Clinical Outcomes of Delayed Clearance of Serum HBsAg in Patients with Chronic HBV Infection
Article information
Abstract
Background
Spontaneous delayed clearance of hepatitis B surface antigen (HBsAg) in patients with chronic HBV infection is a rare event. The aim of this study was to investigate the incidence of delayed clearance of serum HBsAg in chronic HBV infection and to determine the characteristics and clinical outcomes of HBsAg delayed clearance in Korean patients.
Methods
From April 1981 to June 2003, 4,061 patients who were positive for HBsAg were evaluated retrospectively. The following assessments were undertaken in 47 patients who had spontaneous delayed clearance: liver biochemistry, viral markers, α-fetoprotein levels, and radiographic examinations including ultrasonography every three to six months for 6-264 months (median 87.9 months).
Results
Twenty-four of 47 patients were asymptomatic carriers. The others included seven patients with chronic hepatitis, seven with liver cirrhosis and nine with hepatocellular carcinoma. The estimated annual incidence of HBsAg seroclearance was 0.4%. The time span from positive HBsAg to HBsAg seroclearance in the AHC, CH, LC, and HCC was 62.9, 141, 63, and 95.3 months during follow up. Twenty-four of 24 AHC remained normal, 5 of 7 CH remained as CH and 2 patients remained normal, 1 of 7 with LC developed HCC and 6 of the LC remained as LC, and 4 of 9 HCC patients died.
Conclusion
The clinical course following delayed clearance of HBsAg had diverse outcomes from AHC to HCC. Therefore, these patients require close follow up for the possible development of hepatocellular carcinoma following HBsAg clearance.
INTRODUCTION
The Hepatitis B virus (HBV) is the main cause of acute and chronic liver disease worldwide1, 2). The presence of hepatitis B surface antigen (HBsAg) in the serum for more than six months defines the state of chronic HBV infection3, 4). The presence of chronic HBV infection is associated with severe sequelae such as cirrhosis and hepatocellular carcinoma (HCC)5, 6). Patients who cannot clear the HBV after an acute infection generally carry it indefinitely. However, in a very small proportion of these patients, a spontaneous delayed clearance of the HBsAg may occur during the course of chronic infection7-10).
Generally, spontaneous delayed clearance of HBsAg has been associated with a better prognosis than a persistent HBsAg infected state. Chen8) et al reported from Taiwan that three (1.6%) of 189 non-cirrhotic patients with seroclearance developed liver cirrhosis and that HCC developed in 1 (3.4%) of 29 patients with cirrhosis and in 2 (1.1%) of 189 non-cirrhotic patients during a mean period of 63 months after HBsAg seroclearance. Fattovich13) et al also reported that patients with compensated HBV liver cirrhosis, with HBsAg delayed clearance, have a better prognosis than the patients with persistent HBV infection do. However, Huo14) et al reported that 33% of 55 patients with seroclearance developed serious sequelae including 20% with HCC and 9% with cirrhosis during a mean follow up period of 23 months after delayed seroclearance.
Although many studies have been reported on the course of spontaneous delayed seroclearance of HBsAg, the prognosis following delayed seroclearance has not been well defined. This retrospective study was designed to investigate the rate of delayed clearance of serum HBsAg in chronic HBV infection and determine the clinical outcomes of patients with HBsAg delayed clearance in Korea.
MATERIALS AND METHODS
Patients
There were 4,061 patients newly diagnosed with chronic hepatitis B from April 1981 to June 2003. They were followed every three to six months at the Kangnam St. Mary's Hospital in Seoul, Korea. The enrolled patients had no co-infections such as HCV, HDV or HIV. Patients identified with chronic infection were HBsAg positive for more than six months and were regularly followed in the out patient department. The follow up period ranged from six to 264 months a mean period of 87.9 months.
