Efficacy and Safety of Hepatic Arterial Infusion of Fluorouracil with Leucovorin as Salvage Treatment for Refractory Liver Metastases from Colorectal Cancer
Article information
Abstract
Background/Aims
Limited options remain for patients with metastatic colorectal cancer (CRC) after failure of standard systemic chemotherapy. Readministration of chemotherapeutic agents by hepatic arterial infusion (HAI) has the rationale of providing higher concentrations of chemotherapeutic agents to hepatic metastases. The present study was conducted to evaluate the efficacy and safety of HAI of fluorouracil with leucovorin (HAI 5-FU/LV) for patients with liver metastases from CRC.
Methods
Fourteen patients with liver metastases from CRC who received HAI 5-FU/LV after failure of systemic chemotherapy containing fluorouracil and leucovorin were identified and their medical records were reviewed.
Results
Of 10 patients evaluable for response, one partial response, six stable disease, and three progressive disease were reported. Additionally, the overall response and disease control rates were 7% and 50%, respectively. The median time to progression was 4.3 months (range, 2.9 to 5.6), to hepatic progression was 5.8 months (range, 4.7 to 6.9), and to extrahepatic progression was 5.8 months (range, 2.3 to 9.2). No grade 3/4 hematologic toxicities occurred and one case of abdominal pain and two cases of oral mucositis were the only grade 3 nonhematologic toxicities. Catheter-related complications occurred in three patients: one thrombosis, one infection, and one displacement.
Conclusions
HAI 5-FU/LV was well tolerated and showed modest efficacy for patients with liver metastases from refractory CRC. Readministration of previously used chemotherapeutic agents via the hepatic artery could be an effective salvage option and warrants further investigation in a prospective trial.
INTRODUCTION
Nearly 50% of colorectal cancer (CRC) patients will develop liver metastases at some point during their disease and it is the progression of the liver lesion that determines the overall life expectancy for patients with liver metastases [1]. Surgical resection of liver metastases from CRC is the only treatment modality with curative potential and results in a 5-year overall survival (OS) rate of 20-40% [2]. However, only 20% of patients with liver metastases, depending on their comorbidities, have resectable disease at diagnosis and are candidates for major surgery [3]. Therapeutic strategies for unresectable liver metastases consist of chemotherapy plus biologics such as bevacizumab or cetuximab, and then subsequent liver resection for those patients who are converted to resectable disease. Even in the era of targeted agents such as cetuximab [4,5] and bevacizumab [6], the hepatic resection rate rarely exceeds 30-40%. Moreover, many patients cannot receive targeted agents because of economic issues or adverse events. This provides the impetus to develop regimens that are more effective for patients with unresectable liver metastases.
The liver has a dual blood supply system, the portal vein to the healthy liver parenchyma and the hepatic artery to the liver metastatic lesion [7]. Most cancer cells derive their blood supply from hepatic arteries. This unique differential blood supply of the liver provides the rationale for locoregional treatment such as hepatic arterial infusion (HAI) chemotherapy. For patients with unresectable liver metastases from CRC, HAI provides higher concentrations of chemotherapeutic agents in the hepatic artery. HAI has been developed and tested over the past two decades. It has been reported to produce a higher response rate with better control of liver disease than conventional chemotherapy but, for many reasons, has had minimal impact on survival. HAI has no benefit for extrahepatic disease and has its own toxicity profile, including biliary sclerosis, acalculous cholecystitis, and catheter-related problems. Many of these results come from studies with HAI of fluorodeoxyuridine (HAI FUDR) using a hepatic arterial catheter placed during laparotomy [8]. FUDR is ideal for HAI because of its short half-life and high liver extraction rate (> 90%), leading to a 100- to 400-fold ratio of hepatic-to-systemic drug exposure and a response rate exceeding 50%, even without combination with newer agents. However, HAI FUDR has limitations, including biliary sclerosis, which is a dose-limiting toxicity [9], and a disappointing control rate for extrahepatic disease [10]. HAI of fluorouracil with leucovorin (HAI 5-FU/LV) demonstrated a response rate that was similar to, or higher than, that obtained with HAI FUDR without the associated hepatic toxicities and with a reduction in extrahepatic disease. A high local response rate, combined with a significant reduction of extrahepatic disease, may explain the superiority of HAI 5-FU/LV in prolonging time to progression [11].
