Perception of Risk of Developing Diabetes in Offspring of Type 2 Diabetic Patients
Article information
Abstract
Background
The risk of developing diabetes is high in the offspring of patients with type 2 diabetes. There have been no studies to assess the offspring’s awareness of the risk of developing diabetes. The aim of this study was to investigate how the male offspring of type 2 diabetic patients assess their likelihood of developing diabetes.
Methods
One hundred and one non-diabetic men with one or both parents having type 2 diabetes, aged 19–28 years, were recruited.
Results
Thirty-nine subjects (38.6%) were concerned about diabetes and 85 (84.2%) considered diabetes a serious problem. However, only 10 (9.9%) thought they might develop diabetes and 9 (8.9%) had previously attended diabetes education programs with their parents. The educational level amongst the diabetic parents was the only independent predictor of perception of the increased risk. Age, body mass index, waist-to-hip ratio, educational level and the perception of diabetes as a serious problem were not associated with perception of the increased risk.
Conclusion
Most offspring of diabetic parents lacked knowledge about the increased risk amongst family members. We suggest that physicians and diabetic educators should provide knowledge about the increased risk of developing diabetes in offspring and the benefit of lifestyle modification to delay or prevent the development of the disease.
INTRODUCTION
Genetic factors are important for the development of type 2 diabetes. Type 2 diabetes is more common in individuals with a family history of diabetes and in members of certain racial/ethnic groups. The risk of diabetes is 2–4 times higher in the offspring of patients with type 2 diabetes than in offspring of parents without diabetes, about one-third of whom will eventually develop abnormal glucose tolerance or frank diabetes1–2).
Diabetes is also a lifestyle disorder3, 4). Diet and exercise habits can modify the development and progression of diabetes. Culture- and community-based primary prevention strategies that target healthy lifestyle behavior are essential to prevention. These are more efficient in high-risk individuals, such as first-degree relatives of diabetes patients, than in the general population.
To achieve the goal of prevention, it is important for high-risk groups to understand the pathogenesis of diabetes. There have been a few reports about the knowledge of genetic risk of diabetes among family members of type 2 diabetic patients5). However, there has been no study that assesses the awareness of the risk of developing diabetes, amongst the offspring of diabetic parents.
The aim of this study was to investigate the level of risk perceived by the offspring of type 2 diabetic patients for developing diabetes.
MATERIALS AND METHODS
Subjects
We surveyed male soldiers in the Korean army visiting the outpatient department of the army hospital for regular routine examinations from December 1, 1999 to February 28, 2000. Clinical profiles, fasting plasma glucose (FPG) level and a questionnaire, including family histories, were obtained.
Among them, 118 healthy soldiers with normal FPG levels and who had one or both parents with type 2 diabetes were recruited. All subjects were aged over 19 years and were able to complete the questionnaires. This study was approved by the Army Ethics Approval Committee.
Methods
Fasting plasma glucose levels were determined immediately after collection by a glucose analyzer (YSI, Yellow Springs, Ohio, USA). Height, weight, waist and hip circumference were measured.
Subjects answered two questionnaires. One contained the social history of the candidates and family history about diabetes. It also contained 1) concern about diabetes, ‘Are you concerned about diabetes?’ ; 2) perception of the seriousness of diabetes, ‘Do you think that diabetes is a serious disease?’ ; and 3) perception of genetic risk, ‘Do you think that you may develop diabetes because your parents have diabetes?’ The other contained five multiple-choice questions selected partially from Diabetic Knowledge Scale Form of a previous publication6) considering the knowledge of the Korean population to measure the knowledge about diabetes (see appendix A).
Statistical analysis
Data were presented as medians or means with SD. Relationship of FPG with other variables were analyzed with Spearman’s rank correlation test. Differences in categorical data were compared using Fisher’s exact test. Multiple logistic regression analysis was used to observe independent factors predictive of perceived risk of diabetes. Differences were considered statistically significant if p<0.05.