Methods
All patients were tested at the first visit for the following: HBsAg (hepatitis B surface antigen), antibody to HBsAg (anti-HBs) (Abbott Laboratories, IL, USA), HBeAg (hepatitis B e antigen), antibody to HBeAg (anti-HBe), antibody to hepatitis B core antigen (anti-HBc) (Dainabot co., Tokyo, Japan), serum aminotransferase (AST), alanine aminotransferase (ALT), albumin, globulin, bilirubin, alkaline phosphatase, glutamyl transpeptidase, prothrombin time, Alfafetoprotein, and HBV DNA (Quantiplex branched DNA assay, Bayer Diagnostics, Berkeley, CA, USA; sensitivity > 7×105 copies/mL). Follow up included testing for HBsAg and anti-HBs at six-month intervals.
HBsAg seroclearance was defined as the absence of serum HBsAg on repeated testing for a period of at least six months and during subsequent follow-up until the time of analysis. Those patients who showed spontaneous delayed clearance of serum HBsAg were followed at intervals less than every six months. Delayed clearance of HBsAg was defined by a persistent absence of HBsAg recorded in at least two consecutive specimens from patients with chronic HBV infections. During a mean period of 87.9 months, the characteristics of patients who showed delayed HBsAg clearance were evaluated using biochemistry, viral markers and radiographic examinations including ultrasonography.
The diagnostic criteria used were as follows12). The asymptomatic healthy carriers were those with a persistent normal serum alanine aminotransferase level for at least 2 years on periodic biochemical examinations every three or six months. The patients with chronic hepatitis had intermittent or sustained elevations of liver function tests and a necroinflammatory score above 4 from liver biopsy specimens. The patients with liver cirrhosis had laboratory data including low serum albumin and platelet levels with features of portal hypertension. The diagnosis of HCC was made by imaging studies such as ultrasonography and/or computed tomography (CT) and AFP levels > 400 ng/mL.
Results
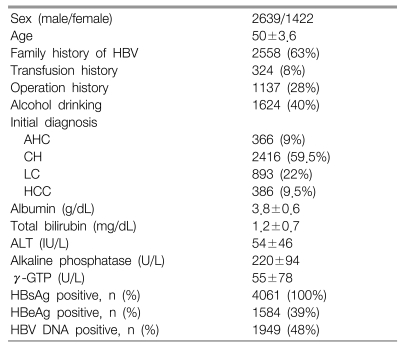
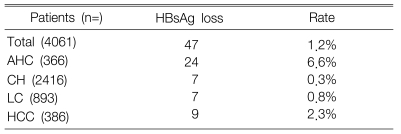
The patient characteristics of the 4,061 included in this study are presented in Table 1. During the period of 6-264 months of follow up (mean 87.9 months) of the enrolled patients, 47 (1.2%) of the 4,061 patients had delayed clearance of serum HBsAg. The accumulated annual incidence of HBsAg seroclearance was 0.4%. HBsAg seroclearance was identified in 24 (6.6%) out of 366 patients that were asymptomatic healthy carriers, 7 (0.3%) out of 2,416 patients that developed chronic hepatitis, 7 (0.8%) out of 893 patients that developed liver cirrhosis and 9 (2.3%) out of 386 patients who developed HCC (Table 2).
At the time of the diagnosis of HBsAg seroclearance, there were 24 (51%) asymptomatic healthy carriers and seven (14.9%) patients with chronic hepatitis. The number of patients with cirrhosis and HCC were seven (14.9%) and nine (19.1%) from the 47 patients, respectively. The mean age at enrollment was 50±3.6 and the mean age at HBsAg seroclearance was 46.2±15.7. The HBeAg at enrollment among the 47 patients with HBsAg seroclearance was 24 negative, nine positive and 14 not determined. The HBsAb state at HBsAg seroclearance was 25 positive and 22 negative. The time span from positive HBsAg to HBsAg seroclearance in the AHC, CH, LC and HCC was 62.9, 141, 63, and 95.3 months during follow up, respectively. The diagnosis at the last visit of the enrolled patients was as follows: 24 of 24 AHC remained normal, 5 of 7 CH remained with CH and 2 patients remained normal; 1 of 7 LC patients developed HCC, 6 of the LC patients remained LC, and 4 of 9 HCC patients died.
