Current status of functional dyspepsia in Korea
Article information
Abstract
Dyspepsia refers to group of commonly occurring upper gastrointestinal symptoms. The majority of patients with dyspepsia suffer from functional (nonulcer) dyspepsia. Although there is a lack of epidemiological data from population-based or patient cohort studies in Korea, the current understanding of this condition has been updated using data from various recent research studies, which have facilitated the development of clinical guidelines for functional dyspepsia. According to a survey using the Rome III criteria, more than 40% of respondents who visited primary clinics and tertiary hospitals were defined as having functional dyspepsia, most of who were within a subgroup of patients with postprandial distress syndrome. In addition, a population-based cross-sectional survey revealed considerable overlap between functional dyspepsia and other functional gastrointestinal disorders, including gastroesophageal reflux disease (especially nonerosive reflux disease) and irritable bowel syndrome. In contrast to the results of Western trials, there is insufficient evidence to recommend a Helicobacter pylori test-and-treat strategy as an initial management approach to functional dyspepsia in Korea, suggesting the need for early endoscopic evaluation. Additional studies are necessary to adjust the cutoff age for implementation of immediate endoscopic evaluation of patients without alarm symptoms. Considering the prevalence of H. pylori infection and the limited efficacy of symptomatic relief after its eradication, further well-qualified studies in Korea are warranted.
INTRODUCTION
It is well known that functional gastrointestinal (GI) disorders, such as functional dyspepsia (FD) and irritable bowel syndrome (IBS), have a considerable negative socioeconomic impact [1-4]. Although there are limited data regarding the disease burden of functional GI disorders in Korea, an economic analysis of the National Health Insurance Corporation database suggested that these disorders represent a severe burden and are associated with high morbidity in outpatients [5]. FD, which is one of the most common GI disorders encountered in clinical practice, is defined by the Rome III criteria as the presence of chronic dyspeptic symptoms for the previous 3 months, an onset of at least 6 months before diagnosis, and the absence of any structural abnormality (determined by upper GI endoscopy), metabolic cause, or systemic cause explaining the symptoms [6,7]. Multiple theories have been proposed to describe the underlying pathophysiology of FD symptoms, including dysmotility and/or hypersensitivity in the upper GI tract [8].
Many studies have reported the prevalence of FD in population-based settings. However, because the diagnosis is influenced by the criteria used to define FD and by the presence of overlapping disorders, the results of such studies are varied. Although there is a lack of qualified research on FD in Korea, recent progress (e.g., inclusion of data from nationwide studies and the suggestion for clinical guidelines) is enhancing our understanding of Korean FD [9,10]. The aim of this review was to describe the current status of FD in Korea from the perspectives of epidemiology, diagnosis, and Helicobacter pylori infection.
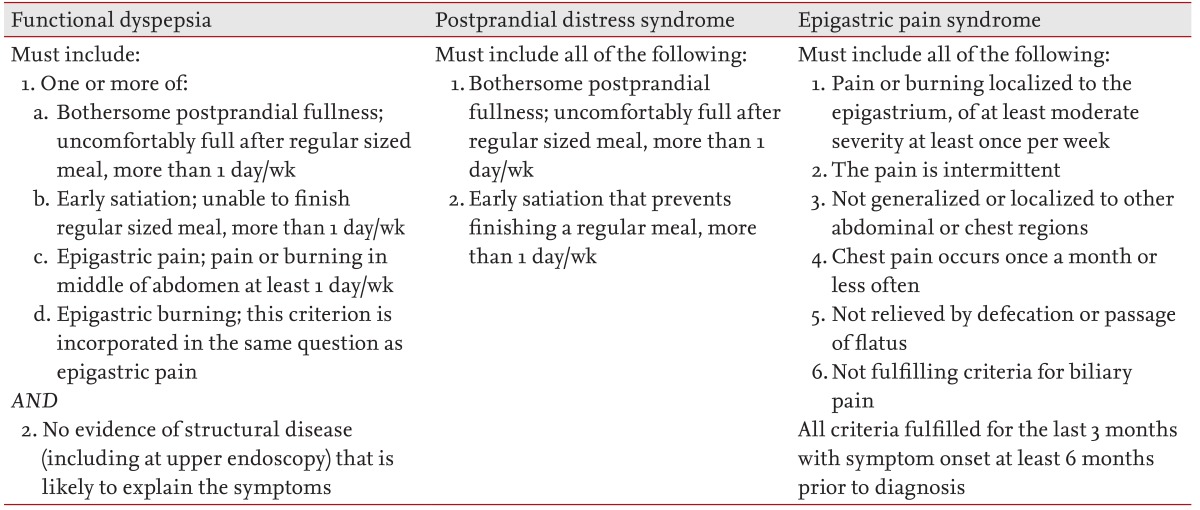
FD DEFINITIONS