RESULTS
Among 118 candidates, 101 subjects completed the questionnaires. The median age was 22 years (range 19–28), mean body mass index (BMI) was 22.1±1.6 kg/m2, mean waist-hip ratio (WHR) was 0.82±0.06 and mean FPG level was 4.33±0.60 mmol/L. When the participants were divided by BMI into three categories (underweight, <20 kg/m2; normal weight, 20–24.9 kg/m2; overweight, 25–29.9 kg/m2), 95.0% were not overweight. Age (r=0.36, p<0.01) and WHR (r=0.31, p<0.01) were significantly correlated with FPG levels.
Thirty-two subjects (31.7%) were attending or had graduated from college or university. Fifty-six subjects (55.4%) had a father with diabetes, 42 subjects (41.6%) had a mother with diabetes and 3 subjects had both parents with diabetes.
Thirty-nine subjects (38.6%) were concerned about diabetes and 85 (84.2%) considered diabetes a serious disease. However, only 11 (10.9%) thought that they might develop diabetes in the future. Nine subjects (8.9%) had an experience of attending a diabetes education program with their diabetic parents. Eighty-six subjects (85.1%) gave correct answers to less than 2 of the 5 diabetes knowledge questions (Table 1).
No clinical and social parameters were associated with perception of increased diabetic risk (Table 2), although a higher educational level amongst the diabetic parents (chi-square=4.0, p<0.05) was associated with perception of increased diabetic risk. Having a father with diabetes showed a borderline significance (chi-square=3.1, p=0.07) (Table 3). Other variables amongst parents that diabetes was a serious problem were not associated with per ception (Table 1, 2, 3). The educational level of diabetic parents was the only independent predictor of perceiving themselves at increased risk of diabetes by multivariate logistic regression analysis (p<0.05).
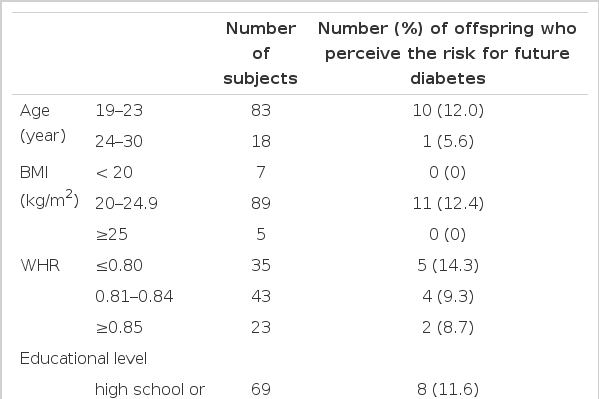
Perception of risk of developing diabetes in offspring of type 2 diabetes patients by clinical and social parameters.
DISCUSSION
This study shows that most young and healthy male offspring of type 2 diabetic parents, one of the high-risk groups of diabetes, do not perceive a strong risk for developing diabetes in the future.
Type 2 diabetes has a complex etiology. Both genetic and environmental factors are involved in the development and progression of the disease. Concordance rates for type 2 diabetes in identical twins are between 70% to 90%. The lifetime risk is up to 40% if one parent has type 2 diabetes1, 2). The American Diabetes Association recommends that screening of high-risk individuals should be considered at a younger age or be carried out more frequently7).
In spite of the importance of genetic background in the development of type 2 diabetes, patients with diabetes and their relatives do not fully understand the risk. Only 35% and 40% of type 2 diabetic patients were aware that their children and siblings, respectively were at an increased risk of developing diabetes8). The studies on the perception of the risk of diabetes in the high-risk group are very rare. Farmer et al. reported that 38% of siblings of type 2 diabetic patients knew the risk5). In this study, only 9.9% of the offspring of diabetic patients were aware of the increased risk of developing diabetes.
