Role of Blocking TSH Receptor Antibodies on the Development of Hypothyroidism and Thyroid Atrophy in Primary Myxedema
Article information
Abstract
We studied blocking type TSH receptor antibodies in 28 patients with primary myxedema and 21 patients with goitrous Hashimoto’s thyroiditis by measuring the ability of their IgG to inhibit TSH binding to its receptor, and to inhibit TSH-stimulated cAMP increases and 3H-thymidine incorporation in a rat thyroid cell line, FRTL-5. The incidences of TSH binding inhibitor immunoglobulin (TBII), thyroid stimulation blocking antibody (TSBAb) and thyroid growth blocking antibody (TGBAb) in patients with primary myxedema were 53.6%, 75% and 65.2%, respectively. However, in goitrous Hashimoto’s thyroiditis, these were 14.3%, 0% and 17.7%, respectively. These antibodies inhibited the receptor binding of 125I-bTSH dose-dependently, and also inhibited dose-dependently not only TSH-stimulated but also Graves’ IgG-stimulated cAMP increase and 3H-thymidine incorporation. TBII activities of patients with primary myxedema were significantly correlated with both their TSBAb (r=0.665; p<0.01) and TGBAb (r=0.618; p<0.01) activities. Thirteen patients whose TBII activities were more than 50% had both strong TSBAb (75.1–100%) and TGBAb (57.4–100%) activities. Transient neonatal hypothyroidism was found in an infant born to a mother having potent TBII activities. Serum of the baby also had potent TBII activities and the baby’s IgG inhibited TSH-stimulated cAMP increase and 3H-thymidine incorporation.
These data suggest that a significant proportion of patients with primary myxedema have potent blocking type TSH receptor antibodies. These might play a role in primary myxedema causing hypothyroidism and thyroid atrophy through inhibition of TSH-stimulated cAMP generation.
INTRODUCTION
Recent data indicate that primary myxedema may be associated with the presence of immunoglobulin G (IgG) which inhibits the binding of TSH to its receptor, blocking the effect of TSH on thyroid adenylate cyclase (1–4) and cell growth (4–6). It has been reported that transplacental transfer of maternal IgGs may lead to transient neonatal hypothyroidism (7–9). Thus these blocking type TSH receptor antibodies (TRAb) could play a role in the pathogenesis of hypothyroidism and thyroid atrophy. However, it is uncertain whether TSH binding inhibitor IgG (TBII), thyroid stimulation blocking antibody (TSBAb) and thyroid growth blocking antibody (TGBAb) are the same IgG. The incidence of blocking type TRAb is reported to be frequent in Japanese (10). Although Vitti et al. (11) recently reported a high frequency of blocking type TRAb in this disease, the number of cases is still limited in western countries (10,12). However, we recently encountered several patients with primary myxedema who had a potent TBII (4,8). Thus, we investigated the incidence, characteristics, and pathogenetic importance of blocking TRAb in patients with primary myxedema and compared its inhibiting effect on TSH binding to its receptor with that on both TSH-stimulated adenylate cyclase activation and growth of FRTL-5 cells.
MATERIALS AND METHODS
The IgG fraction was isolated from serum samples, by means of affinity chromatography on columns of protein A-Sepharose CL-4B, of 28 consecutive patients with primary myxedema (7 men and 21 women; age range 18–81 years). All had non-palpable thyroid glands, low serum T4 levels, and elevated serum TSH levels at the time of diagnosis. As controls, IgG from 21 patients (21 women; age range 17–72 years) with goitrous hypothyroidism (biopsy proven and elevated serum TSH levels) and IgG from 24 normal subjects (10 men and 14 women; age range 22–63 years) were studied.