According to the Rome III consensus, FD is defined as the presence of early satiation, postprandial fullness, epigastric pain, or epigastric burning in the absence of an organic, systemic, or metabolic disease that could explain the symptoms (Table 1). This definition differs from previous Rome consensus definitions in that it is limited to only four symptoms that are considered to be key dyspeptic symptoms [6,7]. The number of key symptoms was decreased to four in the Rome III consensus to improve the specificity of the symptom cluster to the gastroduodenal region. Based on population-based and patient cohort studies, the Rome III consensus proposed distinguishing postprandial distress syndrome (PDS) from epigastric pain syndrome (EPS) [6,11-13]. EPS and PDS are thought to have different pathophysiologies because, unlike EPS, PDS appears to be associated with impaired gastric accommodation and increased duodenal eosinophil counts [14]. As such, these two syndromes might have different responses to medication, and distinguishing the two diagnoses would allow for a more rational approach to drug discovery and development. However, the therapeutic implications of this subdivision remain to be clarified.
EPIDEMIOLOGY AND ISSUES OF OVERLAPPING DISORDERS
The prevalence of uninvestigated dyspepsia varies from 7% to 45% worldwide, and many epidemiological studies globally support the Rome III classification of EPS and PDS subtypes based on a better-than-expected separation of these subgroups in the general population [15,16]. However, a recent report on primary care patients found that EPS and PDS subtypes overlap in the majority of patients with FD, indicating that the value of dividing FD into EPS and PDS subgroups is ineffective [17].
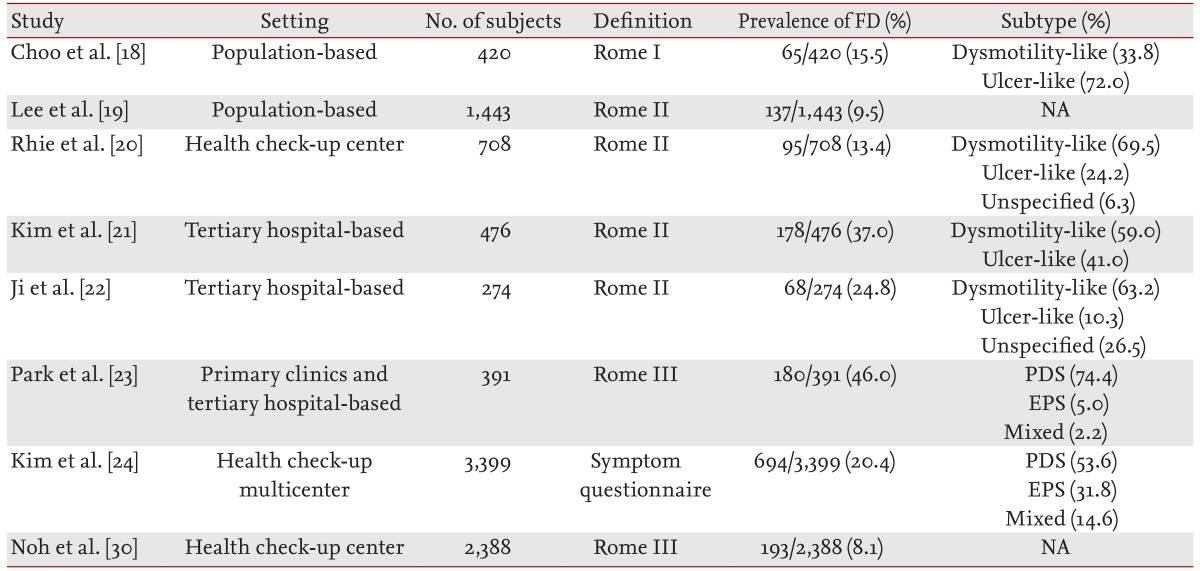
In Korea, the prevalence of FD as assessed by the Rome I criteria in a rural community was reportedly 15.5%, and the prevalence determined from a population-based study using the Rome II criteria was 9.5% [18,19]. In addition, the prevalence of FD in patients undergoing health check-ups in Korea was estimated as 13.4% according to the Rome II criteria. In this analysis, the most common subtype of FD was dysmotility-like dyspepsia (69.5%) [20]. Two tertiary hospital-based studies revealed prevalences of 37.0% and 24.8%, respectively [21,22]. In another point-prevalence study of FD using the Rome III criteria, 46.5% and 45.8% of respondents who visited primary clinics and tertiary hospitals, respectively, were diagnosed with FD [23]. This report showed that 74.4% of all cases were defined as PDS, 5.0% as EPS, 2.2% as mixed, and 18.3% as an undetermined subtype. The prevalences of FD from various Korean studies are presented in Table 2. The mixed subgroup percentage in this report was much lower than those reported in Western studies [13,17]. A recent Korean nationwide, multicenter report on the prevalence of FD in patients undergoing health check-ups (FD not determined using the Rome criteria) revealed a 20.4% prevalence of FD symptoms among seven healthcare screening centers in Korea. In this study, atrophic gastritis and positive serology for H. pylori infection were not associated with the prevalence of FD, suggesting that FD is a multifactorial disease [24].