There are several possible reasons for the lower rate of perception of the risk in the present study, compared with the previous ones. The subjects of this study were younger than those of the previous studies. So, they might have been not concerned about medical illnesses and have less information about diabetes. Another possible explanation is that the Korean population has less chance to have medical information, compared with people in developed countries. As 84.2% considered diabetes as a serious problem, most of diabetic offspring knew the detrimental sequelae of diabetes through the mass media. However, they lacked proper knowledge about genetic influences of diabetes. Among 11 subjects considering themselves having a higher risk, most were concerned about diabetes (8 subjects) and thought diabetes to be a serious disease (10 subjects). This study is the first study that evaluated the perception of the risk for diabetes in offspring with diabetic parents.
Lifestyle is important for the development of type 2 diabetes in terms of inducing insulin resistance. In a country undergoing “westernization” or modernization, the prevalence of diabetes increases along with the increase of obesity from high calorie intake and lack of exercise. In recent decades, type 2 diabetes has become a major public health problem in Korea10). In 1993, community -based prevalence of diabetes in Yonchon County, Korea, was 7.2% in the population with ages over 30 years. This figure was much higher than previously estimated.
Studies of first-degree relatives of type 2 diabetic patients have suggested the presence of a prediabetic state that was associated with insulin resistance, abdominal obesity and lipid disorders9, 11, 12). The change of lifestyle to reduce insulin resistance can prevent the development of type 2 diabetes13).
Primary prevention costs less than comprehensive care for an overt disease. The effects of population-based primary prevention programs can be maximized in the high-risk group, such as offspring of diabetic parents. So the awareness of the benefit from prevention in the high-risk group is important. However, studies about knowledge of the benefit from prevention strategies in the high-risk group are also rare. In the present study, offspring of diabetic parents had poor information about the diabetes. We suggest that an effort to educate the high-risk group is needed. We also think it is necessary to introduce the offspring of diabetic patients to a diabetic education program regularly with their parents to recognize their increased risk of developing diabetes and to modify their lifestyle.
We expected that several factors in the offspring, such as educational level, were associated with a better understanding of the risk for diabetes. However, none was significant. Only the educational level of diabetic parents predicted a better awareness of the possibility to develop diabetes by the offspring. This finding implies the importance of obtaining information from acquaintance and comprehensive education of diabetic parents is necessary, including the need to educate their offspring.
There are some limitations in the present study. Because of low representation of the risk perception group, this study lacks the power to completely analyze the factors influencing the perception of the increased risk for diabetes. A study with a larger number of subjects is needed. Another possible limitation is the adequacy of the questionnaire about the knowledge of diabetes. As mentioned previously, 5 questions were selected partially from Diabetic Knowledge Scale Form of a previous publication6) considering the knowledge of the Korean population. We do not have data to validate the questionnaire. Further study with an adequate questionnaire may be needed.
In summary, most of the offspring of type 2 diabetic parents, the important high-risk group, do not have proper knowledge of genetic effects of diabetes and medical information about the disease. We suggest that physicians and diabetic educators should provide knowledge about the increased risk of developing diabetes, emphasizing the need for lifestyle modification to delay or prevent the development and for early detection of diabetes.
Acknowledgments
The authors acknowledge the assistance of the Korea Special Warfare Command in Seoul for subjects recruitment.
Appendices
Appendix A. Diabetic knowledge questionnaire (Q1–Q5)
Q1 People with diabetes should:
have their food cooked separately from that of the family.
eat the same foods.
vary their diet by substituting different foods from the food exchange list.
I don’t know.
Q2 Which one of the following symptoms is not usually associated with hypoglycemia?
weakness
hunger
chest pain
I don’t know
Q3 Diabetic patient can eat as much as he/she likes of which one of the following foods?
fruit
lettuce
steak
honey
I don’t know
Q4 You must avoid becoming overweight if you have diabetes because:
insulin can be harmful to overweight people.
overweight deteriorates diabetes.
hypoglycemia attacks occur more frequently in
I don’t know.
Q5 Which one or more of the followings are false?
Diabetes is diagnosed by the presence of glucose in the urine.
Diabetic eye complication is common.
If diabetic patient is not having symptoms, it is good.
I don’t know