Because of the advantage of HAI for delivering higher doses of anticancer agents directly into the affected organ, HAI using previously administered systemic chemotherapeutic agents could be another treatment option for patients with refractory CRC with metastases confined to the liver. To test this hypothesis, the present study was conducted to evaluate the efficacy and safety of HAI 5-FU/LV in patients with liver metastases from CRC who were previously treated with systemic 5-FU-based chemotherapy.
METHODS
Patients
All patients with liver metastases from CRC who received HAI 5-FU/LV after failure of systemic 5-FU-based chemotherapy between July 2004 and December 2009 were retrospectively enrolled in the present study. Patients were identified from the prospectively maintained cancer registry from Seoul National University Bundang Hospital electronic medical records. Data, including patient and tumor characteristics, laboratory values, treatment outcomes, and toxicity were collected and analyzed retrospectively from patients' medical records.
Implantation of port system
After injection of a local anesthetic, the Seldinger technique was used to gain access to the right femoral artery. Arteriography of the celiac trunk was performed to reveal the hepatic arterial anatomy. The gastroduodenal artery and the right gastric artery were embolized using steel coils (Tornade, Cook, Bloomington, IL, USA) to prevent gastroduodenal injury from the chemotherapeutic agents. In patients with multiple hepatic arteries, all the hepatic arteries except the largest one were embolized to redistribute the hepatic arterial flow so that a single indwelling catheter could be used to infuse chemotherapeutic agents to the entire liver. To avoid mechanical injury to the artery by the infusion catheter, the "tip-fixation" technique was used [12].
A 5F catheter (Port-A-Cath, Deltec, St. Paul, MN, USA) with a side hole was inserted with the distal tip into the gastroduodenal artery. The position of the side hole was sited at the common hepatic artery, and then the distal tip of the catheter was fixed within the gastroduodenal artery using coils. The proximal end of the catheter was connected to the injection port and the device was implanted in a subcutaneous pocket in the right inner thigh. To prevent occlusion of the catheter, 10 mL (10,000 U) of heparin solution was infused via the injection port after each cycle of chemotherapy.
Chemotherapy administration
The 5-FU/LV treatment protocol consisted of hepatic arterial administration using the infusion pump of 800 mg/m2 5-FU infused over 24 hours on day 1-5 combined with 200 mg/m2 leucovorin on day 1-5. Treatment courses were repeated every 4 weeks. Treatment was continued until disease progression, toxicity prevented pursuit of treatment, or patient refusal of treatment.
Efficacy and toxicity evaluation
Tumor size was measured using computed tomography scans after every 2 or 3 cycles of treatment. The response was assessed by medical oncologists at the time of treatment according to the Response Evaluation Criteria in Solid Tumors 1.0 [13] and was reviewed by an independent radiologist blinded to the clinical outcome at the time of retrospective review. Time to progression (TTP), time to hepatic progression (THP), and time to extrahepatic progression (TEP) were calculated from the time of the first HAI 5-FU/LV infusion. TTP was defined as progression of disease at any site or death from any cause, THP was defined as progression of disease in the liver, and TEP was defined as progression outside the liver. Adverse events were graded according to the Common Terminology Criteria for Adverse Events (CTCAE ver. 3.0) before each course of chemotherapy.
Statistical analysis
All time-related parameters were analyzed using the Kaplan-Meier method. Data were expressed as means or medians with ranges. All data parameters were compiled using SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). The present study was approved by the institutional review board of Seoul National University Bundang Hospital (IRB approval No. B-1003/095-103).
RESULTS
Patient characteristics
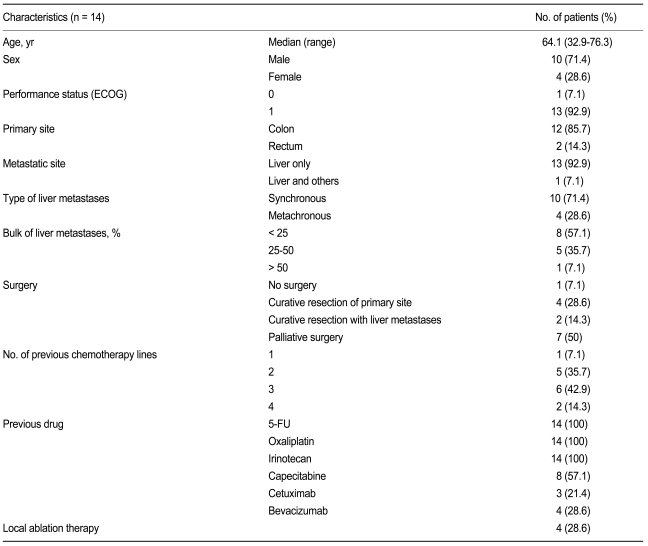
Fourteen patients with liver metastases received HAI 5-FU/LV after failure of systemic chemotherapy. The median duration of follow-up was 8.4 months (range, 4.2 to 20). The median age of all patients was 64.1 years (range, 32.9 to 76.3) and the mean number of previously administered systemic chemotherapies was 2.6 (range, 1 to 4). The patients' characteristics are listed in Table 1.
