The Role of C-Reactive Protein on the Long-Term Clinical Outcome after Primary or Rescue Percutaneous Coronary Intervention
Article information
Abstract
Background
We examined the clinical and angiographic outcomes, success rate of the percutaneous coronary intervention (PCI) and long-term survival rate after primary or rescue PCI in patients with acute myocardial infarction (AMI) according to the level of the C-Reactive Protein (CRP) on admission.
Methods
Two hundred and eight consecutive patients with AMI who underwent primary or rescue PCI between 1997 and 1999 at Chonnam National University Hospital were divided into two groups: Group I (n=86, 59.9 ±9.3 years, male 74.4%) with a normal CRP (<1.0 mg/dL, mean value=0.43±0.14 mg/dL) on admission and Group II (n=122, 59.1±10.4 years, male 83.6%) with an elevated CRP (≥=1.0 mg/dL, mean value=3.50±0.93 mg/dL) on admission.
Results
There were no significant differences in the baseline characteristics noted between the two groups. The incidence of cardiogenic shock was higher in Group II than in Group I (Group I; 3/86, 3.5% vs. Group II; 15/122, 12.3%, p=0.026). The coronary angiographic findings did not differ between the two groups. The ejection fraction and Thrombolysis In Myocardial Infarction flow grade improved after PCI in both groups. The primary success rate of PCI was 94.2% (81/86) in Group I and 95.1% (116/122) in Group II (p=0.776). The survival rates for Group I were 97.7%, 97.7% and 96.5%, and those for Group II were 91.8%, 91.0% and 86.9% at 1, 6 and 12 months, respectively (p=0.043 at 1 month, p=0.040 at 6 months, p=0.018 at 12 months).
Conclusion
A high incidence of cardiogenic shock and worse long-term survival after PCI are observed in AMI patients with an elevated CRP.
INTRODUCTION
Percutaneous coronary intervention (PCI) has been introduced as one of the effective methods in the treatment of acute myocardial infarction (AMI), and an understanding of the pathophysiologic changes involved in the underlying coronary arterial lesion after PCI may be important1, 2). An inflammatory reaction is one of the important pathologic findings in the atheromatous plaque of patients with acute coronary syndrome, and lymphocytes and monocytes/macrophages accumulate at the site of the plaque rupture3, 4).
One of the acute phase reactants, C-reactive protein (CRP), is synthesized in the liver by stimulation of cytokines, such as interleukin-6, and begins to elevate within 6 hours after stimulation of the liver by cytokine5, 6). The serum level of CRP reflects the overall systemic inflammatory reaction within the body and is a simple and objective index7).
The level of CRP is closely related to atherosclerosis in coronary, cerebral and peripheral arteries8). An increase in the serum CRP is known to relate with cardiovascular complications, such as sudden cardiac death or AMI9). In the Multiple Risk Factor International Trial (MRFIT), the level of the CRP was significantly related with mortality due to coronary artery diseases10).
The effects of the initial CRP level on the long-term mortality in patients with AMI, especially after primary or rescue PCI, have not been reported. Our study sought to observe the effects of the serum level of the CRP at the time of admission on the short- and long-term prognosis in patients with AMI after primary or rescue PCI, and the long-term prognosis in patients with AMI after primary or rescue PCI.
METHODS
1. Subjects
All consecutive patients with AMI, who were admitted and underwent primary or rescue PCI at The Heart Center of Chonnam National University Hospital between January 1997 and December 1999, were included in this study. All patients had chest pain for a duration of less than 6 hours and prolonged chest pain for more than 30 minutes not responsive to nitroglycerin or ST elevation of more than 1 mV in two or more limb leads or 2 mV in two consecutive precordial leads. Primary PCI was performed in 177 patients (59.4±9.7 years-old, M:F=141:36) and rescue PCI in 31 patients (59.7±11.4 years-old, M:F=25:6). The two hundred and eight patients were divided into two groups; Group I (n=86, 59.9±9.3 years-old, M:F=64:22, CRP less than 1 mg/dL) and Group II (n=122, 59.1±10.4 years-old, M:F=102:20, CRP higher than 1 mg/dL), and the clinical and angiographic characteristics, success rate of the PCI and the one-month, six-month and 12-month mortality were compared retrospectively between the two groups during a one-year clinical follow-up.