Upper and lower GI symptoms commonly overlap, and psychological disorders (e.g., anxiety, neuroticism, and somatization) have been reported in both patients with FD and in those with IBS [25,26]. Overlap between functional GI disorders may be a manifestation of generalized motor disturbances, altered visceral sensitivity, and/or brain-gut dysfunction [27,28]. In a population cross-sectional survey of Korean subjects, overlaps between FD and gastroesophageal reflux disease (GERD) and between FD and IBS were observed in 2.3% and 1.3% of the population, respectively. In addition, 24% and 14% of dyspeptic subjects had GERD and IBS, respectively [28]. These overlaps occurred predominantly in individuals with anxiety. In particular, a depressive mood was significantly related to FD-IBS overlap based on the Rome III criteria. Patients with FD-IBS overlap appeared to have poorer quality of life than did patients with FD or IBS alone [29]. A report regarding the overlap of FD and GERD in patients undergoing health screening revealed that FD occurred more frequently in patients with nonerosive reflux disease than in patients with reflux esophagitis (74.3% vs. 10.5%, respectively). In addition, the EPS and PDS subtypes overlapped more commonly with nonerosive reflux disease than with reflux esophagitis, and EPS was more prevalent than PDS in patients with nonerosive reflux disease (68.9% vs. 48.6%, respectively) [30].
Several genetic studies have suggested that serotonin transporter gene polymorphisms and G-protein β3 C825T gene polymorphisms are associated with functional GI disorders [31,32]. However, in a few Korean studies, no relationship was found between these genetic polymorphisms and FD, including overlap [33,34]. In contrast, a pediatric study showed that the CC genotype of G-protein β3 C825T may be associated with FD in Korean children [35].
VALIDATION OF THE ROME III CRITERIA AND DIAGNOSTIC QUESTIONNAIRE
In a validation study in a Western population, the Rome III criteria were not sufficiently sensitive to differentiate functional GI disorders from organic disease [36]. However, the criteria for subgroups of FD had good specificity [37]. An early validation study of the Rome III criteria in Korean subjects revealed that their sensitivity and specificity for discriminating functional GI disorders from organic diseases of the upper GI tract were 60% and 53%, respectively [38]. This finding supports the use of the Rome III criteria in Korea. A Korean version of the Rome III questionnaire was developed recently through structural translational processes; its good reliability and convergent validity suggested it to be useful for clinical and research assessments in the Korean population [39]. In addition, the Functional Dyspepsia-Related Quality of Life scale and a Korean version of the Bowel Disease Questionnaire have been validated in Korean patients with FD [40,41].
SYMPTOMS
A study that correlated dyspeptic symptoms with endoscopic findings showed that dyspeptic symptoms alone did not predict the presence or absence of organic disease [42]. According to a systematic review that evaluated whether clinical symptoms or socioeconomic factors can differentiate organic disease from FD before endoscopy, symptoms or socioeconomic factors have limited power in discerning organic disease from FD [43]. Another meta-analysis was conducted to determine whether alarm symptoms discern organic dyspepsia; alarm symptoms had a suboptimal sensitivity of 67% and specificity of 66% for detecting malignancy [44].