Thirteen patients had only hepatic metastases and one patient had both hepatic and extrahepatic metastases. The extrahepatic metastatic site was the lung. Two patients underwent a hepatic metastasectomy, and four patients underwent radiofrequency ablation (RFA) before receiving HAI 5-FU/LV. Most of the patients had been previously heavily treated. All 14 patients had previously received chemotherapy containing 5-FU, oxaliplatin, and irinotecan.
Efficacy
The mean number of treatment cycles was 4.1 (range, 1 to 7). Reasons for treatment discontinuation were disease progression in 10 patients, patient refusal in two, severe abdominal pain in one and catheter thrombosis in one. The patient with severe abdominal pain could not complete the first cycle and was therefore excluded from the response evaluation. Two of four patients who had undergone RFA showed no measurable lesion and the other had a small lesion less than 10 mm. One patient had a partial response, six had stable disease, and three had progressive disease. The overall response rate (RR) was 7% and the disease control rate was 50%. Seven of the 13 patients who had progression of their disease had progression of extrahepatic disease while their hepatic disease was stable. Two patients with stable disease had progression of their disease during the chemo-off period. No patient in the present study underwent hepatic resection after HAI 5-FU/LV.
The median OS was 10.7 months (range, 8.5 to 12.8) and the median TTP was 4.3 months (range, 2.9 to 5.6). The median THP was 5.8 months (range, 4.7 to 6.9) and the median TEP was 5.8 months (range, 2.3 to 9.2). Fig. 1 illustrate the TTP, THP, and TEP. Among the seven patients who experienced earlier progression of extrahepatic disease as opposed to hepatic disease, five presented with de novo extrahepatic metastases, one who had an initial lung metastasis experienced progression of that lung metastasis, and one showed local recurrence. Nine of the 14 patients underwent additional systemic chemotherapy after their disease progression. Among the seven patients with earlier extrahepatic progression, four received salvage chemotherapy, two received palliative care, and one patient was lost to follow-up. Five of six patients who experienced earlier hepatic disease progression underwent salvage chemotherapy and the other received palliative care.

(A) Time to progression in patients who received HAI 5-FU/LV. (B) Time to hepatic progression and extrahepatic progression in patients who received HAI 5-FU/LV. HAI 5-FU/LV, hepatic arterial infusion of fluorouracil with leucovorin; THP, time to hepatic progression; TEP, time to extrahepatic progression.
Capecitabine, S-1, oxaliplatin, irinotecan, oratecan, cetuximab, and bevacizumab were used in salvage therapy as single agents or in combination. One patient received oral S-1 plus HAI oxaliplatin but progressed. Five of the 14 patients did not undergo further systemic chemotherapy because of their poor performance status or refusal to receive further treatment.
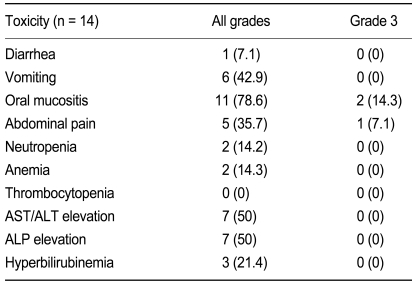
Toxicity
No treatment-related deaths were reported. The most frequent nonhematologic toxicity was oral mucositis, which occurred in 11 patients, with grade 3 oral mucositis in two patients. Hematologic toxicity of any grade was mild and no episode of febrile neutropenia was reported. No biliary sclerosis or cholangitis was observed (Table 2).
Three catheter-related complications were reported. One patient had catheter thrombosis and another had catheter displacement that led to removal of the hepatic arterial catheter and discontinuation of HAI. The other patient had a catheter-related infection, which was treated with antibiotics, and continued HAI 5-FU/LV.
