Kinetics of T-cell-based assays on cerebrospinal fluid and peripheral blood mononuclear cells in patients with tuberculous meningitis
Article information
Abstract
Background/Aims
The goal of this study was to monitor tuberculosis (TB)-specific T-cell responses in cerebrospinal fluid-mononuclear cells (CSF-MCs) and peripheral blood mononuclear cells (PBMCs) in patients with tuberculous meningitis (TBM) over the course of anti-TB therapy.
Methods
Adult patients (≥ 16 years) with TBM admitted to Asan Medical Center, Seoul, South Korea, were prospectively enrolled between April 2008 and April 2011. Serial blood or CSF samples were collected over the course of the anti-TB therapy, and analyzed using an enzyme-linked immunosorbent spot (ELISPOT) assay.
Results
Serial ELISPOT assays were performed on PBMCs from 17 patients (seven definite, four probable, and six possible TBM) and CSF-MC from nine patients (all definite TBM). The median number of interferon-gamma (IFN-γ)-producing T-cells steadily increased during the first 6 months after commencement of anti-TB therapy in PBMCs. Serial CSF-MC ELISPOT assays revealed significant variability in immune responses during the first 6 weeks of anti-TB therapy, though early increases in CSF-MC ELISPOT results were associated with treatment failure or paradoxical response.
Conclusions
Serial analysis of PBMCs by ELISPOT during the course of treatment was ineffective for predicting clinical response. However, increases in TB-specific IFN-γ-producing T-cells in CSF-MC during the early phase of anti-TB therapy may be predictive of clinical failure.
INTRODUCTION
Mycobacterium tuberculosis-specific interferon-γ (IFN-γ) releasing assays (IGRAs) are an effective method for diagnosing tuberculous meningitis (TBM) in both peripheral blood mononuclear cells (PBMC) and cerebrospinal fluid mononuclear cells (CSF-MC) [1,2,3,4]. Serial analysis of tuberculosis (TB)-specific IFN-γ-producing T-cell responses by IGRA over the course of anti-TB therapy may be useful in predicting clinical response [5,6,7,8,9]; however, it is uncertain whether such an analysis would be beneficial in patients with TBM. Here, we evaluated TB-specific T-cell responses in CSF-MC and PBMCs using an enzyme-linked immunosorbent spot (ELISPOT) assay in patients with TBM during the course of anti-TB therapy.
METHODS
Study design and patients
Adult patients (≥ 16 years) with suspected TBM admitted to Asan Medical Center, a 2,700-bed tertiary hospital in Seoul, South Korea, were prospectively enrolled between April 2008 and April 2011. Patients with suspected TBM were categorized as definite, probable, or possible TBM, according to a recently proposed uniform case definition, with some modifications [10]. In brief, patients were classified as having "definite TBM" if clinical specimens were found to be positive for M. tuberculosis either by culture or through the use of an M. tuberculosis polymerase chain reaction assay. Patients were classified as having "probable TBM" or "possible TBM" according to the diagnostic scoring system [10]. All patients received standard TB therapy in accordance with the recommendations of the American Thoracic Society [11]. Only patients willing to provide serial blood or CSF samples over the course of anti-TB therapy were included in the final analysis. The study protocol was approved by the Institutional Review Board of Asan Medical Center.
ELISPOT assay
PBMCs and CSF-MCs were isolated from peripheral venous blood (~8 mL) and CSF (~4 mL), respectively, within 30 minutes of collection. Cells were then resuspended in appropriate medium, and analyzed using an ELISPOT assay (T-SPOT.TB, Oxford Immunotec, Oxford, UK) as described previously [1,12]. The minimum threshold for a positive response was defined as ≥ 6 spot-forming cells per well (SFCs) after subtraction of the negative control. Indeterminate responses were defined as < 20 spots in the positive control well, or > 10 spots in the negative control well [1,12].