DISCUSSION
Patients with chronic HBV infection usually develop severe sequelae including cirrhosis and hepatocellular carcinoma. In a very small proportion of these patients, spontaneous delayed clearance of HBsAg may occur during the course of chronic infection. The results of this study showed that delayed serum HBsAg clearance was a very rare event. The incidence of spontaneous delayed clearance from serum of HBsAg was 1.2% (47 out of 4,061 patients) in our study. The accumulated annual incidence was 0.4%. Previous reports of HBsAg seroclearance suggested a 0.1% to 0.8% annual incidence1, 10). In 1991, Liaw11) et al reported that 1.9% of biopsy-proven chronic hepatitis patients, and 2.2% of asymptomatic chronic carriers, cleared HBsAg from their serum during a mean follow up period of 4.0±2.3 years. In a Japanese study on spontaneous clearance of HBsAg in chronic carriers, 29% of chronic carriers, with a yearly incidence of 2.5%, had clearance of the serum HBsAg7). In a Turkish study, during a mean follow up period of 36.8 months, 9.7% of patients cleared their HBsAg spontaneously15). In a European study, a 10% rate of HBsAg seroclearances in chronic carriers with HDV antibodies was reported13).
The prognosis after spontaneous delayed HBsAg seroclearance was generally good. In our study, asymptomatic healthy carriers were identified in 24 out of 47 patients with HBsAg seroconversion. By contrast, serious life threatening sequelae such as cirrhosis (7 of 47 patients, 14.9%) and HCC (9 of 47 patients, 19.1%) developed in some patients followed during this investigation. These findings support several prior short-term and long-term studies7, 8, 11, 13, 14). Chen8) et al reported that the patients who had concurrent HCV and/or HDV infection, before spontaneous HBsAg seroclearance, had a significantly higher incidence of complications with a less favorable prognosis. However, Huo14) et al reported that seroclearance of HBsAg, in chronic carriers, does not imply a good prognosis; they found a 29.8% overall cumulative probability of complications in such patients. However, other investigators have reported lack of correlation with superinfections such as HCV and/or HDV16). None of our enrolled patients had concurrent co-infections. Our findings of a favorable prognosis in patients with AHC and CH, with HBsAg seroclearance, may be due to this difference from the patients reported by Huo14) and/or Chen8) et al. However, the prognosis of LC and/or HCC patients after seroclearance was less favorable; 1 of the LC patients progressed to HCC.
The mechanisms underlying delayed serum HBsAg clearance remain unknown. Sheen17) et al and Liaw18) et al reported that superinfection with HCV and/or HDV had a role in the termination of the chronic HBsAg carrier or chronic hepatitis state. Moreover, Yeh19) et al reported that seroclearance of HBsAg could be explained by the presence of defective pre-S/S genes in some patients, whereas superinfection with other viruses played a more important role. Cirrhosis and HCC also develop in cases with spontaneous HBsAg seroclearance. Immune clearance or viral integration into the liver tissue may weaken viral replication, and may play a role in HBsAg seroclearance14, 20-22). Therefore, superinfection, cirrhosis and/or immune factors are all likely to be involved in the underlying clearance mechanisms. The annual incidence of HBsAg seroclearance in Western countries has been reported to be 1% to 2%23, 24), in Taiwan 0.1%/yr10) and 0.4%/yr in our study on Korean patients. These results could be explained by the occurrence of infection during the perinatal period or childhood in hyperendemic areas; however, further study is needed to confirm the causes.
The limitations of this study are as follows; first, an accurate determination of the initial infection was difficult. Second, the present study did not show the effect of HBV DNA levels on HBsAg seroclearance. Third, detailed comparisons were not possible because the relevant data such as the effect of treatment with interferon or other antiviral agents was not available.
In conclusion, the incidence of delayed HBsAg clearance during chronic HBV infection is low. The prognosis of patients with delayed serum HBsAg clearance is good except for those patients who develop cirrhosis or HCC. Long-term follow up of HBsAg seroclearance may be an important approach to elucidating the natural history of HBsAg clearance and eradication of the hepatitis virus itself. Furthermore, patients with liver cirrhosis require meticulous followed up for serious life threatening complications.
Notes
This article was financially supported by grants from the Medical College of the Catholic University of Korea.