Different Impact of Diabetes Mellitus on In-Hospital and 1-Year Mortality in Patients with Acute Myocardial Infarction Who Underwent Successful Percutaneous Coronary Intervention: Results from the Korean Acute Myocardial Infarction Registry
Article information
Abstract
Background/Aims
The aim of this study was to evaluate the impact of diabetes mellitus (DM) on in-hospital and 1-year mortality in patients who suffered acute myocardial infarction (AMI) and underwent successful percutaneous coronary intervention (PCI).
Methods
Among 5,074 consecutive patients from the Korea AMI Registry with successful revascularization between November 2005 and June 2007, 1,412 patients had a history of DM.
Results
The DM group had a higher mean age prevalence of history of hypertension, dyslipidemia, ischemic heart disease, high Killip class, and diagnoses as non-ST elevation MI than the non-DM group. Left ventricular ejection fraction (LVEF) and creatinine clearance were lower in the DM group, which also had a significantly higher incidence of in-hospital and 1-year mortality of hospital survivors (4.6% vs. 2.8%, p = 0.002; 5.0% vs. 2.5%, p < 0.001). A multivariate analysis revealed that independent predictors of in-hospital mortality were Killip class IV or III at admission, use of angiotensin converting enzyme inhibitors or angiotensin-II receptor blockers, LVEF, creatinine clearance, and a diagnosis of ST-elevated MI but not DM. However, a multivariate Cox regression analysis showed that DM was an independent predictor of 1-year mortality (hazard ratio, 1.504; 95% confidence interval, 1.032 to 2.191).
Conclusions
DM has a higher association with 1-year mortality than in-hospital mortality in patients with AMI who underwent successful PCI. Therefore, even when patients with AMI and DM undergo successful PCI, they may require further intensive treatment and continuous attention.
INTRODUCTION
Acute myocardial infarction (AMI) remains a leading cause of morbidity and mortality worldwide. However, mortality from MI has decreased over the years due to improvements in percutaneous coronary intervention (PCI) techniques and the development of stents, new life-saving devices, and medications. Nevertheless, many clinical risk factors affect high mortality in patients with AMI.
Diabetes mellitus (DM) is well-known as a coronary artery equivalent disease and a major cardiovascular risk factor [1]. Patients with DM have a higher rate of AMI and a greater need for repeated revascularization after PCI [2,3]. After suffering from AMI, short- and long-term mortality rates are twice as high for patients with DM as those without DM [4,5]. However, in the recently improved interventional era of drug-eluting stents, few large-scale studies have been reported about the impact of DM on clinical outcomes, particularly in patients with AMI who underwent successful PCI.
In the present study, we compared in-hospital and 1-year mortality in diabetic and non-diabetic patients with AMI who underwent successful PCI using data from the Korean Acute Myocardial Infarction Registry (KAMIR).
METHODS
Study design and patient population
We consecutively selected 5,074 patients with AMI who underwent successful PCI from November 2005 to June 2007 and had 1-year follow-up data in the KAMIR. Among them, patients with a history of DM, regardless of whether they received treatment, were assigned to the DM group (n = 1,412) and those without a history of DM were assigned to the non-DM group (n = 3,662).
The KAMIR is a prospective, multicenter, observational, online registry that can be used to evaluate epidemiology, current management, and clinical outcomes in Korean patients with AMI and improve care for AMI patients. Data, including baseline clinical and angiographic characteristics as well as clinical outcomes, were collected by a specialized study coordinator at each center using a standardized case report form. AMI was diagnosed by characteristic clinical presentation, serial changes on electrocardiogram (ECG) suggesting infarction, and increases in cardiac enzymes [6]. The diagnosis of ST-segment elevated myocardial infarction (STEMI) was based on a suggestive history with an ST elevation of 2 mm in two precordial leads, an ST elevation of 1 mm in two limb leads, or a new left branch bundle block on 12-lead ECG with a concomitant increase in troponin-I or -T to the 99th percentile of the upper reference limit.
