Autoimmune Chronic Pancreatitis Relapsing Despite the Maintenance Dose of Steroid
Article information
Abstract
Autoimmune chronic pancreatitis is a disease characterized by diffuse swelling of the pancreas, irregular narrowing of the main pancreatic duct and elevated levels of serum IgG, and lymphoplasmacytic infiltration is observed on histologic examination. Steroid therapy can dramatically reverse the clinical symptoms and the histologic and radiologic findings. It is known that recurrence is very rare after successful steroid treatment. Furthermore, there have not yet been any reports about a case that relapsed during maintenance therapy with low dose steroid.
We experienced a rare case of autoimmune chronic pancreatitis that relapsed despite maintenance therapy with low-dose steroid, and the patient again responded to high-dose steroid.
INTRODUCTION
Autoimmunity has recently been examined as one of the etiologies of chronic pancreatitis1). In this type of chronic pancreatitis, such characteristics as the increased IgG level, the presence of autoantibodies, the occasional association with other autoimmune diseases and the lymphoplasma cell infiltration in the pancreas provide circumstantial evidences that autoimmune mechanism may be involved in the pathogenesis2,3). Above all, a dramatic response to steroid in most patients strongly suggests that autoimmunity is an important pathogenetic mechanism in the development of this disease because ordinary chronic pancreatitis does not respond to steroid. Steroid therapy leads to improvement of the clinical symptoms, normalization of the IgG level and also regression of the diffuse enlargement of the pancreas and the irregular narrowing of the main pancreatic duct4-9). After successful treatment by steroid, it is known that the recurrence of this disease is rare4). Furthermore, there have been no cases reported that have relapsed during low dose maintenance with steroid.
We report here on our experience with a rare case of autoimmune chronic pancreatitis that relapsed despite maintenance therapy with low-dose steroid, and it again responded to high-dose steroid treatment.
CASE REPORT
A 59 year old man was admitted to another hospital because of epigastric pain and jaundice. The patient had been healthy until three months earlier when he began to experience postprandial epigastric pain and he lost 9 kg of weight. Abdominal US revealed diffuse swelling of the pancreas that was especially more prominent in the head portion. The patient was transferred to Asan Medical Center under the impression of pancreatic cancer.
The patient drank only a little alcohol and had no history of diabetes mellitus, hypertension, pancreatitis and biliary stone disease. On physical examination, there was a mild tenderness over the epigastric area. The other physical examination findings were unremarkable. The total bilirubin was elevated to 7.9 mg/dL (normal range: 0.2~1.2 mg/dL). Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were elevated to 214 IU/L (normal range: < 40 IU/L) and 68 IU/L (normal range: < 40 IU/L), respectively. γ-Glutamyl transpeptidase (γ-GTP) and alkaline phosphatase (ALP) were also elevated to 385 IU/L (normal range: 11~63 IU/L) and 213 IU/L (normal range: 40~120 IU/L), respectively. Serum amylase was 46 U/L (normal range: 30~110 U/L), and serum lipase was 22 U/L (normal range: 22~51U/L). The CA19-9 was 24.5 U/mL (normal range: < 37 U/mL).
The total IgG concentration was normal (1,230 mg/dL, normal range: 694~1,618 mg/dL), but the serum IgG4 had not been initially measured. The test for lupus anticoagulant was positive, while the other autoantibodies such as anti-nuclear antibody, anti-mitochondrial antibody, rheumatoid factor and anti-smooth muscle antibody were all negative. Anti-carbonic anhydrase II antibody and anti-lactoferrin antibody were not measured.
A dynamic CT scan revealed diffuse enlargement of the whole pancreas. An ERCP showed diffuse, irregular narrowing of the main pancreatic duct (Figure 1) and narrowing of the intrapancreatic common bile duct. An US-guided core needle biopsy was preformed, and we targeted the enlargedportion of the pancreatic head for differentiating between benign and malignant disease of the pancreas. Pancreatic histology confirmed marked lymphoplasma cell infiltration and fibrosis with acinar atrophy.

Endoscopic retrograde pancreatogram that was done at the first attack. It showed diffuse irregular narrowing of the main pancreatic duct.