RESULTS
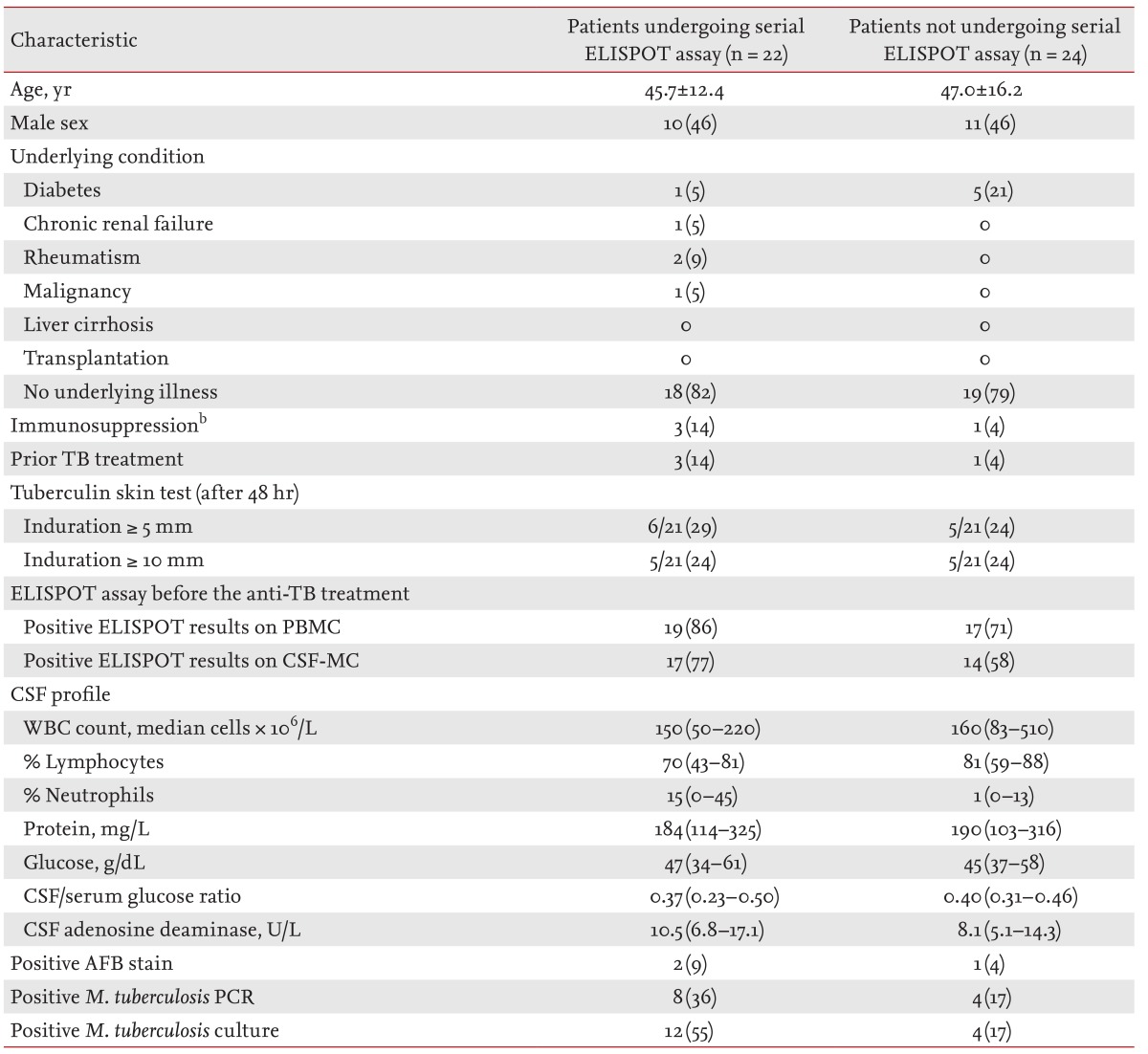
Forty-six patients with TBM were prospectively enrolled during the study period. Of these 46 patients, 17 (37%), 8 (17%), and 21 (46%) were classified as having definite, probable, and possible TBM, respectively. Baseline ELISPOT assays were performed on PBMCs and CSF-MCs from all 46 patients; however, only 22 of these patients were willing to provide serial samples over the course of their treatment. Baseline clinical characteristics were similar between patients providing serial samples and those providing only pretreatment samples (Table 1).
Serial PBMC ELISPOT assays were performed on 17 patients (seven definite, four probable, and six possible TBM). Among the 15 patients exhibiting positive ELISPOT results at baseline, no negative reversions (< 6 spots) were observed during the course of treatment; positive conversion (≥ 6 spots) occurred in one of two patients initially diagnosed as negative by ELISPOT. Median IFN-γ-producing T-cell numbers steadily increased during the first 6 months after commencement of anti-TB therapy in these patients (Fig. 1).