2. Laboratory and angiographic assessments
A blood sample was obtained on arrival at the emergency room and stored in a refrigerator. The serum level of the CRP was measured by the latex photometric immunoassay method, and 1 mg/dL was set as the cut-off value for the comparison between the high and low groups. The left ventricular ejection fraction was compared by the Simpson method using two-dimensional echocardiography. A coronary angiogram was performed through the femoral or radial arteries. Coronary artery lesions were classified using the American College of Cardiology/American Heart Association system, in which a stenosis of more than 75% defined as a significant lesion11). The lesion location, involved vessel number, lesion characteristics and presence of an intracoronary thrombus on the coronary angiogram were compared between the two groups, and the vessel patency of the infarct-related artery was assessed by the Thrombolysis in Myocardial Infarction (TIMI) flow score12). TIMI 0 was defined as a total occlusion without any distal flow below the lesion, TIMI 1 as trivial distal flow without complete visualization of the entire artery, TIMI 2 as complete visualization of the entire coronary artery with a slow flow rate and TIMI 3 as complete visualization of the entire artery with a normal flow rate. Successful revascularization was defined as a TIMI flow score of more than grade 2 and residual stenosis less than 50%13).
Rescue PCI was defined as a dilation of the occluded infarct-related artery less than 6 hours after the onset of chest pain in patients with persistent ST segment elevation and persistent chest pain after thrombolytic therapy. Urokinase or tissue plasminogen activator was used for thrombolysis and 100–300 mg of aspirin was administered daily. Heparin was administered to maintain an activated partial thromboplastin time of about 2 times above the normal control. After discharge from the hospital, the patients were observed at the out-patient clinic at 4 week intervals, and the cardiovascular mortality was assessed at 1, 6 and 12 months after the PCI. Restenosis was defined as diameter stenosis more than 50% by the Phillips quantitative coronary angiogram analysis system.
3. Statistical analysis
For the statistical analysis, the unpaired t-test, Chi-square test and multiple logistic regression analysis were performed using SPSS-PC 10.0 (Statistical package for the social sciences, SPSS Inc. Chicago, IL, U.S.A.) and MS Windows®, and the results were designated as mean±standard deviation. A value of p less than 0.05 was considered as significant.
RESULTS
1. Clinical characteristics
The age and sex ratios did not differ between the two groups (p=0.599, 0.104 respectively). There were no differences in these risk factors between the two groups (p=0.472, 0.373, 0.054 and 0.346, respectively) (Table 1). The incidence of cardiogenic shock was 3 cases in Group I (3.5%) and 15 in Group II (12.3%), and was higher in Group II than in group I (p=0.026) (Table 1). The values of Troponin I and T and ESR were higher than those in Group I (p<0.001, <0.001 and =0.026, respectively) (Table 1).
2. Coronary angiographic characteristics
The time interval between the onset of symptoms and arrival at the emergency room, and the interval between the onset of symptoms and the time of the PCI did not differ between the two groups (p=0.860 and 0.843, respectively) (Table 1). The number of patients that underwent rescue PCI or primary PCI did not differ between the two groups (p=0.747) (Table 1). The number of vessels involved on diagnostic coronary angiography did not differ between the two groups (p=0.753) (Table 2). The mean number of vessels involved was 1.60±0.71 in group I and 1.54±0.71 in group II. The order of frequency in the number of vessels involved was single vessel disease, two vessel disease and three vessel disease.