The patient was diagnosed as having autoimmune chronic pancreatitis based on the diagnostic criteria (characteristic pancreatic imaging, histologic findings and positive autoantibody) for autoimmune pancreatitis proposed by the Japan Pancreas Society10). He was treated with prednisolone (40 mg/day) and by inserting a plastic stent (10 Fr, 5 cm) for the narrowing of the common bile duct. Three months after treatment with prednisolone (40 mg/day), a follow-up ERCP showed dramatic improvement of the narrowing (Figure 2) of both the main pancreatic duct and the common bile duct. The swollen pancreas returned to normal size on dynamic CT scan. The abnormal laboratory findings were normalized and he gained about 4 kg of weight. As a result, the biliary stent was removed and the daily dose of prednisolone was then gradually tapered to 5 mg over a period of 6 months. Since then, the patient had taken low dose steroid (5 mg/day) without discontinuation.

Endoscopic retrograde pancreatogram that was done 3 months after steroid treatment. Here the narrowing of the main pancreatic duct had been ameliorated by steroid treatment.
Nine months after maintenance therapy with 5mg prednisolone/day (sixteen months after the start of steroid treatment), the patient again complained of epigastric pain and jaundice of two days' duration. The total bilirubin was elevated to 7.4 mg/dL. AST, ALT and γ-GTP were elevated to 366 IU/L, 268 IU/L and 170 IU/L, respectively. Serum ALP and amylase were within normal range, while serum lipase was mildly elevated to 64 U/L. Characteristically, the serum IgG4 concentration was markedly increased (840 mg/dL, normal range: 6~121 mg/dL) with a normal concentration of total IgG. The test for the initially positive lupus anticoagulant was negative. A dynamic CT scan again revealed diffuse swelling of the pancreas. The ERCP showed segmental irregular narrowing of the main pancreatic duct in the tail portion (Figure 3) and the narrowing of the intrapancreatic common bile duct.

Endoscopic retrograde pancreatogram (arrows) that was done on relapse. It showed the segmental irregular narrowing of the main pancreatic duct in the tail portion.
In spite of the maintenance therapy of low dose prednisolone (5 mg/day), the patient's relapse into autoimmune pancreatitis was strongly suspected. High dose prednisolone (40 mg/day) was administered again and the biliary stent was re-inserted into the common bile duct. Three months after therapy with a daily dose of 40 mg prednisolone, the abnormal liver function tests were normalized and serum IgG4 concentration also returned to normal. Yet it is interesting that the test for anti-nuclear antibody, which was negative on the first attack and on relapse, turned positive with a titer of 1:80 and with a nucleolar pattern during the retreatment for relpase. A follow-up ERCP demonstrated obvious improvement for the narrowing of both the main pancreatic duct (Figure 4) and the common bile duct. His symptoms including the epigastric pain also disappeared. Six months after maintenance therapy with 10 mg prednisolone/day and tapering by 5 mg per month, he is in good health.
DISCUSSION
Horiuchi et al11). have previously reported that during the mean follow-up period of 56 months, only one (4.3%) of 23 patients with autoimmune chronic pancreatitis relapsed after cessation of their corticosteroid therapy. In a similar fashion, we experienced a case of relapse for one (5.8%, the present case) of 17 patients who had good responses to steroid during the mean follow-up period of 12 months12). Although a relapse of autoimmune chronic pancreatitis after successful steroid therapy has been anecdotally reported, there have been no case reports about disease progress and treatment after relapse. In addition, there has been no report about a case that relapsed during maintenance therapy of steroid, but that went into remission after retreatment of high dose steroid.