The materials were purchased from commercial sources, as follows: Coon’s modified Ham F12 media from Hazelton (Denver, PA, USA); calf serum, bovine TSH (bTSH), bovine insulin, transferrin, L-glycyl-L-histidyl-L-lysine, hydrocortisone, 3-isobutyl-L-methyl-xanthine (IBMX), HEPES, and sodium dodecyl sulfate (SDS) from Sigma Chemical Co. (St. Louis, Mo, USA); somatostatin from Calbiochemical Co. (La Jolla, CA, USA); methyl-tritiated-thymidine from Amersham (Buckinghamshire, UK); and protein A-Sepharose CL-4B from Pharmacia Fine Chemicals (Uppsala, Sweden).
TBII activity was measured using the TSH receptor antibody kit prepared by R.S.R. Ltd. (Cardiff, Wales, UK) as previously described (13). TBII was expressed as % inhibition of 125I-bTSH binding to the TSH receptor. A TBII value exceeding 15% was considered abnormal or positive.
For the assay of TSBAb, FRTL-5 cells, kindly supplied by Dr L.D. Kohn (NIH, Bethesda, MD, USA), were maintained as previously described (14) for 7 days in medium without TSH before assay. The medium was changed with 300 ul of test IgG (10 g/l) with or without bTSH (0.1 U/l), IgGs were dissolved in Hank’s balanced salt solution (HBSS) without NaCl containing 0.5 mmol/l IBMX, 20 mmol/l HEPES, and 1.0% BSA, pH 7.4. After 2 h incubation at 37°C, cAMP released into the medium was measured by RIA (Immunonuclear, Stillwater, Minnesota, USA). The assay system was sensitive to 5 mU/l bTSH with a response of 1.71 ± 0.07 times the basal cAMP level. All samples were run in triplicate. The intraassay variance was 8.2–12.1% and the interassay variance was 17.1–30.5%. TSBAb activity was expressed as % inhibition of TSH-stimulated cAMP increase, and was calculated as follows: TSBAb (%) = 100 × [1-(cAMP under 0.1 U/l bTSH with test IgG-cAMP under normal IgG/cAMP under 0.1 U/l bTSH with normal IgG-cAMP under normal IgG)]. TSBAb was defined as positive when the value was greater than 2 SD above the mean value produced by the IgG fraction from 24 normal subjects (>37%).
For the assay of TGBAb, FRTL-5 cells were plated as in the TSBAb assay. After 7 days in 5H media, each well was washed with basal medium, then 500 ul of test IgG (5 g/l) in basal medium with 0.1% BSA was added with or without TSH 1 U/l. Seventy-two h later, the media was aspirated, and 250 ul of basal media with 0.1% BSA containing 5 uCi of 3H-thymidine was added to each well and pulse labelling was done for 6 h. After aspiration of supernatant, each well was washed three times with 1 ml of ice cold PBS. Five hundred ul of 10% trichloroacetic acid was added and 10 min later it was washed with PBS again and 500 ul of 2% SDS was added to solubilize the precipitated cells. One h later its radioactivity was counted. TSBAb was expressed as % inhibition of TSH-stimulated 3H-thymidine uptake, and was calculated as follows: TSBAb (%) = 100 × [1-(cpm under 5 g/l test IgG and 1 U/l TSH-cpm under normal IgG/cpm under 5 g/l normal IgG and 1 U/l TSH-cpm under normal IgG)]. A TSBAb value above 40% was considered abnormal.
Statistical analysis was done with Spearman’s rank correlation test, Wilcoxon’s rank sum test, chi square test and Fisher’s exact test. Statistical significance was determined when the p value was below 0.05.
RESULTS
1. Inhibition of TSH Binding to Its Receptor
In the radioreceptor assay for TSH, 15 of 28 IgGs (53.6%) from the patients with primary myxedema had TBII. Thirteen of them showed potent TBII activities, resulting in more than 70% inhibition of 125I-bTSH binding in the assay. On the other hand, 3 of 21 (14.3%) patients with goitrous Hashimoto’s thyroiditis were weakly positive for TBII (Fig. 1).