Procedural and post-intervention medications
Emergent or early invasive treatments were determined based on the status of the patients with AMI according to the clinical decision of the operators. Primary PCI was defined as angioplasty and/or stenting as quickly as possible in patients with STEMI. Early invasive treatment was defined as angioplasty and/or stenting within 24 hours of admission in patients with non-STEMI. Coronary angiography was performed by transfemoral or transradial approaches. Conventional heparin was infused during the procedure to maintain an activated clotting time of at least 250 seconds. Stents were implanted in cases in which significant coronary artery stenosis was present following balloon angioplasty. The type of stent was decided by the operator. Successful revascularization was defined as a target vessel at the treatment site that had achieved angiographic residual stenosis of < 30% following balloon angioplasty or implantation of stents in the presence of thrombolysis in myocardial infarction (TIMI) antegrade 3 flow. Antiplatelet agents were administered to all patients prior to intervention, including 300 mg aspirin and 300-600 mg clopidogrel. After the intervention, 100 mg aspirin was recommended as a treatment for life and 75 mg clopidogrel was administered for at least 1 year. Other medical treatments, including angiotensin converting enzyme inhibitors (ACEis) or angiotensin II receptor blockers (ARBs), beta-blockers, calcium channel blockers, and lipid-lowering agents were also used based on the standard treatment regimen for patients with AMI according to the physician's decision.
Study endpoints and definition
The primary endpoint was in-hospital and 1-year mortality of patients with AMI with and without DM. The secondary endpoint was 1-year major adverse cardiac events (MACE) defined as the composite of cardiac death, nonfatal MI, target lesion revascularization (TLR), target vessel revascularization (TVR), and coronary artery bypass graft. Cardiac death was defined as any death with an undetermined cause and a definitive noncardiac origin. TLR or TVR was defined as any percutaneous coronary revascularization performed on a treated lesion or vessel. Hypertension was defined as a history of hypertension or antihypertensive medication use. A current smoker was defined as someone who reported smoking cigarettes during the past 30 days. Dyslipidemia was defined as a diagnosis previously made by a physician or treatment with lipid-lowering medications. Baseline creatinine clearance was calculated using the Cockcroft-Gault formula considering age, gender, and body weight.