Lesions involving the left anterior descending artery were the most common, but the lesion distribution did not differ between the two groups (p=0.642) (Table 2). The lesion morphology assessed according to the ACC/AHA classification was not significantly different between the two groups (p=0.634) (Table 2). An intracoronary thrombus was not different between the two groups (p=0.450) (Table 2). The mean TIMI flow grade did not differ between the two groups (p=0.087) (Table 2).
3. Results of PCI
The mean TIMI flow grade represented a significant improvement after the PCI (p<0.001) (Table 4), and there was no significant difference between the two groups (p=0.863) (Table 3). The primary success rate resulted in no difference between the two groups (p=0.776) (Table 3).
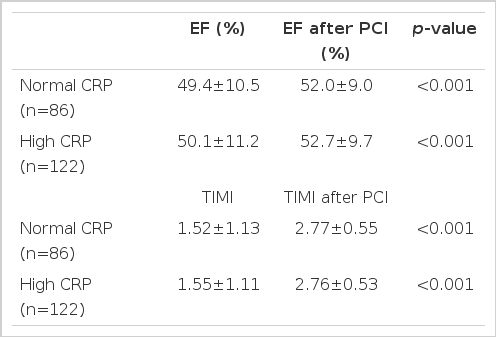
Improvement of the ejection fraction and Thrombolysis In Myocardial Infarction flow after percutaneous coronary intervention
4. Left ventricular ejection fraction
The ejection fraction measured by two-dimensional echocardiography on admission did not differ between the two groups (p=0.673) (Table 1). After the PCI, the ejection fraction significantly improved in both groups (p<0.001) (Table 4).
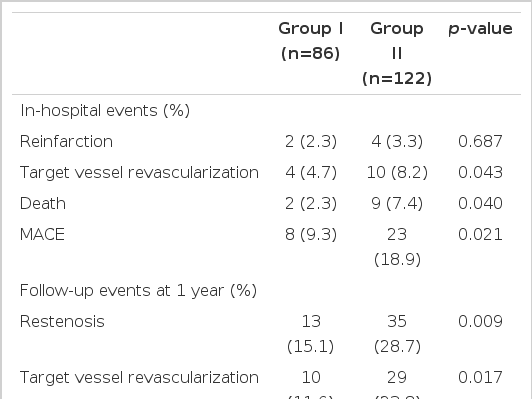
5. Major adverse cardiac events and the long-term survival
The in-hospital death at the time of admission that presented with cardiogenic shock occurred in 2 cases in group I and 7 cases in group II. Major adverse cardiac events were observed in all patients at one, six and twelve months. Restenosis represented a significantly higher occurrence in group II (p=0.009) and the number of cases with target lesion revascularization was higher in group II (p=0.017) (Table 5).
The survival rate was analyzed during the clinical follow-up at 1, 6 and 12 months after the PCI and the survival rate was significantly lower in group II than in group I for each time period (p=0.043, 0.040 and 0.018, respectively) (Table 3).
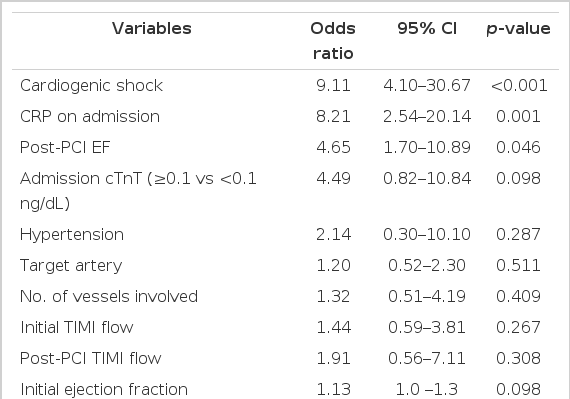
6. Independent predictive factors for the one-year mortality
Multiple logistic regression analysis was performed for the prediction of the one-year mortality after primary or rescue PCI. Cardiogenic shock at the time of admission, a CRP higher than 1 mg/dL and an ejection fraction lower than 40% after the PCI were independent risk factors (p<0.001, 0.001 and 0.043, respectively), whereas cardiac tropanin-T was a strong albeit not independent predictor indicating a one-year mortality. Age, sex, risk factors for atherosclerosis, target lesion location, involved vessel number and TIMI flow grade were not independent risk factors (Table 6).