2. Inhibition of TSH-Stimulated cAMP Increase
Twenty-one (75.0%) of 28 IgGs from patients with primary myxedema had TSBAb. However, none of the patients with goitrous Hashimoto’s thyroiditis had TSBAb. (Fig. 2). The effects of various amounts of IgG prepared from two patients with primary myxedema (patient 1 and 2 in Table 1) on 0.1 U/l TSH-stimulated cAMP increase are shown in Fig. 3a. TSH-stimulated cAMP increases were significantly inhibited by 0.01 g/l IgG from the patients with primary myxedema, and maximum inhibition was obtained with 1–10 g/l IgG, whereas no changes occurred when IgG from a normal subject was added. The same IgGs were tested at 10 g/l against varying concentrations of TSH. At 10 mU/l TSH, cAMP production began to increase and reached its peak at 5 U/l TSH. These IgGs completely inhibited the TSH-stimulated cAMP increase up to 1U/1 (Fig. 3b). All IgGs from patients with primary myxedema had no intrinsic thyroid stimulating activity (data not shown).

Distribution of TSBAb activities in 28 patients with primary myxedema and 21 patients with goitrous Hashimoto’s thyroiditis. The shaded area represents the normal range, as defined from the distribution in 24 normal controls.
(a) Effects of graded doses of IgG from a normal subject and two patients with primary myxedema on 0.1 U/l TSH-stimulated cAMP increases in FRTL-5 cells, ○, Normal subject; •, patient 1; ▴, patient 2. Each point is the mean ± SEM of three determinations, (b) Effects of 10 g/l IgG from a normal subject and 2 patients with primary myxedema on cAMP responses to graded doses of TSH. ○, Normal subject; •, patient 1; ▴, patient 2. Each point is the mean ± SEM of three determinations. Significantly different: ○ vs •, ▴ at 0.01, 0.05, 0.1, 0.5, 1, 5, 10 U/l TSH (p<0.01).
3. Inhibition of TSH-Stimulated 3H-Thymidine Uptake
In 23 patients with primary myxedema, 15 patients (65.2%) were positive for TGBAb (Fig. 4). However, TGBAb were positive in 3 (17.7%) of 17 patients with goitrous Hashimoto’s thyroiditis. The effects of various amount of IgG prepared from two patients with primary myxedema (patient 1 and 2 in Table 1) on 1 U/l TSH-stimulated 3H-thymidine incorporation are shown in Fig. 5a. These IgGs inhibited TSH-stimulated 3H-thymidine incorporation in a dose-dependent manner. The same IgGs were tested at 5 g/l against varying concentrations of TSH. At 1 mU/l TSH, 3H-thymidine incorporation began to increase and reached its peak at 1 U/l TSH. These IgGs completely inhibited TSH-stimulated 3H-thymidine incorporation up to 1 U/l (Fig. 5b). All IgGs from the patients with primary myxedema had no intrinsic growth stimulating activity. On the other hand, 6 of 17 IgGs from the patients with goitrous Hashimoto’s thyroiditis showed intrinsic thyroid growth stimulating activity and 3 of 6 patients who had thyroid growth stimulating activity were positive for thyroid stimulating antibodies (data not shown).
Distribution of TGBAb activities in 23 patients with primary myxedema and 17 patients with goitrous Hashimoto’s thyroiditis. The shaded area represents the normal range, as defined from the distribution in 24 normal controls.

(a) Effects of graded doses of IgG from a normal subject and two patients with primary myxedema on 1 U/l TSH-stimulated 3H-thymidine incorporation into FRTL-5 cells, ○, Normal subject; •, patient 1; ▴, patient 2. Each point is the mean ± SEM of three determinations, b) Effects of 5 g/l IgG from the same patients on 3H-thymidine incorporation into FRTL-5 cells by graded doses of TSH. Significantly different; ○ vs •, ▴ at 0.01, 0.1, 1, 10 U/l TSH (p<0.01).
