Immunologic and non-immunologic complications of a third kidney transplantation
Article information
Abstract
Background/Aims:
Patients who undergo repeat kidney transplantations (KTs) are considered at high risk for experiencing immunologic and non-immunologic complications. In this study, we investigated the clinical outcomes, including medical and surgical complications, of patients who underwent a third KT at our center.
Methods:
Between March 1969 and December 2012, a total of 2,110 KTs were performed at the Seoul St. Mary’s Hospital. Of them, we examined 11 patients who underwent a third KT, and investigated the allograft outcomes and complication rates.
Results:
The mean follow-up duration after KT was 72.4 ± 78.3 months. The mean age at KT was 38.2 ± 8.0 years, and seven patients (63.6%) were males. Nine patients (81.8%) underwent living-donor KT. A cross-match test yielded positive results in four of the nine patients, and all underwent pretransplant desensitization therapy. After KT, three patients (27.2%) showed delayed graft function. Acute rejection developed in four patients (36.4%), and surgical complications that required surgical correction occurred in three patients. Allograft failure developed due to acute rejection (n = 3) or chronic rejection (n = 1) in four patients. Allograft survival rates at 1, 5, and 10 years were 81.8%, 42.9%, and 42.9%, respectively; however, the allograft survival rate at 5 years was > 80% in patients who underwent KT only after results of the panel reactive antibody test became available.
Conclusions:
Thus, a third KT procedure may be acceptable, although aggressive pretransplant immune monitoring and patient selection may be required to reduce the risks of acute rejection and surgical complications.
INTRODUCTION
Kidney transplantation (KT) is considered the best treatment option for patients with end-stage renal disease [1,2]. Due to the increase in the number of patients with end-stage renal disease in Korea, the number of KTs has also markedly increased [3,4]. Moreover, long-term allograft survival rates have improved because of advancements in immune-suppressant and transplant techniques. However, a single transplant seems to be insufficient based on the limited duration of allograft survival in many patients; therefore, these patients require a further transplantation or must return to dialysis [5-8].
Many studies have investigated the clinical course of re-transplantation and have suggested that a second KT procedure shows superior patient outcomes and cost-effectiveness compared to patients who return to dialysis after allograft failure [5,6,9-11]. In addition, patients who undergo a second KT procedure have graft survival rates similar to those who undergo a first KT procedure [12-14]. Patients who undergo a third KT procedure will likely exhibit distinct characteristics compared to patients who undergo a second KT procedure because of a longer medical and surgical history, which may result in immunologic and non-immunologic complications [15,16]. However, few reports have presented the outcomes of a third KT procedure; hence, it is unclear whether a third KT is associated with better survival or whether this procedure is advisable for patients who experience a second allograft failure.
Therefore, in the present study, we investigated whether a third KT procedure is advisable for patients who experience a second kidney allograft failure by reviewing the clinical outcomes and complications associated with a third KT procedure.
METHODS
Between March 1969 and December 2012, a total of 2,110 KT procedures were performed at Seoul St. Mary’s Hospital. Of these, 1,950 were a first procedure, 149 were a second procedure, and the remaining 11 were a third procedure. We reviewed the clinical outcomes of patients undergoing their third KT procedure. Baseline characteristics such as sex, age, primary renal disease, and the results of immunologic tests (panel reactive antibody [PRA] tests, human leukocyte antigen [HLA] mismatch number, and cross-match tests) were collected. We also collected data on the main immune-suppressant type, dialysis status after previous allograft failure, and survival duration of the previous renal allograft.
In addition, we analyzed the clinical outcomes after the third KT procedure, including postoperative recovery pattern, development of acute rejection, surgical or infectious complications, and allograft survival rates. We also compared the allograft survival rate of these patients to those of patients who had undergone their first and second KT procedures. The Institutional Review Board of Seoul St. Mary’s Hospital (KC13RISI0808) approved this study.
Statistical analysis
Statistical analyses were performed using the SPSS version 20.0 (IBM Co., Armonk, NY, USA). Data are presented as means ± standard deviations or counts and percentages, according to the data type. Patient and allograft survival rates were calculated using the Kaplan-Meier method. All tests were two-tailed, and results with a p < 0.05 were considered significant.
