risk MDS. However, the conclusion of this study should be carefully interpreted and proven by large scale research in the future.
KEY MESSAGE
1. In patients with high/very high risk myelodysplastic syndrome (MDS) by Revised International Prognostic Scoring System (IPSS-R), hypomethylating agents showed no survival benefit compared to best supportive care.
2. Allogeneic hematopoietic cell transplantation was the only favorable factor for high/very high risk MDS by IPSS-R.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This research was supported by Kyungpook National University Research Fund, 2015 to 2016.