A Korean study that enrolled subjects who underwent upper GI endoscopy in a hospital or health screening setting showed that dyspepsia was not significantly associated with the presence of organic disease. However, male subjects with alarm symptoms had a statistically significant twofold increase in the relative risk of organic disease [45]. In this study, despite the increase in the relative risk of organic disease with age, a significant proportion of organic disease could have been missed. Together, these results show that organic disease in patients with dyspepsia is difficult to predict on the basis of sex, the presence or absence of alarm symptoms, and age. In a large-scale analysis at a health promotion center, ~40% of subjects with dyspepsia had abnormal endoscopic findings. In addition, the Rome III diagnostic criteria were useful in predicting the absence of significant upper endoscopic findings [46]. An investigation to verify whether endoscopic findings differ according to the symptoms of patients with FD showed that erythema and raised erosions were observed more frequently in the antrum of patients with EPS while atrophy was observed more frequently in the fundus of patients with PDS [47].
EARLY ENDOSCOPIC EVALUATION
According to the clinical guidelines of the American Gastroenterological Association, immediate endoscopy is recommended if alarm symptoms exist or the patient is > 55 years of age. If H. pylori eradication or protein pump inhibitor administration fails or a relapse occurs in patients ≤ 55 years of age, endoscopy is recommended [48]. The British guidelines are similar to the American guidelines [49]. The Canadian guidelines recommend immediate endoscopy for patients aged ≥ 55 years [50]. Such guidelines arose from comparative studies of early endoscopic evaluation and the H. pylori test-and-treat strategy [51,52].
Previous meta-analysis results indicated that there was no significant difference in symptom improvement between an early endoscopic evaluation strategy and the H. pylori test-and-treat strategy [49,53]. Age is the most important factor in determining the indications for the use of early endoscopic evaluation. Organic disease, particularly malignant disease, commonly occurs in older people; thus, the most effective age for endoscopy to detect organic disease differs based on epidemiological characteristics such as location or ethnicity [10,54]. The prevalence of gastric cancer is high (0.9% to 3.4%) in Asia, including Korea [55]. Because cancer occurs in both young and old people, the Asian guidelines regarding FD have a younger standard age for implementation of endoscopy than do the Western guidelines [56-59].
In Korea, studies on the cutoff age for immediate endoscopic evaluation are scant. Evaluation of alarm symptoms, performance of the H. pylori serum test, and performance of endoscopy for patients with dyspepsia revealed no malignancy in patients < 35 years of age; in contrast, malignancy was found in four patients aged ≥ 35 years [59]. However, because this study was limited by the small sample size and was conducted only in a tertiary hospital, additional studies are needed to determine the optimal cutoff age for implementation of early endoscopic evaluation in Korean patients with dyspepsia.
HELICOBACTER PYLORI TEST-AND-TREAT STRATEGY
The prevalence of H. pylori infection is currently decreasing in the West, and the incidences of peptic ulcers and gastric cancer are decreasing proportionately [60]. Given that gastric cancer was found in < 1% of patients who underwent upper GI endoscopy, the majority of cases of organic diseases associated with dyspepsia are regarded to involve peptic ulcers [10].
In a study of dyspeptic patients in primary care facilities in Canada, 30% of patients were positive for H. pylori infection, and organic disease was found in 58% of patients undergoing upper GI endoscopy [61]. In a study conducted in Europe, upon the completion of a urea breath test as an initial test for dyspepsia, the H. pylori status showed high diagnostic value in detecting peptic ulcers in patients suspected to have dyspepsia [62]. In addition to these findings, the worldwide clinical guidelines recommend the H. pylori test-and-treat strategy if the result of the H. pylori test as an initial test for dyspepsia is positive [63-66]. The national survey of H. pylori prevalence in Korea showed a trend toward reduction; the H. pylori prevalence rate in those aged ≥ 16 years was 66.9% in 1998, but 59.6% in 2005. Whereas 80.0% of patients with peptic ulcer disease who were referred to a tertiary institution for evaluation of dyspepsia were H. pylori-positive, only 20.2% among those diagnosed with FD were H. pylori-positive [67]. There was also a report that only 28.4% of those diagnosed with FD after undergoing comprehensive health screening were H. pylori-positive. However, this report was not representative because of the very low H. pylori prevalence [20]. Among patients who underwent endoscopy for evaluation of dyspepsia in tertiary medical facilities, the H. pylori prevalences were 86.7%, 77.8%, and 54.2% in those with peptic ulcer disease, gastric cancer, and nonulcer dyspepsia, respectively [68-70]. No observational study or randomized controlled study on whether an H. pylori test should be performed to diagnose FD in Korea has been performed. A study of use of a serum H. pylori test before endoscopy on Korean patients with FD revealed that among subjects younger than 40 years, sensitivity to organic disease was 76.7% and the negative predictive value was 85.8% when the H. pylori test was positive [71]. In subjects ≥ 40 years of age, the sensitivity was 61.9% and the negative predictive value was 64.0%. Therefore, the H. pylori test-and-treat strategy is expected to have low diagnostic value for dyspepsia in Korea. This issue played a critical role in the recently developed Korean clinical guidelines for H. pylori infection and FD in Korea [9,72].