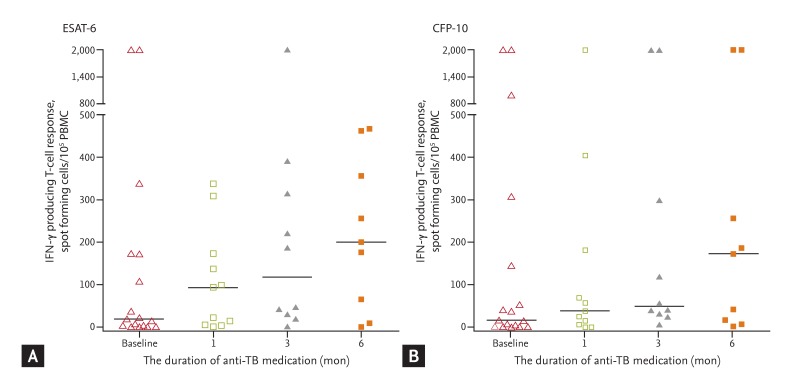
Serial (A) early secreting antigenic target-6 (ESAT-6) and (B) culture filtrate protein-10 (CFP-10) responses in peripheral blood mononuclear cell (PBMC) enzyme-linked immunosorbent spot assays after initiation of anti-tuberculosis (TB) therapy in 17 patients with tuberculous meningitis. Horizontal bars denote medians. IFN-γ, interferon-γ.
Serial CSF-MC ELISPOT assays were performed on nine patients with TBM (all definite TBM). Serial changes in the number of IFN-γ-producing T-cells were associated with both white blood cell (WBC) counts and clinical responses (Fig. 2). IFN-γ-producing T-cell counts decreased in four patients with decreasing CSF WBC counts (patients 1 to 4), but increased in four others exhibiting increased CSF WBC counts (patients 6 to 9); one patient (patient 5) exhibited no change in IFN-γ-producing T-cell numbers despite a decrease in CSF WBC counts. None of the five patients, in whom IFN-γ-producing T-cells decreased or remained constant during the early phase of anti-TB therapy, experienced a worsening of clinical symptoms; however, all four patients with definite TBM, in whom IFN-γ-producing T-cells increased, exhibited clear signs of clinical deterioration.
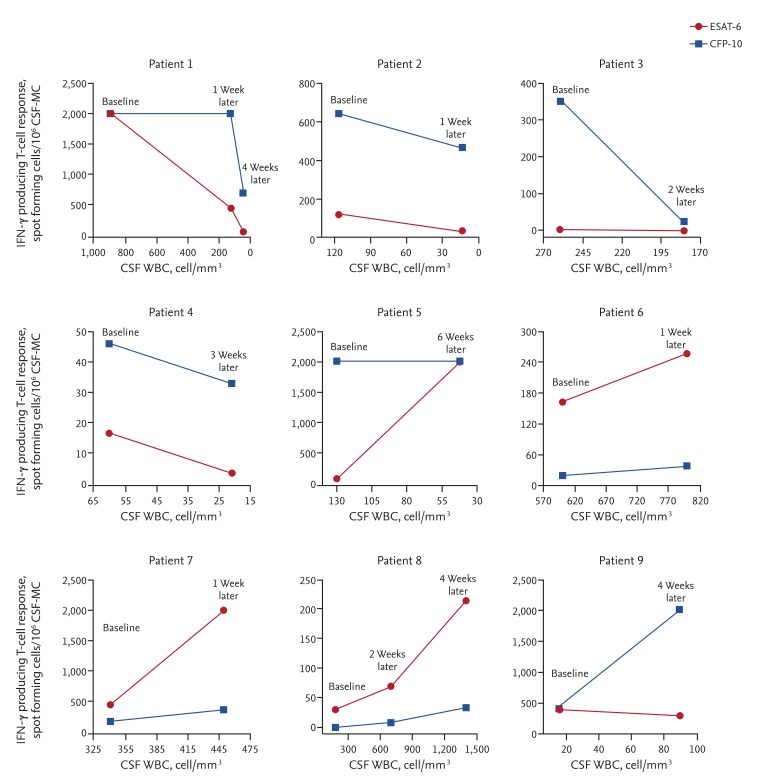
Serial cerebrospinal fluid-mononuclear cell (CSF-MC) enzyme-linked immunosorbent spot assays after initiation of anti-tuberculosis (TB) therapy in nine patients with definite tuberculous meningitis. Note that the CSF white blood cell (WBC) counts on the X-axis decrease from left to right in patients 1 to 5 but increase in patients 6 to 9. Of the four patients (patients 6 to 9) in whom interferon-γ (IFN-γ) producing T-cells increased, two (patients 6 and 9) died despite anti-TB therapy, while the other two (patients 7 and 8) experienced paradoxical responses. ESAT-6, early secreting antigenic target-6; CFP-10, culture filtrate protein-10.