Statistical analysis
Continuous variables are expressed as mean ± SD, and categorical variables are expressed as frequencies. The analysis of continuous variables was performed using Student's t test and that of categorical variables was performed using the chi-square or Fisher's exact tests. Multiple logistic regression and Cox proportional regression analyses were conducted to identify the independent predictors of in-hospital and 1-year mortality. Variables entered into the multivariate models were age, gender, creatinine clearance, history of hypertension, DM, dyslipidemia, ischemic heart disease, current smoker, left ventricular ejection fraction (LVEF), ACC/AHA B2 or C lesions, Killip class on admission, multivessel disease, STEMI or non-STEMI, concomitant medications, and stent type. All statistical analyses were performed using SPSS version 15.0 (SPSS Inc., Chicago, IL, USA). All statistical tests were two-tailed, and a p value < 0.05 was considered statistically significant.
RESULTS
Baseline characteristics
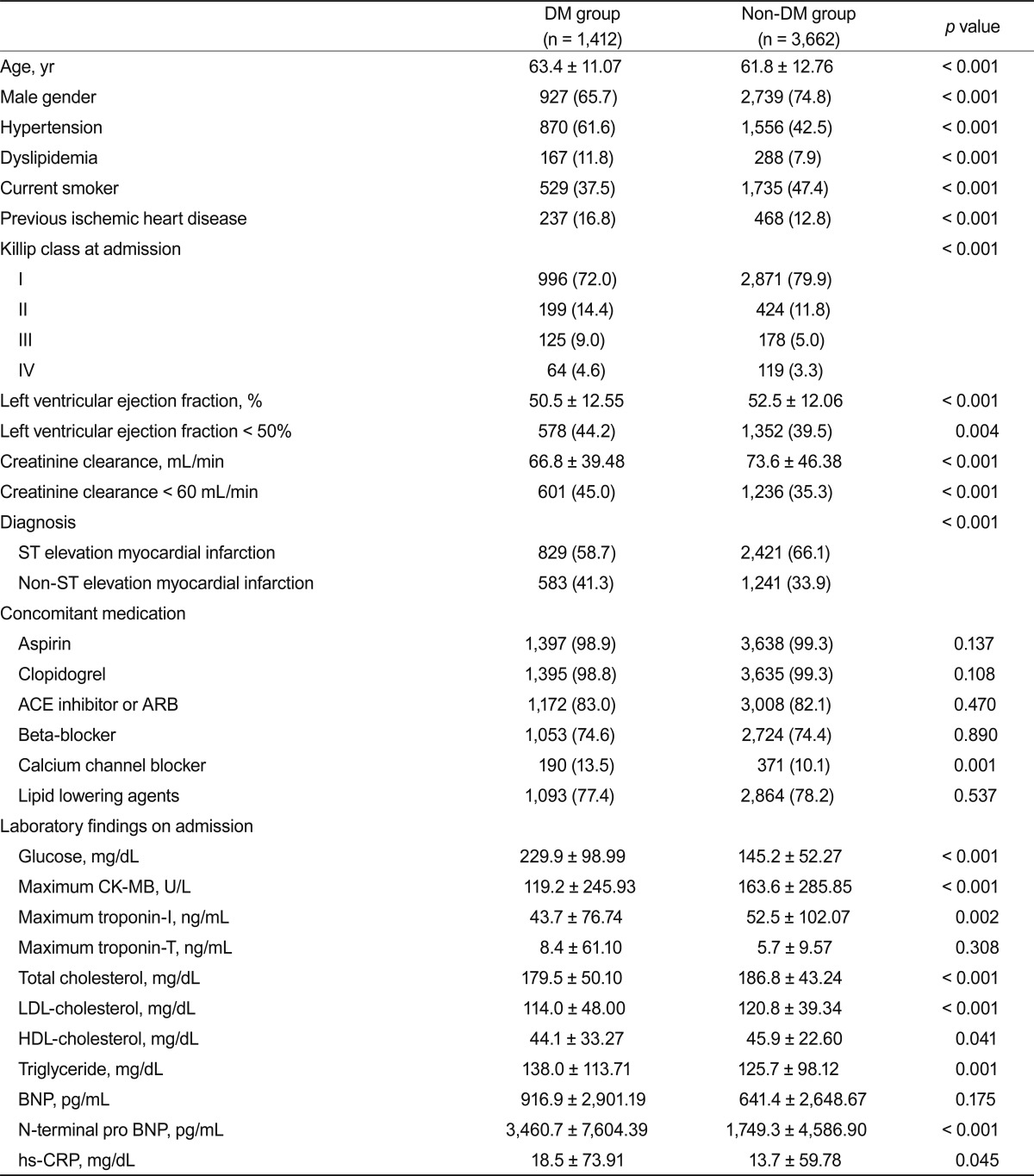
Mean age was higher in the DM group than in the non-DM group. Female gender, history of hypertension, dyslipidemia, previous ischemic heart disease, and diagnosis of non-STEMI were more prevalent in the DM group. However, male gender, current smoker, and diagnosis of STEMI were more prevalent in the non-DM group. LVEF and creatinine clearance were lower in the DM group. However, no differences in concomitant medications except calcium channel blockers were observed between the two groups. Table 1 shows the baseline clinical characteristics, concomitant medications, and laboratory findings of the two groups.
In the baseline angiographic and procedural characteristics, single-vessel disease was more prevalent in the non-DM group than in the DM group. However, three-vessel disease or left main coronary artery disease were more prevalent in the DM group, whereas preprocedural TIMI antegrade 0 flow rates were more common in the non-DM group and postprocedural TIMI antegrade flow rates did not differ between the two groups. TAXUS stents (Boston Scientific Co., Natick, MA, USA) were used more commonly in the non-DM group, whereas Cypher stents (Cordis, Johnson & Johnson, Miami Lakes, FL, USA) were used more commonly in the DM group. The stent diameter of the target lesion was smaller, and the total number of implanted stents was more numerous, in the DM group than in the non-DM group (Table 2).