RESULTS
Baseline characteristics
The baseline characteristics of the patient populations are presented in Table 1. The mean age at the time of the third KT procedure was 38.2 ± 8.0 years, and seven of the patients (63.6%) were males. The mean follow-up duration after the third KT procedure was 72.4 ± 78.3 months. Nine patients (81.8%) underwent living-donor kidney transplantation (LDKT) and two patients (18.2%) underwent deceased donor kidney transplantation (DDKT). Three of the LDKT donors were not related to the recipients. The main immunosuppressive drug was tacrolimus in seven patients (63.6%), cyclosporine in two, and azathioprine (Imuran, GSK, Philadelphia, PA, USA) in two. The mean HLA mismatch number was 3.3 ± 1.4. The PRA test was performed in six patients before KT; the value was > 50% in four patients (66.7%). The crossmatch test was positive in four of nine patients (44.4%) who underwent LDKT. Two of these four patients (patients 7 and 10) underwent desensitization therapy with rituximab, plasmapheresis, and intravenous immunoglobulin (IVIG) whereas the other two (patients 6 and 9) received plasmapheresis and IVIG alone (Table 1).
Clinical characteristics of the previous transplantation
The clinical characteristics of the previous allografts were available for 10 patients (Table 1). The mean survival duration of the first graft was 37.0 ± 38.2 months, whereas that of the second allograft was 59.5 ± 60.2 months. The mean interval between the first and second KT procedures was 63.3 ± 53.3 months, whereas that between the second and third KT procedures was 81.3 ± 58.1 months. After the second allograft failure, nine patients underwent hemodialysis; the remaining two patients underwent a preemptive third KT procedure. The donor types for the first and second procedures are shown in Fig. 1; grafts from living donors were used during the first and second transplantation procedures for most patients, similar to patients who underwent a third KT procedure. The causes of the first graft failure were acute rejection (7/11, 63.6%) and chronic rejection (4/11, 36.4%), whereas the causes of the second graft failure were acute rejection (6/11, 54.5%), chronic rejection (4/11, 36.4%;), and renal infarction with renal artery thrombosis (1/11, 9.1%).
Clinical outcomes after the third KT procedure
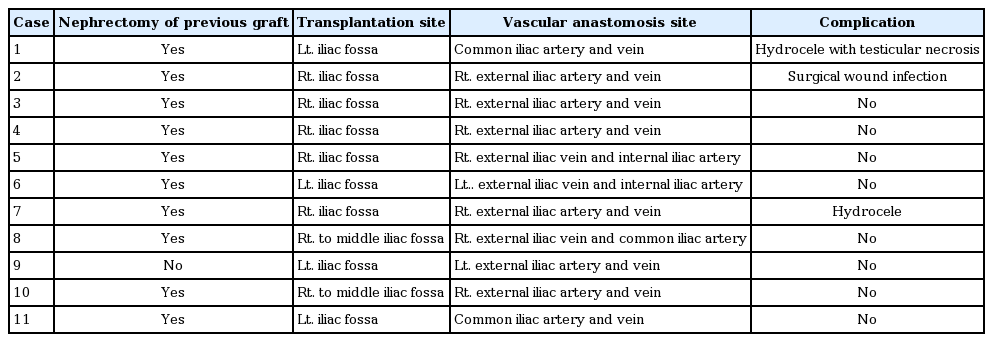
Surgical problems during the third KT procedure
Table 2 shows the surgical problems observed during the third KT procedure. A total of seven grafts (63.6%) were transplanted at the right iliac fossa, whereas the other four grafts (36.4%) were transplanted at the left iliac fossa during the third KT. Prior to the third KT, 10 patients underwent nephrectomy of the previous graft. Of these patients, we performed nephrectomy of the first and second grafts in three patients, the first graft only in four patients, and the second graft only in the remaining three patients. Various methods were used for vascular anastomosis (Table 2). The right external iliac artery and vein were used in five patients (45.5%), whereas the common iliac artery and vein were used in two patients (18.2%). The left external iliac artery and vein, right external iliac vein and internal iliac artery, left external iliac vein and internal iliac artery, and right external iliac vein and common iliac artery were each used in one patient. Surgical complications were observed in three patients (27.3%). One patient each had hydrocele with testicular necrosis, mild hydrocele, and a surgical wound infection with Pseudomonas aeruginosa and Aspergillus sp., all of which were treated without sequelae.
