Neuropathic truncal pain in patients with type 2 diabetes mellitus relieved by topical cream and nerve block
Article information
To the Editor,
Neuropathy is common in patients with diabetes mellitus (DM). The condition involves several neurological systems resulting in a variety of symptoms and diverse treatments [1]. Truncal neuropathy is among the spectrum of peripheral neuropathies associated with DM. It manifests as localized chest or abdominal pain, which may be confused with referred pain from the intrathoracic or intra-abdominal organs [2], and when treated as such it may lead to extensive and unnecessary clinical investigations. Although truncal neuropathy is generally managed using oral medication, we report here successful treatment of truncal neuropathy in a patient with type 2 DM using a topical agent and nerve block. We also present a review of the literature.
A 50-year-old male presented at the emergency department of Chonbuk National University Hospital, South Korea, complaining of lower abdominal pain, such as burning and a lacerating pain, during the past 2 weeks. He complained of severe lancinating pain from the lower costal area to upper inguinal area, and his numeric rating scale (NRS) pain symptom score was 10. He had been diagnosed with type 2 DM 2 years previously and was prescribed premixed 70:30 insulin for 6 months. The patient was 168 cm tall, weighed 45 kg, and had smoked 20-pack years. On physical examination, the patient had no diarrhea, abdominal discomfort, fever, or skin lesions. During the previous 3 months, he experienced severe weight loss of 10 kg (20% of total body weight). Laboratory tests were as follows: complete blood count (white blood cell 6,240/µL, hemoglobin 12.8 g/dL, platelet 357 k), sodium 139 mmol/L, potassium 3.9 mmol/L, alanine transaminase 15 IU/L (normal range, 12 to 33), aspartate transaminase 18 IU/L (normal range, 5 to 35), erythrocyte sedimentation rate (ESR) 13 mm/hr (normal range, 0 to 9), highly sensitive C-reactive protein 0.2 mg/L (normal range, 0 to 5), hemoglobin A1c 95 mmol/mol (10.8%), fasting insulin 5.0 µU/mL (normal range, 2.6 to 24.9), C-peptide 1.17 ng/mL (normal range, 1.1 to 4.4), homeostasis model assessment for insulin resistance 2.5, and albumin to creatinine ratio 91.9 mg/g. He had nonproliferative diabetic retinopathy. Tumor marker and abdomen pelvic computed tomography were performed to screen for cancer. The scans revealed no evidence of cancer or intra-abdominal organ pathology. Furthermore, no abnormalities in rheumatic autoantibodies, such as rheumatoid factor or antinuclear antibodies, were found nor were there suspected symptoms of vasculitis or other connective diseases. Plain X-ray revealed no thoracolumbar spine abnormalities. The quantitative sensory test showed small and large fiber neuropathy at the upper and lower extremities. A nerve conduction study revealed sensorimotor polyneuropathy in the trunk. The patient was diagnosed with type 2 DM with triopathy involving truncal neuropathy. He was managed with pregabalin 300 mg/day, nortryptiline 50 mg/day, and α-lipoic acid 600 mg/day. After 2 weeks, his NRS symptom score improved to 3, and he was discharged. However, 3 months later, the patient complained of aggravation of the same abdominal wall. His neuropathic medications had not changed during this time. According to his self-monitored blood glucose values, fasting glucose was 80 to 110 mg/dL and postprandial glucose was 180 to 230 mg/dL using premixed insulin. He reported recently smoking and heavy alcohol consumption following a stressful situation. His pain symptom score increased to NRS 7. He complained of extreme aching, burning, and lancinating pain, which severely disrupted his daily activities. His current oral medication regime was not effective for reducing his pain, and the dose could not be increased because of side effects such as nausea and drowsiness. Thus, we prescribed topical capsaicin cream and a lidocaine patch. Furthermore, we performed an epidural nerve block at the 10 to 11 thoracic nerve using lidocaine, ropivacine, and triamcinolone. After 2 to 3 weeks of using this topical treatment, the patient's symptom score improved to NRS 2. He was maintained on topical capsaicin cream, lidocaine patch, and pregabalin and was able to decrease his dose of nortryptiline to 10 mg/day and discontinue α-lipoic acid.
Peripheral neuropathy is a common microvascular complication of DM. It presents in various ways such as peripheral sensory neuropathy, motor neuropathy, and autonomic neuropathy. Factors commonly associated with peripheral neuropathy are being male, a smoker, long duration of DM, and poor glycemic control. Painful diabetic neuropathy is best managed by maintaining good control of glucose level and using medication to relieve painful symptoms [3]. Truncal neuropathy is a type of acute painful neuropathy. It presents as an acute onset pain in a dermatomal distribution over the thorax or the abdomen [2]. The acute asymmetrical pain may be associated with local bulging of the abdominal wall. Lauria et al. [4] compared symptomatic and non-symptomatic skin biopsies from three patients with truncal neuropathy to investigate the neuropathological features of truncal neuropathy. They found the loss of intraepideraml nerve fiber densities and the presence of degenerative changes in dermal nerve fibers associated with truncal neuropathy. Furthermore, the lesions were correlated with the subjective sensory symptoms. We did not assess nerve fiber changes before and after treatment using nerve biopsy; thus, the relationship between topical agents and neuropathy must be clarified in future studies.