DISCUSSION
Analyses of serial TB-specific IFN-γ-producing T-cell responses in CSF-MCs and PBMCs of patients with TBM remain limited. Here, we showed that TB-specific IFN-γ-producing T-cell responses in PBMC increased steadily over the course of 6 months after initiation of anti-TB therapy. This finding is consistent with a previous ELISPOT analysis performed by our laboratory in which median TB-specific T-cell responses were shown to increase steadily for up to 6 months in 52 patients with extrapulmonary TB, followed by a decrease thereafter [13]. A more complete comparison was not possible however, as long-term follow-up (> 6 months) in patients with TBM was not performed.
While some studies have reported increased T-cell responses during or after anti-TB therapy [13,14,15,16,17], consistent associations between anti-TB therapy and an attenuated T-cell response in PBMCs have also been observed [5,6,7,8,9,18,19,20]. The reasons underlying this discrepancy, along with the small number of negative reversions with increased T-cell responses described in this study are not clear. One possible explanation may be that extrapulmonary TB is more likely to exhibit a paradoxical response to anti-TB therapy [21]. Most studies examining IGRA kinetics during anti-TB therapy have focused exclusively on pulmonary TB [5,6,8,15,16,17,19,20], which may explain some of the different response kinetics observed in our studies. Further studies will be necessary to evaluate differences in immune response kinetics between pulmonary and extrapulmonary TB.
In addition to PBMC-related effects, we also observed increased TB-specific T-cell responses in CSF-MC during the early phase of anti-TB treatment, which were associated with clinical deterioration in patients with definite TBM. Previously, we had reported a case of TBM in which a therapy-induced increase in TB-specific T-cell responses in CSF-MC and PBMCs occurred [22]. Taken together, these studies suggest that the clinical deterioration seen during the early phase of TB therapy may be the result of TB-specific T-cell responses. Interestingly, these heightened T-cell responses occurred not only in patients who died as a result of TBM but also in those who experienced clinical deterioration despite CSF sterilization, but ultimately improved without modification to their anti-TB regimen (i.e., paradoxical response). These observations are consistent with our earlier work showing that an "immunologic paradox" often preceded a "therapeutic paradox," which is strongly predictive of poor outcomes [22]. Further studies will be needed to evaluate the prognostic value of increased TB-specific T-cell responses during anti-TB therapy, and the clinical utility of this phenomenon in patients with TBM.
Like all studies, this work is not without limitations. Ten of the seventeen patients (59%) in whom serial PBMC ELISPOT assays were performed were classified as having probable or possible TBM on the basis of clinical features and image findings alone, in the absence of microbiological confirmation. However, as existing bacteriological methods are not sufficiently sensitive to be used for diagnosing TBM alone, the majority of studies include patients based upon a combination of microbiological, clinical, and radiological criteria [1,23,24]. These patients were subsequently classified using a recently proposed uniform case definition as a way to minimize selection bias [10]. Second, serial ELISPOT assays were performed in only a small number of patients with TBM. Although a clear trend towards increased T-cell responses in PBMCs was observed during the anti-TB therapy, the small sample size was insufficient for most statistical analyses. Finally, CSF-MC ELISPOT assays were not performed at regular intervals. Further studies should include a larger number of patients with serial measurement performed at regular intervals.
Despite these limitations, this study may be useful for understanding the immunologic response to anti-TB therapy in patients with TBM. Serial analysis of PBMCs by ELISPOT during the course of treatment was found to be ineffective for predicting clinical response; however, increases in TB-specific IFN-γ-producing T-cells in CSF-MC during the early phase of anti-TB therapy may be predictive of clinical failure.
KEY MESSAGE
Serial peripheral blood mononuclear cell enzyme-linked immunosorbent spot assays during the course of treatment were found to be ineffective for predicting clinical response in patients with tuberculous meningitis (TBM).
Increases in tuberculosis (TB)-specific interferon-gamma producing T-cell response on cerebrospinal fluid-mononuclear cells during the early phase of anti-TB therapy may be predictive of clinical failure in patients with TBM.
Acknowledgments
This study was supported by the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (grant number: 2011-A110004).
Notes
No potential conflict of interest relevant to this article was reported.