Non-Hodgkin’s Lymphoma of the Thyroid and Adrenal Glands
Article information
Abstract
We report a case of non-Hodgkin’s lymphoma(NHL) with simultaneous involvement of both thyroid and bilateral adrenal glands. Literature review on a computerized search showed that this is an extremely rare condition. The final diagnosis of diffuse large B cell lymphoma was confirmed by biopsies of thyroid gland, enlarged cervical lymph node, and adrenal gland. The significant endocrine dysfunction of the thyroid, adrenal or other endocrine glands was absent in our case. The patient responded dramatically to three cycles of chemotherapy with no complication or endocrine dysfunction and continues to be followed.
INTRODUCTION
Primary extranodal lymphoma frequently involves the gastrointestinal tract, Waldeyer’s ring, and the brain, and accounts for 31.5–41% of all non-Hodgkin’s lymphoma (NHL). The prevalence of the thyroid involvement in lymphoma is about 2.5–3% of patients with NHL and most of the involvements occurred in the gland of Hashimoto’s thyroiditis1). It has been reported that primary malignant lymphoma accounts for approximately 5% of all thyroid malignancies2). Though secondary involvement of the adrenal gland with NHL occurs relatively frequently, primary adrenal lymphoma is extremely rare3).
We report a patient with NHL presenting with simultaneous involvement of two rare extranodal sites -thyroid and adrenal- without significant endocrine dysfunction.
CASE
A 76-year-old female patient presented with a three month history of anterior neck swelling that was rapidly progressing during the last two weeks. There was no history of thyroid disease or previous malignancy. Her physician detected hypertension several years ago, but the patient took no specific medication. The patient’s family history was noncontributory. She had a 20 pack-year smoking history and drank alcohol occasionally. The patient denied fever or night sweats but had lost 6 Kg of weight during the past three months.
Physical examination showed a chronically ill-appearing woman. On examination of the neck, both lobes of the thyroid gland were diffusely enlarged with hard consistency and were relatively fixed. Multiple bean-sized, movable lymph nodes were palpable along the anterior margins of the mid-portion of both sternocleidomastoid muscles. The abdomen was nontender and nondistended, and no mass or organomegaly was found.
Her blood pressure was 130/80 mmHg: pulse rate was 78 beats per minute, and her body temperature was 36.0 °C. Laboratory blood tests showed a white blood cell count of 5800/mm3 with normal differential count: hemoglobin 11.5g/dL, hematocrit 33.6% and platelet 152,000/mm3. Data of blood chemistry were as follows: total protein 5.9g/dL, albumin 3.2g/dL, lactic dehydrogenase 373U/L (normal range 120–240 U/L), ESR 40mm/hr normal range 0–30mm/hr), aspartate amino-transferase 18U/L normal range 0–35 U/L), uric acid 107 μmol/L (normal range 90–360 μmol/L), alkaline phosphatase 78U/L (normal range 30–120U/L). There was no specific abnormality of other laboratory tests. Anti-microsomal and antithyroglobulin antibodies were negative. Thyroid function tests were as follows: free T4 21.8 pmol/L (normal range 9.0–43.76 pmol/L), TSH 0.51 mU/L (normal range 0.4–5 mU/L), and thyroglobulin 630 ng/mL (normal range 2–60 ng/mL).
Thyroid US demonstrated a diffusely enlarged thyroid gland, diffuse irregular hypoechoic lesions on the left lobe and multiple irregularly scattered hypoechoic lesions on the upper part of the right lobe. There were also multiple hypoechoic enlarged lymph nodes of 1–1.2 cm size on both sides of the neck. 99mTc pertechnetate scan demonstrated markedly decreased and heterogeneous uptake on the ultrasonographically abnormal area and showed normal uptake on the right lower pole (Figure 1A). 99mTc-hexakis-2-methoxy isobutyl isonitrile (MIBI) scan showed significant uptake in the abnormal area on the 10-minute image with normal washout on the right lower pole (Figure 1B), and significant retention of isotope on 4-hour-delayed image (Figure 1C). Fine-needle aspiration of the thyroid mass was indeterminate, but a cytologist suggested the probability of undifferentiated malignancy. Computerized tomographic (CT) scan of the neck showed diffuse enlargement of both thyroid lobes with more marked enlargement in the left lobe. Focal areas of normal enhancement were present in both lobes. However, other abnormal areas showed decreased density with lobulated margins. There were also multiple lymphadenopathies in both internal jugular chains (Figure 2).

