Recent trends in hepatitis B virus infection in the general Korean population
Article information
Abstract
Background/Aims
Hepatitis B virus (HBV) is the major cause of chronic liver disease in Korea, but viral prevalence has decreased because of hepatitis B vaccination programs. In this study, we investigated longitudinal changes in HBV in fection in the general Korean population.
Methods
HBV surface antigen (hepatitis B surface antigen, HBsAg) seropositivity was assessed from the Korea National Health and Nutrition Examination Survey (I to V). In total, 50,140 subjects were tested for serum HBsAg positivity over a period of 12 years (1998 to 2010).
Results
The prevalence of HBsAg seropositivity decreased over the study period. The rates of HBsAg carriers were 4.61% in 1998, 4.60% in 2001, 3.69% in 2005, 3.01% in 2008, and 2.98% in 2010 (p < 0.0001). The reduction in HBV infection rates was more prominent in younger age groups. Among teenagers (10 to 19 years), the percentage of HBsAg carriers decreased from 2.2% in 1998 to 0.12% in 2010 (p < 0.0001). Among those aged 10 to 39 years, the percentage of HBV infection decreased from 4.72% in 1998 to 2.29% in 2010 (p < 0.0001). However, no decreasing trend in HBsAg positivity was observed among those aged 50 or older (p > 0.05). Neither gender nor socioeconomic status were associated with the decreased prevalence of HBsAg carriers.
Conclusions
HBV infection has decreased in the Korean population since the advent of vaccination programs. However, the decrease is limited to the younger population, and viral persistence remains in the middle-aged and older population.
INTRODUCTION
Hepatitis B virus (HBV) is the leading cause of acute hepatitis, chronic hepatitis, cirrhosis, and hepatocellular carcinoma (HCC) in South East Asia, China, and sub-Saharan Africa [1]. The prevalence of HBV infection in these regions ranges from 5% to 20% [2]. Seropositivity for hepatitis B surface antigen (HBsAg) was estimated at 8% to 9% in males and 5% to 6% in females in the 1980s [3]. The introduction of hepatitis B vaccination has dramatically decreased acute and neonatal HBV infection in many countries. In Korea, universal vaccination of all infants has been performed since 1991 and nationwide strategies have been implemented since 1995 [4]. Prior to the introduction of the vaccination program, approximately 8% of the general Korean population was HBsAg-positive [5]. Following the introduction of HBV vaccination, HBsAg prevalence rates have decreased, from 10% in the 1980s to 3.8% in 2007 in the general population [6]. This rate decreased further, to 0.4% in teenagers and 0.2% in children younger than 10 years [7]. Korea is now classified as an intermediate HBV endemic area (2% to 7% prevalence) [6].
Although the prevalence of HBV has decreased, few epidemiological studies have investigated changes in HBV infection rates and the related demographic or environmental factors. Some Korean studies have been conducted using nonrepresentative or small samples from selected communities. Since 1998, a nationwide survey, named The Korea National Health and Nutrition Examination Survey (KNHANES), has been conducted. This survey is based on a representative sample of the entire population to provide national health and nutritional status statistics. Considering the adverse effects of HBV on public health, the KNHANES has included serological markers for HBsAg and anti-HBs.
In the present study, we investigated recent epidemiological changes in HBV infection rates and related clinical and demographic factors. The results may be useful in establishing public health policies against HBV infection and its comorbidities in Korea.
METHODS
Subject
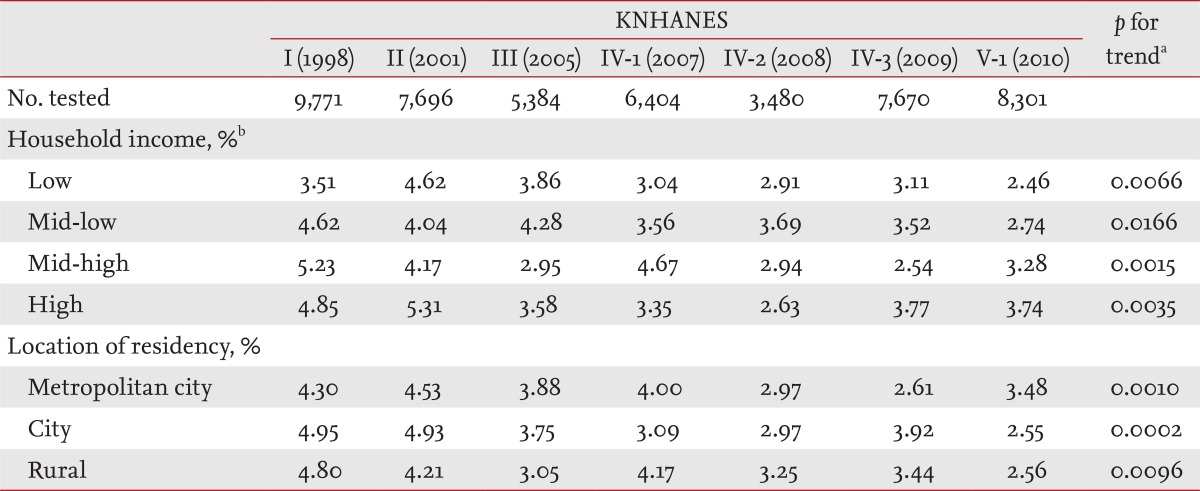
KNHANES is a cross-sectional national representative health and nutrition examination survey, conducted by the Korea Centers for Disease Control and Prevention. The survey uses a complex, stratified, multistage probability sample of the Korean population. The procedures for selecting the sample group and conducting the interviews and examinations have been specified elsewhere (The Korean Association for Survey Research). The sample was selected in 11 metropolitan cities and provinces (seven metropolitan cities, Gyeonggi-do, Gangwon-do/Gyeongsang-do, Chungcheong-do, Jeolla-do/Jeju-do) of Korea and systematic sampling was done to reflect characteristic of the population by region [8]. Trained research staff conducted a health interview, health consciousness and behavior survey, nutritional survey, and medical examination. The KNHANES database includes 50,140 serum samples that were analyzed from 1998 to 2010 (Table 1).