DISCUSSION
Our study demonstrated that the event-free survival was higher in patients with AMI and high CRP after primary or rescue PCI. The mechanism of the inflammatory reaction in acute myocardial infarction has not been clearly elucidated14), but previous reports suggested that the level of CRP is elevated in patients with acute myocardial infarction and that CRP is an important factor for the prediction of the short-and long-term prognosis in acute myocardial infarction15–18). CRP is produced from liver cells stimulated by cytokines, such as interleukin-6 (IL-6), tumor necrosis factor (TNF)-α and interieukin-1 (IL-1), and these kinds of cytokines are released from activated monocytes/macrophages during ischemic insults in patients with an acute myocardial infarction19). A recent study reported that the concentration of IL-6 was closely related to the level of CRP in an acute myocardial infarction20). Our results suggested that elevated CRP could predict poor prognosis even after successful PCI in patients with AMI.
The level of CRP at the time of admission in patients with an acute myocardial infarction can be used as a useful index for the assessment of the vulnerability of the coronary artery lesion. Tomoda et al.21) reported that a level of CRP greater than 0.3 mg/dL in patients with an acute myocardial infarction was related to the restenosis after the primary PCI, restenosis, recurrent myocardial infarction and cardiac death. In contrast, in the patients with a normal CRP on admission, major adverse cardiac events were demonstrated in less than 5% of the patients.
Our study demonstrated that lower event-free survival at one, six and twelve months after the PCI was observed in patients with a CRP higher than 1 mg/dL. Our preliminary study22) showed that the mean value of CRP was elevated in Asian patients with an acute myocardial infarction. Liuzzo et al.23) reported that the serum concentration of CRP was elevated after PCI in patients with a high CRP, but not so in patients with a normal baseline CRP or in patients with stable angina. Zebrack et al.24) reported that pre-discharge CRP levels are higher after acute myocardial infarction than after unstable angina or stable angina and that CRP is strongly predictive of long-term risk of death or nonfatal acute myocardial infarction for unstable angina or stable angina, but it is not predictive shortly after acute myocardial infarction.
Nikfardjam et al.25) reported that high CRP level was associated with increased 3-year mortality, but there was only a weak and non-significant association between increased serum CRP and the risk of death. Walter et al.26) reported that high CRP level was independently associated with a high risk of adverse coronary events and that restenosis rates were significantly higher in the two upper tertiles compared with CRP levels in the lowest tertiles. Abdelmouttaleb et al.27) analyzed 201 patients who underwent diagnostic coronary angiography, 142 patients with coronary artery stenosis, 37 patients without lesions and 37 controls. The serum level of the CRP was closely related to the acute coronary syndrome. Tomoda et al.21) reported that CRP was the only prognostic factor in patients with an acute myocardial infarction for the prediction of major adverse cardiac events (MACE), such as recurrent myocardial infarction, target lesion revascularization due to restenosis and cardiac death. Anzai et al.28) reported that a peak CRP level of more than 2.0 mg/dL and an age greater than 70 years old were predictive factors for MACE during a one-year clinical follow-up. Giannitsis et al.29) reported that the prognostic factors for long-term cardiac death in patients with an acute myocardial infarction were cardiogenic shock and elderly patients older than 75 year of age.
However, this was a single center study and the major limitation was the sample size of the number of AMI cases that underwent primary or rescue PCI. Further, patients with cardiogenic shock should be divided into a separate group in future studies with a large number of patients.
In conclusion, an elevated CRP is an independent prognostic marker in patients with acute myocardial infarction after primary or rescue PCI.