Radionuclide studies of the thyroid gland. 99mTc pertechnetate scan demonstrates markedly decreased and heterogeneous uptake in both thyroid lobes, except the right lower pole(A). 99mTc-MIBI scan shows significant uptake in both thyroid lobes on the 10-minute image with normal washout on the right lower pole(B), and significant retention of isotope on the 4-hour-delayed image(C).

Contrast enhanced CT scan of the thyroid shows a diffuse goiter with decreased density and focal areas of normal enhancement.
Chest radiology was normal, but abdominal US demonstrated large bilateral adrenal masses of homogeneous hypoechoic texture. Abdominal CT scan showed large bilateral masses in the region of the adrenal glands. The mass on the right measured 6×4×6.5 cm, and the mass on the left measured 10×6×10.5 cm. The masses were of homogeneous low attenuation. There was no evidence of abdominal or pelvic lymphadenopathy (Figure 3).

Abdominal CT scan reveals large bilateral masses of low attenuation in the region of the adrenal glands without involvement of other areas
Ultrasound-guided core needle biopsies of the left thyroid lobe and of the adrenal mass on the left side were done and incisional biopsy of the palpable lymph node on the left jugular chain was performed. All of them showed diffuse lesions consisting of large, oval to round monomorphic cells with scant cytoplasm. Most cells had a single nucleolus with finely stippled chromatin. Marker study of tumor cells revealed B cell origin with a final diagnosis of diffuse large B cell lymphoma (Figure 4). Peripheral blood smear and bone marrow biopsy were normal. Brain MRI revealed a multifocal lacunar infarction of left basal ganglia. Echocardiography was nonspecific.

Biopsy of the left lobe of the thyroid gland showing diffuse lesions consisting of large, oval to round monomorphic cells with finely stippled chromatin. Most cells had a single nucleolus.
Other endocrine tests were done: plasma ACTH 15.3 pmol/L (normal range 2–11 pmol/L), cortisol 416.6 nmol/L (normal range 140–690 nmol/L), and her serum calcitonin, plasma renin activity, aldosterone, urinary vanillylmandelic acid and metanephrine were all within normal ranges.
She received CHOP regimen (cyclophosphamide 750 mg/m2, doxorubicin 50 mg/m2, and vincristine 1.4 mg/m2 intravenously on the first day, and prednisone 100 mg/m2 orally for five days). On the fifth day of first chemotherapy, her goiter was found to be markedly reduced. Gallium scintigraphy done one day after the first cycle of chemotherapy revealed no uptake of radiotracer in the region of the tumors (Figure 5). Before receiving a second cycle of chemotherapy, thyroid function test and one-hour standard ACTH stimulation test were normal: free T4 12.6 pmol/L (normal range 9.0–43.76 pmol/L), TSH 0.4 mU/L (normal range 0.4–5 mU/L), basal plasma ACTH 8.76 pmol/L (normal range 2–11 pmol/L), basal serum cortisol 532.5 nmol/L (normal range 140–690 nmol/L), and serum cortisol 684.2 pmol/L 60 min after intravenous injection of 250 ug (85 nmol) of Cosyntropin. Abdominal US revealed no mass in the regions of both adrenal glands.
DISCUSSION
The most common presentation of thyroid lymphoma is a rapidly enlarging neck mass, as in our case. Thyroid dysfunction caused by involvement of NHL is seen in 7–59% of patients and most of them have evidence of Hashimoto’s thyroiditis4,5). Our patient showed no evidence of thyroid dysfunction or Hashimoto’s thyroiditis. Aozasa et al.6) reported that tests for the serum antithyroid antibodies were positive in 83% of the patients with thyroid lymphoma in Japan. Moreover, Hashimoto’s thyroiditis should be considered in the differential diagnosis with thyroid lymphoma. Features that might point to a diagnosis of lymphoma, rather than thyroiditis, are the rapidity of growth of the goiter (40% of patients with lymphoma had symptoms for less than 1 month) and the older age of the patient (Hashimoto’s thyroiditis is more common in the 30′s to 50′s). As noted above, hoarseness and vocal cord paralysis are also more likely to be associated with malignancy than thyroiditis7).