Laboratory evaluation
Serum samples were collected from subjects aged at least 10 years who completed the examination component of the KNHANES. HBsAg tests were performed using enzyme-linked immunosorbent assays (ELISA) in 1998 and 2003 (CODA, Bio-Rad, Hercules, CA, USA). Electrochemiluminescence immunoassays (ECLIA) were conducted from 2005 to 2010 (E170, Roche Diagnostics, Basel, Switzerland). HBsAg titers greater than 1 IU/mL were considered positive for HBV infection.
Data analysis and statistical methods
All sampling and weight variables were stratified. The SUDAAN (Research Triangle Institute, Research Triangle Park, NC, USA) procedure was used for statistical analyses. To assess means, standard errors, and percentages, we used stratification variables and sampling weights designated by the Korean Center for Disease Control and Prevention, based on the sample design of each survey year. The sampling weights were adjusted for nonresponses according to demographic factors after survey completion. The SAS Survey procedure was performed using clusters as a sampling-district variable. The chi-squared test was used to compare proportional differences among the 7 survey years. The Cochran-Mantel-Haenszel trend test was used to examine the linear effects of proportion among the 7 survey years. All statistical analyses were conducted using the SUDAAN software version 10.0. Reported p values were two-tailed, and p values < 0.05 were considered to indicate statistical significance.
RESULTS
Changes in prevalence of HBsAg carriers in Korean population
Table 1 presents the baseline clinical characteristics of the 50,140 participants. Overall HBsAg seropositivity was 4.61% (95% confidence interval [CI], 4.06% to 5.16%) in 1998, 4.60% (95% CI, 3.96% to 5.24%) in 2001, 3.69% (95% CI, 3.07% to 4.30%) in 2005, 3.72% (95% CI, 2.88% to 4.56%) in 2007, 3.01% (95% CI, 2.59% to 3.44%) in 2008, 3.23% (95% CI, 2.67% to 3.78%) in 2009, and 2.98% (95% CI, 2.48% to 3.48%) in 2010. The prevalence of HBsAg carriers decreased over the study period (p < 0.0001, Cochran-Mantel-Haenszel trend test) (Fig. 1). HBsAg carriers decreased across all surveys among both men and women (Table 1).
Changes in HBsAg seropositivity according to age group
The HBsAg-positive population markedly declined in younger age groups over the study period (1998 to 2010) (Fig. 2). Among teenagers (10 to 19 years), prevalence decreased, from 2.2% in 1998 to 0.12% in 2010 (p < 0.0001) (Table 2). Among subjects aged 20 to 39 years, the prevalence of HBsAg carriers decreased significantly (5.48% to 2.34% in 20s and 6.15% to 3.85% in 30s; p < 0.0001 and p = 0.0002, respectively). Among subjects aged 40 to 49 years, the presence of HBsAg carriers also decreased (5.43% in 1998 and 3.71% in 2010; p = 0.0233). However, among subjects aged 50 years or older, HBsAg seropositivity did not decrease throughout the study period (Table 2).

Changes in hepatitis B surface antigen (HBsAg) seropositivity in age groups. p value by Cochran-Mantel-Haenszel trend test.
KNHANES, Korea National Health and Nutrition Examination Survey.
Changes in HBsAg seropositivity according to socioeconomic status
Table 3 summarizes the prevalence of HBsAg carriers according to household income and location of residency. Household income is classified into four subgroups. Each subgroup was calculated by income quartile to measure the average household income of residents, ranking them from poorest to wealthiest, and then grouping them into four income quartiles (low, mid-low, mid-high, and high), each quartile containing approximately 25% of the population [8]. A decrease in the prevalence of HBsAg carriers was observed in all household income level subgroups. A similar pattern was observed in all studied locations (metropolitan, city, and rural area). Thus, household income and location did not affect HBV prevalence in the Korean population.