Clinical outcomes
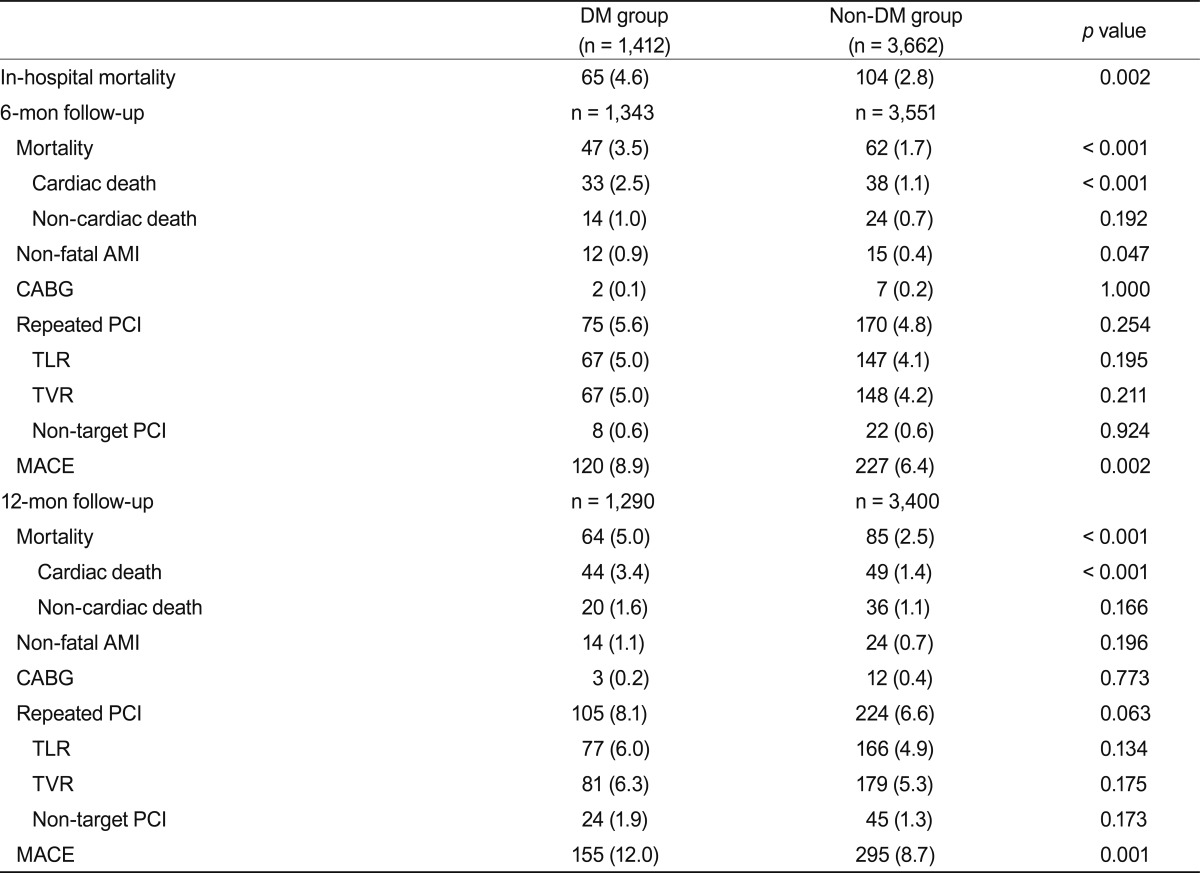
The DM group had a significantly higher incidence of in-hospital mortality than the non-DM group (4.6% vs. 2.8%, p = 0.002).
Approximately 92% of all hospital survivors were available for the 1-year clinical follow-up, during which the DM group had significantly higher incidences of total mortality (5.0% vs. 2.5%, p < 0.001), cardiac death (3.4% vs. 1.4%, p < 0.001), and MACE (12.0% vs. 8.7%, p = 0.001) than did the non-DM group (Table 3).
Subgroup analyses showed that the incidence of in-hospital mortality in the DM group was significantly higher than in non-DM patients with STEMI (6.2% vs. 3.5%, p = 0.001), but no difference in in-hospital mortality was observed between the two groups in patients with non-STEMI (2.4% vs. 1.6%, p = 0.164). However, the incidence of 1-year mortality in the DM group was higher than that of non-DM patients with both STEMI and non-STEMI (4.6% vs. 2.7%, p = 0.010 in STEMI; 5.5% vs. 2.1%, p < 0.001 in non-STEMI).
A Kaplan-Meier survival analysis revealed that the DM group had significantly lower 1-year survival rates than the non-DM group (95.2% vs. 97.7%, p < 0.001) (Fig. 1).
Multivariate analyses
The independent predictors of in-hospital mortality by multiple logistic regression analysis were Killip III or IV class on admission, use of ACEis or ARBs, LVEF, creatinine clearance, and STEMI, whereas DM was not an independent predictor of in-hospital mortality (hazard ratio, 1.386; 95% confidence interval, 0.810 to 2.374; p = 0.234). However, independent predictors of 1-year mortality included Killip class on admission, age, LVEF, creatinine clearance, balloon angioplasty, use of bare metal stents, multivessel disease, female gender, current smoker, and history of DM (Table 4).
DISCUSSION
We evaluated the impact of DM on in-hospital and 1-year mortality in patients with AMI who underwent successful revascularization, and the results suggest that despite successful revascularization, the incidence of in-hospital and 1-year mortality in patients with AMI and DM remained high. However, DM was not an independent predictor of in-hospital mortality, whereas DM was a predictor of 1-year mortality in the multivariate analyses.