4. Correlation of TBII, TSBAb, and TGBAb in Patients with Primary Myxedema
TBII activity of patients with primary myxedema was significantly correlated with both their TSBAb activity (r = 0.665; p<0.01) and TGBAb (r = 0.618; p<0.01) activity (Fig. 6). There was also significant correlation (r = 0.55; p<0.01) between TSBAb and TGBAb activity. In 23 patients with primary myxedema whose IgGs were tested in all three activities, 13 patients had all three activities and only 3 patients were negative for all three activities. Thirteen patients whose TBII activities were more than 50% had both potent TSBAb (75.1–100%) and TSBAb (57.4–100%) activities (Fig. 7, Table 1).

Relation between (a) TBII activity and TSBAb activity in 28 patients with primary myxedema (r = 0.665, p<0.01), and (b) TBII activity and TSBAb activity in 23 patients with primary myxedema (r = 0.618, p<0.01). The shaded area represents the normal range, as defined from the ditribution in 24 normal controls.
5. Clinical Features
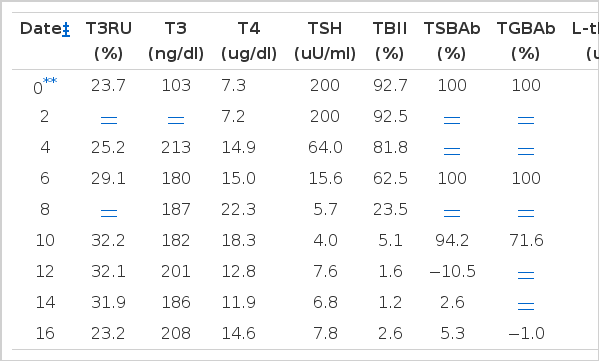
The clinical and laboratory data of the 28 patients with primary myxedema are summarized in Table 1. There were no significant differences in age, sex, titers of thyroid autoantibodies, and radioiodine thyroid uptake between patients with and without blocking type TRAbs. These TBII activities did not change during the thyroxine replacement for 2 to 5 years (Table 2.)
Among 15 patients who had blocking type TRAb, one patient (patient 1 in Table 1) delivered a baby with transient neonatal hypothyroidism. The initial maternal serum sample showed 90.7% TBII activity and the activity did not change during thyroxine treatment (Table 2). At the time of delivery, maternal TBII activity was 92.5%. On the second day of life, the baby’s serum T4 was 7.3 ug/dl, T3 was 103 ng/dl, and TSH was 200 uU/ml. The baby’s TBII activity was 92.7% at birth and decreased gradually and was negative at the 10th week after birth (Table 3). The baby’s IgG inhibited TSH-stimulated cAMP increase and TSH-stimulated 3H-thymidine incorporation completely at birth (Fig. 8), and its inhibitory activities decreased gradually, disappearing completely at the 12th and 16th week after birth, respectively. After these antibodies disappeared, the baby reamined euthyroid without replacement therapy.
6. Inhibition of Graves’ IgG-stimulated cAMP Increase and 3H-thymidine Incorporation
To evaluate whether the binding site of blocking TRAb is the same as that of thyroid stimulating antibody (TSAb), we studied the effects of these IgGs on Graves’ IgG-stimulated cAMP increase and 3H-thymidine incorporation. We used pooled Graves’ IgG from 7 patients with untreated Graves’ disease as TSAb. IgGs prepared from 2 patients with primary myxedema (patient 1 and 2 in Table 1) inhibited Graves’ IgG-stimulated cAMP increase and 3H-thymidine incorporation in a dose-dependent manner (Fig. 9). These dose-dependent inhibitions of IgGs on Graves’ IgG-stimulated cAMP increase and 3H-thymidine incorporation were the same as those of TSH-stimulated responses (Fig. 3a, 4a).

Effects of graded doses of IgG from a normal subject and 2 patients with primary myxedema on 10 g/l Graves’ IgG-stimulated cAMP increase (a) and on 5 g/l Graves’ IgG-stimulated 3H-thymidine incorporation into FRTL-5 cells. ○, Normal subject; •, patient No. 1; ▴, patient No. 2. Each point is the mean ± SEM of three determinations.