Fine-needle biopsy is the initial procedure of choice in the histologic diagnosis of the thyroid tumor, including lymphoma. The yield of this procedure was reported to be high. However, about 10 % of specimens from thyroid lymphoma could be misclassified as undifferentiated carcinoma8). Considering the above, one should proceed to a more aggressive procedure to establish a definitive diagnosis when clinical findings are inconsistent with the fine-needle biopsy.
It has been reported that secondary adrenal tumors can be seen rather frequently, and secondary involvement of the adrenal gland has been reported to occur in as many as 25% of the patients with NHL at autopsy3). Primary adrenal lymphoma, however, is extremely rare9). There have been a few reports of adrenal insufficiency due to bilateral adrenal lymphoma10), but in our patient there was only a slight elevation of plasma ACTH, despite massive bilateral involvement. On the follow-up examination, adrenal function was convinced to be normal by one-hour standard ACTH stimulation test before the second cycle of chemotherapy.
Many reports have described the uses of 99mTc-MIBI in benign and malignant tumors of various sites, which may be useful in the initial assessment of lymphoma and in monitoring tumor response to treatment11). In our case, 99mTc-MIBI scan showed significant uptake that might foretell good response to chemotherapy. The region of decreased uptake on 99mTc pertechnetate scan matched the area of increased uptake on 99mTc-MIBI scan.
Gallium-67-citrate, known for its avidity for lymphoma cells, is often used in detecting and staging lymphoma, and evaluating the treatment response of lymphomas, including thyroid lymphoma12,13). Interestingly, one day after the first cycle of chemotherapy, gallium scintigraphy revealed absent uptake of radiotracer in the region of the tumors.
As for the primary site, we thought that it was the thyroid gland. In general, malignant lymphoma of the thyroid invades locally until most or all of the gland is eventually replaced by a tumor. At that stage, direct extension into surrounding tissue or regional lymph nodes occurs14). In our case, there were multiple lymphadenopathies in bilateral jugular chains, and the involvement of NHL was confirmed by biopsy. There was no evidence of extension beyond the adrenal glands, but simultaneous development could not be ruled out.
To the best of our knowledge, there have been only a few cases with simultaneous involvement of the thyroid and adrenal gland by extranodal NHL. Table I summarizes the clinical, laboratory and pathological data of three reports that could be found on a computerized literature search. Baskal et al.15) reported the first patient whose initial clinical manifestation was symptoms of adrenal insufficiency due to involvement of both adrenal and thyroid glands by high grade immunoblastic lymphoma. After the third course of chemotherapy, his ACTH level normalized. Erdogan et al.16) reported such a case with minor pelvic nodal involvement. Their case was B-cell type of immunoblastic lymphoma. More recently Nasu et al.14) reported a rare case of NHL (diffuse large cell, B cell type) presenting with adrenal insufficiency and hypothyroidism but their case was found to have brain metastasis and died of pneumonia. In the second and third case reports, the adrenal glands seemed to be primary sites, because the second patient had the evidence of lymph node involvement in the pelvis, and the third showed massive involvement of both adrenal glands with a focal thyroid lesion.
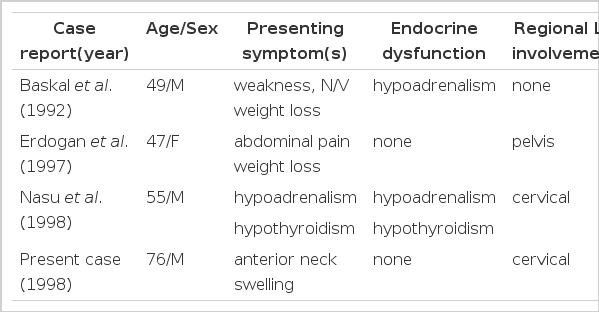
Case reports on simultaneous involvement of the thyroid and adrenal glands by non-Hodgkin’s lymphoma.
In conclusion, simultaneous involvement of the thyroid and adrenal glands with NHL is very rare. Adrenal gland involvement should be ruled out, however, during the stating of thyroid lymphoma, especially in patients with symptoms or signs suggesting hypoadrenalism.