Glucocorticoids inhibit the access of leukocytes to inflammatory sites; steroid interferes with their function and also the function of fibroblasts and endothelial cells at those sites, and steroid suppresses the production and the effects of humoral factors13). Most patients with autoimmune chronic pancreatitis are known to have dramatic responses to steroid within one month on the radiologic and biochemical findings4-9,11). Moreover, it is very interesting that to what extent the fibrosis of the pancreas could be reversed after therapy14,15). Until now, however, a consensus opinion on the duration of steroid treatment and the timing of dose reduction or the dose of maintenance therapy, if needed, has not yet been established. Also, any specific disease marker that can predict an early relapse or the natural course of the disease is currently unknown. According to the literature, a dose of 30 to 40 mg/day of steroid should be initially administered, then the high dose of steroid is gradually tapered by 2.5 to 5 mg/week if the abnormal clinical, radiologic and laboratory findings revert to normal. Eventually the steroid is completely discontinued or maintained at a dose of 5~10 mg/day according to the preference of the doctor8,10,16).
In the present case, the swelling of the pancreas and the narrowing of main pancreatic duct were alleviated by the steroid treatment. The narrowing of the CBD secondary to autoimmune chronic pancreatitis was initially treated by an endoscopic approach, but the biliary stent was not necessary after remission. Steroid at an initial dose of 40 mg/day was administered for 3 months and the dose was gradually tapered to 5 mg/dayfor 6 months, and then maintained at a dose of 5 mg/day for 7 months. During maintenance therapy with steroid, the patient relapsed, but he responded again to high dose steroid at 40 mg/day. We observed that re-remission could again be achieved with high dose steroid for patients who relapsed after their initial successful treatment with steroid. The maintenance dose of steroid over a physiologic dose of 7.5 mg/day may be required in a relapsing case because a dose below this physiologic dose may not be sufficient for suppressing the autoimmunity in a state of secondary adrenal insufficiency caused by long-term exogenous steroid administration, as was noted in our case. Also, for autoimmune chronic pancreatitis that frequently relapses,the switch to other immunosuppressive agents such as azathioprine may be tried in order to reduce the life-threatening adverse effects of steroid, but further study is required to identify the effectiveness of other agents.
Hamono et al8). reported that serum IgG4 concentrations are closely associated with disease activity. In our case, the serum IgG4 concentration was initially not measured, but the serum IgG4 concentration at relapse was markedly increased despite the normal concentration of total IgG, and it was again normalized after therapy with high dose steroid. Close monitoring of the serum IgG4 concentration can be helpful to predict early relapse, as in our case. It was interesting that the lupus anticoagulant was positive on first attack; it turned negative 3 months after steroid therapy and then reappeared on relapse. In addition, the anti-nuclear antibody that was initially negative emerged during treatment for relapse (Table 1). These findings give us important information, that autoantibodies commonly associated with autoimmune chronic pancreatitis should be monitored periodically during the follow-up period even if they were initially negative. It has been reported that the total IgG level commonly increases for patients with chronic autoimmune pancreatitis and it returns to normal after steroid therapy. Even though the total IgG level did not increase during the first attack and in follow-up period in our case, we suggest that closely monitoring the serum IgG concentration would be useful as well. We think that the identification of a reliable marker for relapse prior to the development of clinical symptoms and signs may be important to avoid further invasive procedures and for preventing irreversible damage to the pancreas by inappropriate administration of steroid.
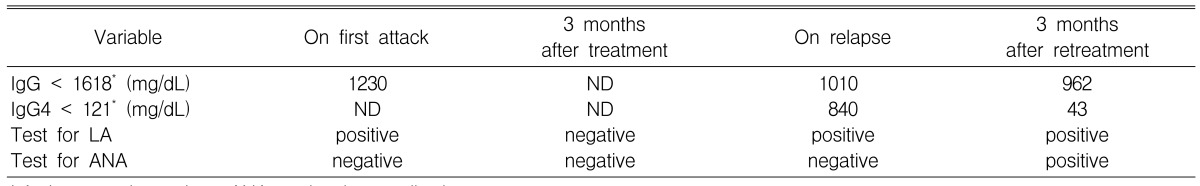
Results of immunological laboratory testing on the first attack, 3 months after treatment, on relapse and 3 months after retreatment
In summary, our experience gives us the following important clinical implications; first, for autoimmune chronic pancreatitis that relapses after initial remission or even during maintenance therapy, remission can again be achieved with medical treatment using high dose steroid. Second, continuous monitoring of the total IgG, IgG4 or autoantibodies may be needed during the follow-up period for monitoring the disease activity and for early prediction of relapse.