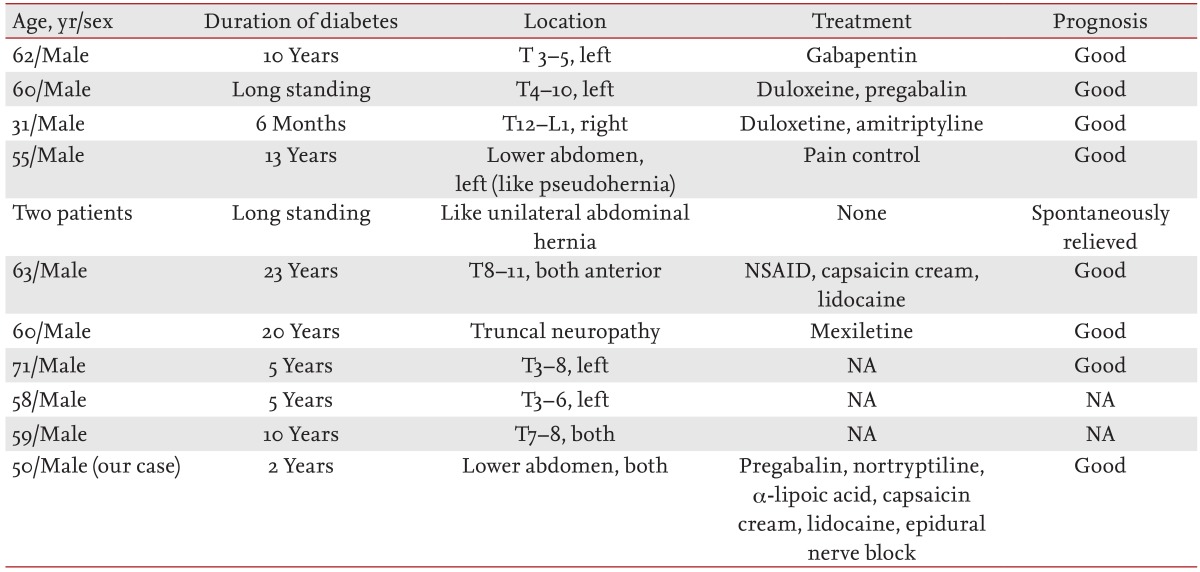
Several cases of truncal neuropathy in patients with DM have been reported previously (Table 1). Most patients have been male with a DM duration > 2 years, and the neuropathy has primarily been unilateral. Three cases have shown abdominal wall weakness similar to an abdominal hernia. About half of patients had used systemic oral pain medications to control pain, as in the present case. However, the present case is the only one to have used the topical medications capsaicin cream and lidocaine to control pain. Most previous patients have had a good prognosis, and the pain spon taneously remitted in two patients so they did not require further pain relief medication. Our patient improved following the administration of systemic oral medication, topical cream, and epidural nerve block.
Diabetic peripheral neuropathy is typically managed by controlling blood glucose levels and administering tricyclic antidepressants, anticonvulsants, α-lipoic acid, opioids, and topical agents. Furthermore, truncal neuropathy may be managed using oral medications such as gabapentin, pregabalin, and duloxetin (Table 1). Truncal neuropathy pain generally improves completely 3 to 12 months following treatment. However, our patient experienced severe acute pain, which significantly disrupted his sleep and daily activities. Thus, we used systemic oral medications, topical agents, and an epidural nerve block to treat his pain, which was successfully relieved after 2 to 3 weeks. Epidural nerve block is generally used to control cancer pain and irreversible neuropathy pain [5]; however, our case indicates that epidural nerve block may be effective for patients with inadequate pain control after optimal use of systemic medications or intolerance to systemic analgesic side effects. It is important to manage the appropriate patient for nerve block because postprocedure neuritis or deafferentation neuralgia may develop in some patients. Epidural nerve block has not previously been used in patients with DM, possibly because some diabetic peripheral nerve damage may be reversible. However, as our patient demonstrates, topical epidural nerve block may be an effective treatment for patients who have severe truncal neuropathy that is not controlled by oral medications or for those who cannot tolerate their medications. Further studies on the efficacy of nerve block for the management of truncal neuropathy in patients with DM are warranted.
To the best of our knowledge, our patient is the first case of truncal neuropathy successfully managed using topical cream and epidural nerve block.
Notes
No potential conflict of interest relevant to this article is reported.