HELICOBACTER PYLORI ERADICATION
In more than one study, H. pylori eradication resulted in longer-term symptom improvement in the FD patient group than in the placebo group [73,74]. A Cochrane review showed that the risk of symptom persistence was reduced significantly by 9% in the H. pylori eradication group compared with the placebo group [75]. In addition, a prospective study conducted in a primary medical facility showed that H. pylori eradication had a significant effect on symptom improvement in patients with FD [76]. In Asia, whether H. pylori eradication can improve FD is unclear because of insufficient evidence from studies with small sample sizes or nonrandomized protocols. Although a meta-analysis showed 3.6-fold symptom improvement in the H. pylori eradication group, evaluation of cost-effectiveness was limited due to the different costs of H. pylori eradication among the various regions [77]. Another analysis of 12 randomized studies showed that H. pylori eradication had good cost-effectiveness for FD [78]. Most guidelines worldwide recommend H. pylori eradication in some patients with FD, and all guidelines based on evidence regarding eradication in FD suggest that the data are of the highest quality [63-66].
There are no results from any randomized controlled studies on the effect of H. pylori eradication on FD in Korea [79]. A nonrandomized prospective study showed no difference in symptom improvement between the successful H. pylori eradication group and the failed group [80]. However, another study reported significant symptom improvement upon the completion of H. pylori eradication [81]. Other observational studies that evaluated parameters of gastric emptying or hypersensitivity did not show significant differences in symptoms, emptying, or hypersensitivity in patients with H. pylori infection [82-84]. The effect of H. pylori eradication on FD and the relationship between the changes in histological gastritis and FD symptom responses in Korea were evaluated recently, but the results suffered from a number of limitations, including the low sample size and the nonrandomized, non-double-blind design [85]. That study showed that H. pylori eradication (odds ratio [OR], 5.81) and symptom improvement at 3 months (OR, 28.90) were associated with improvement in dyspepsia at 1 year. Because the H. pylori infection rate is high in Korea, H. pylori eradication for all patients with FD might result in adverse events or development of antibiotic resistance. Furthermore, the benefits and risks of the treatment should be considered based on the cost-effectiveness [86]. From this viewpoint, the Korean clinical guidelines weakly recommend that H. pylori eradication may be helpful in long-term symptom improvement in only a proportion of patients with FD [9,72].
CONCLUSIONS
FD is a common disease that imparts a high socioeconomic burden. A few prevalence studies of FD using the Rome III criteria revealed that the PDS subtype was more prevalent than the EPS subtype in Korea. In addition, a cross-sectional population survey revealed considerable overlap between FD and other functional GI disorders, including GERD (particularly nonerosive reflux disease) and IBS. The recently developed Korean version of the Rome III questionnaire may be useful for diagnosing FD and performing clinical and research assessments in the Korean population. In contrast to results from Western trials, there is insufficient evidence that the H. pylori test-and-treat strategy is superior as an initial approach to FD in Korea. The results do, however, suggest the benefit of early endoscopic evaluation in Korea. However, additional studies are necessary to adjust the cutoff age for implementing immediate endoscopic evaluation of patients without alarm symptoms. When the benefits and risks, together with the cost-effectiveness, are taken into consideration, H. pylori eradication may be a therapeutic option for FD in Korea.
Notes
No potential conflict of interest relevant to this article was reported.