The median dose intensity of infused 5-FU was 915.0 mg/m2/wk (range, 682.2 to 1098.0) and the relative dose intensity was 91.5%. Five patients had the same daily dose of HAI 5-FU/LV for 4 instead of 5 days, which led to the reduction of the dose to 80% of that planned.
DISCUSSION
In our study, HAI 5-FU/LV in heavily treated patients with unresectable liver metastases from CRC demonstrated moderate efficacy and toxicity. Although all patients had failed previous systemic chemotherapy containing 5-FU, oxaliplatin, and irinotecan, they showed a TTP of 4.3 months and a disease control rate of 50%. These findings are similar to those of other second-line systemic chemotherapies. Prospective randomized phase III trials of first-line modern chemotherapy FOLFOX [14] and FOLFIRI [15] before the era of targeted therapy reported response rates of 50-56% and complete resection rates of 4-21%. Response rates to second-line chemotherapy were even lower [15]. Second-line FOLFIRI and FOLFOX-6 achieved response rates of 4% and 15% and progression-free survivals of 2.5 and 4.2 months, respectively. Our results suggest that HAI 5-FU/LV might be effective in increasing the TTP in patients who experienced failure of previous systemic 5-FU by delivering a higher concentration of drug directly to metastatic lesions. This hypothesis could be expanded to HAI with other active agents such as oxaliplatin and irinotecan after systemic failure of the same agents. HAI of oxaliplatin or irinotecan has demonstrated efficacy and feasibility as a salvage treatment modality. HAI of irinotecan, 5-FU, and oxaliplatin in previously treated patients resulted in a 33% objective response rate and a median progression-free survival (PFS) of 6 months [16]. HAI of oxaliplatin with systemic infusion of 5-FU/LV in pretreated patients reported an objective response rate of 55% and a median PFS of 7 months [17].
The present study showed that the response rate to HAI 5-FU/LV was lower than the previously reported response rates to hepatic arterial chemotherapy of 22-48% [11,18,19]. The median TTP was similar to that reported by Bouchahda et al. (4.5 months) [20] but inferior to those reported in other studies (12-24 months) [11,18,19]. These different results could have arisen from differences in study populations. Previous studies with heavily treated patients reported a median TTP similar to the current study [20]. Other studies with chemotherapy-naïve patients reported higher response rates and longer TTP [11,18,19]. In the current study, the median TEP was equal to, or longer than, the THP. This finding could be attributed to the use of 5-FU and LV as the HAI agent.
Neurotoxicity (not reported) and hematologic toxicities (0-14.2%) were less common than for second-line systemic chemotherapy with similar 5-FU dose intensity [15]. The frequency of all and grade 3 oral mucositis (78.6% and 14.3%, respectively) in patients treated with HAI 5-FU/LV was similar to that observed in patients treated with systemic infusion of 5-FU/LV (75% and 11.5%, respectively) [11]. Local complications such as hyperbilirubinemia and alkaline phosphatase elevations (21%) were lower and milder than were those with HAI FUDR (38%) [19]. In contrast to FUDR, which has a hepatic extraction rate of more than 95%, 5-FU can achieve a high intrahepatic concentration while maintaining a significant systemic concentration because it has a hepatic extraction ratio of 10-80% depending on the infusion dose rate [21]. These pharmacokinetic features could explain the efficacy and toxicity of HAI 5-FU/LV.
Catheter-related complications were catheter thrombosis, displacement, and infection. The rate of these complications was lower than in other studies [22,23]. A surgically implanted port catheter system results in a higher port failure rate than a radiologically implanted system [24] and can result in procedure-related morbidities that can lead to a lack of survival benefit from treatment [25]. Radiologic placement of the catheter in the current study contributed to the lack of procedure-related complications.
This is a retrospective study and has limitations because of its small sample size. However, the results of the present study demonstrate that HAI 5-FU/LV is feasible, has few toxicities or catheter-related complications, and could be an alternative salvage option for patients who fail with treatment using systemic infusion of 5-FU/LV. The results of the present study suggest that readministration via the hepatic artery of a chemotherapeutic agent to which patients have already been exposed could be a feasible salvage option for patients with refractory CRC, with metastases confined to the liver. Thus, prospective studies evaluating the potential of hepatic arterial chemotherapy are warranted.
Notes
No potential conflict of interest relevant to this article was reported.