DISCUSSION
In this study, we found that 53.6% of the patients with primary myxedema had TBII, and TSBAb and TGBAb were positive in 75% and 65.2%, respectively. Such an incidence is higher than that in previously reported series (1–3, 6, 11, 15–17). All patients whose IgGs showed TBII activities had TSBAb and all but one patient with TBII activities had TGBAb. Moreover, most of the patients with primary myxedema had at least one kind of blocking type antibody. Initially, the occurrence of blocking type TRAb seemed to differ from race to race, because in western countries, primary myxedema with blocking type TRAb was rarely detected (12). But recently an increasing number of European authors have reported the presence of blocking type TRAb in patients with primary myxedema (11, 15–19). Our data support the concept that the incidence of blocking type TRAb in primary myxedema is not infrequent and is a universal finding (10).
Both the TSBAb and TGBAb activity correlated significantly with the TBII activity. The growth-blocking activity in these IgG preparations also correlated with their ability to inhibit TSH-stimulated cAMP increase. Moreover, we found a case of transient neonatal hypothyroidism due to transplacental transfer of maternal blocking type TRAb (9). These findings support the concept that these blocking antibodies are against the TSH receptor or closely related structures, and may play a role in primary myxedema causing hypothyroidism and atrophy by inhibiting TSH-stimulating cAMP generation (1,4). Furthermore, these antibodies inhibited not only TSH-stimulated but also Graves’ IgG-stimulated cAMP increase and 3H-thymidine incorporation. These results suggest that the binding site of blocking type TRAb may be the same as that of TSAb. But we can not explain why the functional properties of blocking type TRAb are different from those of TSAb despite the same binding site in the TSH receptor.
In our study, there was no significant difference of any clinical and laboratory parameters between the blocking type TRAb positive group and negative group. This finding is a little different from the result of Konishi et al. (2), who demonstrated that thyroid uptake in patients with blocking type TRAb was significantly lower than that in patients without blocking type TRAb. This discrepancy may be related to the difference in the duration of illness before diagnosis. Another interesting point is that in our study, the titer of blocking type TRAb did not change during the thyroxine replacement for 2 to 5 years. This is in contrast to the report of Vitti et al. (11), who demonstrated that the prevalence of TSBAb in patients with primary myxedema under treatment was markedly low compared with untreated patients. We could not explain this discrepancy. It should be clarified whether the titer of blocking type TRAb can be changed by antithyroid drugs as can that of stimulating TRAb of Graves’ disease.
Primary myxedema has been though to be the end result of long-standing goitrous Hashimoto’s thyroiditis. Hypothyroidism and thyroid atrophy in this disease were considered to result from the thyroidal unresponsiveness to circulating TSH due to irreversible destruction by cytotoxic antibodies and cell mediated immunity (20). In our study, however, all patients had no history of previous goiter and some of them were too young to have long-standing goitrous Hashimoto’s thyroiditis. Moreover, the high incidence of blocking type TRAb in primary myxedema compared with that in goitrous Hashimoto’s thyroiditis may reflect differences in the autoimmune mechanism involved in these patients. In HLA studies, DR3 antigens were shown to be associated in primary myxedema and DR5 in Hashimoto’s thyroiditis (21). It suggests that these two diseases may be genetically different.
From this study, we could conclude that the vast majority of patients with primary myxedema have potent blocking type TRAb. These antibodies might play a role in primary myxedema causing hypothyroidism and thyroid atrophy by inhibiting TSH-stimulated cAMP generation.
Acknowledgements
We would like to thank Miss K S Min and J G Lee for their technical assistance, and Miss E J Kwack and J H Choi for their secretarial assistance.
Notes
This work was supported in part by Chung-Ram research grants from the Korean Association of Internal Medicine (1988)