In our cohort, patients with DM had worse baseline clinical characteristics than those without DM. In addition, they were more likely to have developed a worsening of Killip class at admission and a higher incidence of pump failure, because increased incidence of silent myocardial ischemia and infarction in patients with DM tends to lead to late presentation for medical attention and subsequent delayed initiation of treatment [7]. Several studies have found that patients with AMI and DM have a higher incidence of in-hospital mortality than those without DM [8-12]. However, almost all of these studies included patients who received only pharmacological treatment for AMI. Successful revascularization via a catheter-based approach minimizes ischemic injury of the myocardium and improves survival rates. Therefore, we included patients with AMI who underwent successful revascularization and excluded patients with AMI who received only medical treatment or thrombolytic therapy without mechanical revascularization.
Our results showed that despite successful revascularization in patients with AMI, patients with DM still had a higher incidence of in-hospital mortality than those without DM. Other trials have reported that a significant delay from symptom onset to hospital arrival in patients with DM results in a significant delay in reperfusion treatment [7,13,14]. The presenting symptoms of patients with DM may also be more difficult to relate to active ischemic heart disease and may be associated with a delay in the AMI diagnosis. Delayed treatments were associated with poor clinical outcomes during the hospital stay.
Patients with DM have increased platelet aggregatory and procoagulant activity, leading to an inherently greater incidence and rate of thrombus formation [13,15]. However, our results showed that patients with DM had a lower incidence of pre-procedural TIMI antegrade 0 or 1 flow than those without DM. This finding may be based on patient selection bias, because we included patients who underwent successful revascularization. However, despite better preprocedural TIMI flow, patients with DM had poorer in-hospital outcomes. This is also evidence of the negative impact of DM on AMI.
DM was not an independent predictor of in-hospital mortality, which has been reported in other trials [8,9,12]. Independent predictors of in-hospital mortality were high Killip class on admission, use of ACE is or ARBs, depressed LVEF, decreased renal function, and STEMI. Successful PCI could probably improve in-hospital survival rates and influence the predictors of in-hospital mortality. Therefore, in-hospital mortality was more likely to be associated with patient clinical status and medical treatment strategy than a history of DM in patients with AMI who underwent successful PCI.
DM is a well-known metabolic abnormality of hyperglycemia and insulin resistance, and a variety of mechanisms, including endothelial dysfunction, abnormal platelet function, and coagulation abnormalities, are responsible for accelerated atherosclerosis and excessive neointimal formation after coronary intervention [16-18]. DM is associated with an increased risk of death, stent thrombosis, and restenosis after PCI [19-21]. Our results showed that DM was an independent predictor of 1-year mortality in patients with AMI. Although patients received successful revascularization and improved management, patients with DM still had high 1-year mortality rates. Patients with DM had more depressed left ventricular systolic function, decreased renal function, and an increased prevalence of three-vessel disease or left main coronary artery disease. Therefore, patients with DM tended to receive incomplete revascularization. These poor clinical conditions and incomplete revascularization could also affect the high incidence of 1-year mortality and MACE in patients with DM [22]. Our results showed that repeated PCI tended to be more frequent in patients with DM during the 1-year follow-up period. The major stimulus for increased intimal hyperplasia in patients with DM may be hyperinsulinemia, as supported by the findings of several studies [23-26]. Therefore, even though patients with AMI and DM underwent successful PCI, they required further intensive treatment and continuous attention.
The rates of in-hospital mortality and 1-year mortality were 4.6% and 5.0% in the patients with AMI and DM after successful revascularization. Even if a direct comparison is impossible, these rates are relatively low compared to those of previous studies [8,11,12,27,28]. While patients with DM still have high mortality rates, successful PCI and appropriate medical treatment should help to improve their clinical outcomes.
Study limitations
Many limitations of our study should be noted. First, this was a multicenter prospective observational registry study and not a randomized controlled trial. Second, we only included patients with AMI who underwent successful revascularization and excluded those who received medical treatment including thrombolytic therapy. Therefore, we could not evaluate the impact of DM in patients with AMI. Third, because a follow-up coronary angiography was performed in only approximately 43% of all patients, we may have underestimated the incidence of repeated PCI and MACE.
In conclusions, DM was more highly associated with 1-year mortality than in-hospital mortality in patients with AMI who underwent successful PCI. This suggests that patients with AMI and DM who undergo successful PCI may require further intensive treatment and continuous attention.
Acknowledgments
KAMIR investigators; this work was supported by a grant from the National Research Foundation of Korea funded by the Korean Government (MEST), Republic of Korea (2010-0020261), and by a grant from the Korea Healthcare Technology R&D Project, Ministry for Health, Welfare, and Family Affairs, Republic of Korea (A084869).
Notes
No potential conflict of interest relevant to this article was reported.