DISCUSSION
The population-based national survey (KNHANES) revealed a decreased prevalence of HBV infection in the general Korean population over the last decade. The decrease in HBsAg carriers was more prominent in the younger population. Universal vaccination programs have contributed to the marked decline of HBV infection in subjects younger than 20 years (2.2% to 0.12%). A similar decline in HBV infection rates was reported in Taiwan following its newborn vaccination program [9]. HBV vaccinations of newborns prevented the majority of perinatal transmission and reduced horizontal transmission to children born up to 6 years prior to the initiation of the program. In 1995, the Korean National Immunization Program for all neonates began to include universal vaccination for HBsAg, regardless of maternal HBsAg status. Since July 2002, newborns of HBsAg-positive mothers have been vaccinated as part of the hepatitis B prenatal transmission prevention program. HBV vaccine and hepatitis B immune globulin are simultaneously administered at two sites within 12 hours of delivery. The vaccination rate exceeds 90% of subjects and the prevention rate of vertical transmission is 90% to 95% [10,11].
This extensive and national effort reduced vertical and horizontal transmission of HBV within the population. In the present study, we observed positive effects of the HBV vaccine, particularly in younger age groups.
The prevalence of HBsAg carriers also declined among those aged 30 to 39 years. The prevalence of HBsAg carriers decreased, from 6.15% to 3.85%, among those aged 30 years (p = 0.0002) and from 5.43% to 3.71% among those aged 40 years (p = 0.0233). The causes of these declines in HBV rates are unclear. Socioeconomic status, including household income or location, did not significantly affect the rates of HBV decline. HBV vaccination likely played a role, but the universal neonatal HBV vaccination was not available to these specific age groups (30 to 49 years), and many of these individuals were vaccinated during childhood and adolescence. The Korean government has conducted a mass catch up vaccination campaign since 1988, when school-aged children and adolescents were vaccinated [12]. HBV vaccines have been available commercially since 1983 [13], so private HBV vaccinations and herbal immunity may have contributed to the decline in HBV rates. The use of disposable syringes and razors and increased awareness about proper hygiene may also have contributed to decreasing HBV infection rates.
Unsurprisingly, the prevalence of HBsAg positivity has remained unchanged in middle-aged and elderly populations. Although HBsAg-positive rates tend to decrease with aging, due to a natural loss of HBsAg [14], the overall trends in HBV infection were unaffected. This suggests that the risk for HBV-related cirrhosis or HCC in the elderly population may not decrease for some time. Recent national cancer statistics have confirmed that the incidence of HCC in Korea has not declined in the elderly population: 13,126 in 2000 and 15,936 in 2009 [15]. In contrast, HCC rates among children who received HBV vaccinations declined rapidly [16].
Screening programs to detect HBV infection in the general adult population should therefore be maintained. Screening, defining high-risk subjects, and providing optimal antiviral treatment are also important to reduce mortality and morbidity from chronic HBV infection.
This study had some limitations. First, bias from the self-reported questionnaire cannot be excluded. Second, HBsAg detection methods differed between KNHANES I, II, III, IV, and V. An automated enzyme immunoassay (ELISA; Bio-Rad Elite microplate) was used in surveys I and II, whereas an ECLIA was used in later tests. Enzyme immunoassays are reliable and easy to perform for mass screening programs, and display a high level of performance [17,18]. The ECLIA is an additional highly sensitive and specific screening assay for HBsAg, including HBV mutants [19], and is widely used in HBsAg screening. The sensitivity of ELISA and ECLIA testing is over 99% [20] and the concordance rate between the two methods is reportedly as high as 97% [21]. Although the methods used in KNHANES have not been compared directly, differences in HBsAg sensitivity are likely to be minimal.
In summary, HBV infection rates have decreased since the adoption of HBV vaccination programs in Korea. The dramatic reduction of HBV infection is more prevalent in the younger population. Among subjects aged 30 to 49 years, HBV infection decreased over the 12-year study period, while the overall prevalence of HBsAg carriers remains around 4%. Additionally, HBV infection remains prevalent in the older Korean population (≥ 50 years). Thus, the detection of HBV infection, optimal antiviral treatment, and cost-effective surveillance strategies are still required for the middle-aged and elderly Koreans where HBV prevalence remains high.
KEY MESSAGE
1. Hepatitis B virus (HBV) infection has decresed in the Korean population since the advent of vaccination programs.
2. In our study, the decrease is limited to the younger population, and viral persistence remained in the middle-aged and older population.
3. Therefore, effective surveillance strategies to detect HBV infection in the general adult population are still required for the middle-aged and older population.
Notes
No potential conflict of interest relevant to this article is reported.