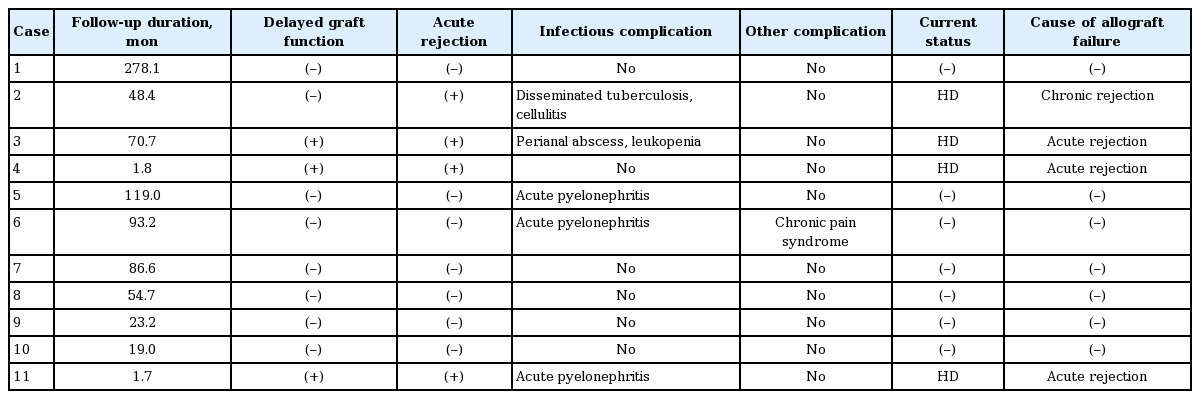
Medical problems after the third KT procedure
The total follow-up duration after KT was 72.4 ± 78.3 months. Three cases of delayed graft function were noted. A total of seven episodes of infectious complications developed in five patients, which required hospitalization (Table 3). One patient (patient 2) developed disseminated tuberculosis and cellulitis. Another patient developed a perianal abscess and leukopenia that was resolved after discontinuation of mycophenolate mofetil (MMF). The remaining three patients developed acute pyelonephritis. Acute rejection was observed in four patients (36.4%); three of these experienced allograft loss. One patient developed chronic pain syndrome, which presented with leg pain and numbness.
Allograft and patient outcome after the third KT procedure
The patients’ clinical outcomes are presented in Table 3. During follow-up, allograft failure developed in a total of four patients owing to acute rejection in three patients and chronic rejection in one patient. Therefore, the 1- and 5-year allograft survival rates were 81.8% and 42.9%, respectively. However, none of the patients died during the follow-up period. We divided the patients into two groups, as follows: cases in which the KT was performed prior to the use of tacrolimus and MMF (pre-tacrolimus/MMF group; in this group, azathioprine or cyclosporine was used), and cases in which KT was performed with the use of tacrolimus and MMF (tacrolimus + MMF group). Four patients who underwent KT developed allograft failures, among whom only one patient was in the tacrolimus + MMF group; the other three patients were in the pre-tacrolimus/MMF group. The allograft survival rate was superior in patients in whom tacrolimus was used than in those in whom tacrolimus and MMF were not used (Fig. 2).

Comparison of allograft survival rates between the pre-tacrolimus/MMF and tacrolimus + MMF groups. The tacrolimus + MMF group showed a higher 10-year allograft survival rate. Pre-tacrolimus/MMF:KT performed prior to the use of tacrolimus and MMF (azathioprine or cyclosporine was used); tacrolimus + MMF:KT performed with the use of tacrolimus and MMF. MMF, mycophenolate mofetil; KT, kidney transplantation.
Third allograft survival rates at 1, 5, and 10 years were 81.8%, 42.9%, and 42.9%, respectively. We compared the first and second allograft survival rates to that of the third allograft. The survival rate of the third allograft was higher than those of the first and second allografts in these patients (p = 0.034), but the strength of this conclusion is limited by the small number of patients included in the study (Fig. 3).
DISCUSSION
Despite significant advances in transplantation techniques and immune suppressants, renal allograft survival rates remain low. In this regard, re-transplantation is beneficial for those patients in terms of survival and quality of life [6,9]. At our centers, the survival rate of the second graft was not inferior to that of total primary transplantation or the findings of previous reports [12-14,17,18]. However, the clinical outcomes of a third KT procedure have not been established, and various medical and surgical issues regarding a third KT procedure remain to be resolved [17].
Many patients belong to an immunologically high-risk group. Indeed, the most characteristic finding among patients who underwent a third KT procedure in this study was the high rate of sensitization. Of the five patients who underwent a PRA test, four had a PRA value > 50% and four of nine LDKT recipients (44.4%) showed a positive cross-match result, and therefore required pre-transplant desensitization therapy. In addition, the cause of allograft failure was acute rejection in three of four patients who developed allograft failure, which is consistent with earlier reports of high sensitization and allograft loss rates due to acute rejection [16,19,20].
Second, the manipulation of the previous transplant may involve technical difficulties and various surgical problems. Indeed, the surgical complication rate after a third KT procedure was higher than that after the first KT procedure; for example, the rates of vascular thrombosis, urinary obstruction, and vessel injury were higher in patients who underwent a third KT procedure than in those who underwent a first KT procedure [15,17]. Kidney grafts are usually placed in the right iliac fossa because this approach is easier than that on the left side as it avoids the sigmoid colon [21,22]. However, in patients undergoing a third KT procedure, allografts must be positioned in the previously manipulated space with restricted access to the iliac vessels because of the prior transplantation. Therefore, nephrectomy of the previous graft is required to ensure sufficient space for the third graft, which can result in further surgical complications.
In most of the cases in our study, the right external iliac artery and vein were used and nephrectomy of the previous graft was performed. Therefore, various complications, such as perirenal hematoma and hydrocele with testicular necrosis, developed. Various alternative methods have been suggested, such as the use of the common iliac vessels and inferior vena cava instead of the iliac vessels, and some studies have recommended orthotopic techniques [23,24]. However, none of these methods exhibit clear superiority to the others; therefore, technical issues might develop during the third transplantation [13,15,25,26].
A total of four patients experienced allograft loss during the follow-up period, and the allograft survival rates at 1 and 5 years were 81.8% and 42.9%, respectively. However, most (75%) allograft failures developed in patients in whom tacrolimus and MMF were not used. Among those who underwent KT after using tacrolimus and MMF, allograft failure did not develop in LDKT recipients, and only one instance of allograft failure developed in DDKT recipients. Indeed, the graft survival rate of the tacrolimus + MMF group was higher than that of the pre-tacrolimus/MMF group (Fig. 2). This suggests that a third KT shows favorable outcomes with the currently used immune-suppressant regimen comprising tacrolimus and MMF [27,28].
In previous studies from other countries, the proportion of deceased donors has been considerably higher than that of living donors [15,17]. However, in our study, the majority of third KT procedures were performed using grafts from living, related donors. One reason for this was the fact that most Korean families prior to the 1990s had more than five members, meaning that sufficient donor sources were available within a family, even for second and third KT procedures [29]. However, with the change in Korean families to a “nuclear family” model, the proportion of living, related donors has decreased, whereas the proportions of spousal and deceased donors have increased [30]. This suggests that living, related donors will not be a major donor source for the second or third transplants in the near future.
The need for desensitization and previous long-term use of immune suppressants may result in non-immunologic complications such as infection, cardiovascular issues, and posttransplant malignancies. In this study, cardiovascular mortality and posttransplant malignancy were not detected; only infectious complications, which were treated without sequelae, were observed. This suggests that strict and regular monitoring may prevent fatal complications associated with the long-term use of intense immune suppression.
The limitations of this study were the small number of patients enrolled and the performance of transplantations at different time points. Nevertheless, the follow-up duration in most cases was > 10 years; therefore, various immunologic and non-immunologic complications, which can develop not only immediately after KT but also during long-term follow-up, were evaluated.
In summary, the clinical outcomes of the third KT procedure are acceptable, especially with currently used immune-suppressant regimens and desensitization techniques. Various medical and surgical complications were detected, but most were treated without sequelae and did not affect allograft or patient outcomes. Therefore, we suggest that a third KT procedure could be a valuable option for patients who experience a second allograft failure.
KEY MESSAGE
1. A third kidney transplantation procedure is associated with both immunologic and non-immunolo gic complications.
2. However, the clinical outcomes are acceptable, especially when current immune suppressant regimens and desensitization techniques are used.
3. Complications do not affect the long-term clinical outcomes of a third kidney transplantation.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This study was supported by a grant (HI13C1232) from the Korean Health Technology R&D Project, Ministry of Health and Welfare, Republic of Korea.