Urinary Bladder Involvement in Patients with Systemic Lupus Erythematosus: with Review of the Literature
Article information
Abstract
Objectives
To investigate the etiologies of urinary bladder involvement in patients with systemic lupus erythematosus (SLE), the clinicoradiologic features of gastrointestinal tract manifestations and clinical outcomes in patients with lupus cystitis accompanied by gastrointestinal manifestations.
Methods
We conducted a retrospective chart review on 413 patients with SLE. Patients were selected for review on the basis of tower urinary tract symptoms including urinary frequency, urgency and urinary incontinence. Radiologic studies were analyzed in patients with lupus cystitis.
Results
Ten consecutive patients, complicated with lower urinary tract symptoms, were identified. Underlying etiologies were as follows: lupus cystitis in five, neurogenic dysfunction secondary to transverse myelitis in three, cyclophosphamide-induced cystitis in one and tuberculous cystitis in one patient. All patients with lupus cystitis showed gastrointestinal manifestations, such as abdominal pain, nausea, vomiting and/or diarrhea during the periods of cystitis symptoms. In all patients with lupus cystitis, paralytic ileus was demonstrated on plain abdominal X-ray and ascites, bilateral hydroureteronephrosis and thickened bladder wall were identified on abdominal ultrasound or CT. Abdominal CT revealed bowel wall thickening in four of the five patients. The main sites of thickened bowel on abdominal CT were territory supplied by superior mesenteric artery. Two of five patients with lupus cystitis expired during the follow-up period.
Conclusion
Diverse etiologies may cause lower urinary tract symptoms in patients with SLE. Lupus cystitis is strongly associated with gastrointestinal involvement and abdominal CT can be a useful radiologic tool to investigate the gastrointestinal tract involvement in patients with lupus cystitis.
INTRODUCTION
Systemic lupus erythematosus (SLE) is an autoimmune disease characterized by the production of autoantibodies in association with various clinical manifestations. Urinary bladder involvement in SLE is an uncommon but important manifestation. Lupus cystitis, neurogenic dysfunction secondary to transverse myelopathy, cyclophosphamide administration, inflammatory polyneuropathy and infections are known to be related to bladder dysfunction in patients with SLE1). Chronic interstitial cystitis is a chronic inflammation of the bladder wall, in which numerous autoimmune mechanisms are thought to be involved in the pathogenesis. After interstitial cystitis related to SLE was named ‘lupus cystitis’ by Orth, et al., at least 39 total patients with lupus cystitis have been described in more than 27 reports2–28) and it has been suggested that intestinal tract is frequently associated with lupus cystitis29). However, data regarding clinical and radiologic features of gastrointestinal tract involvement in lupus cystitis are limited. The pathogenesis of lupus cystitis and associated gastrointestinal abnormalities has not been fully explained, but immune complex-mediated vasculitis has been suggested22). Abdomen computed tomography (CT) was suggested to be useful in the diagnosis and follow-up evaluation of lupus vasculitis of the intestinal tract and urinary bladder18). Few reports described CT findings of the gastrointestinal tract in lupus cystitis patients complicated with gastrointestinal manifestations10,14–15,18–19). As for treatment of lupus cystitis, early diagnosis and corticosteroid administration has been emphasized29). Cyclophosphamide is widely used for malignancy, and it has had an increasing role in the treatment of non-neoplastic diseases such as SLE, rheumatoid arthritis and Wegener’s granulomatosis. Cyclophosphamide may cause urological side effects, from transient irritative voiding symptoms to life-threatening hemorrhagic cystitis, which were a major limiting factor in cyclophosphamide use30). The incidence of tuberculous infection in SLE is much higher than in the general population31). SLE associated tuberculosis often include miliary and far-advanced pulmonary and extrapulmonary forms. Urogenital tuberculosis has been rarely reported in SLE patients31). Acute transverse myelopathy (ATM), which is a rare manifestation of SLE, can cause sphincter disturbances. A satisfactory outcome may be obtained by early aggressive combination therapy with corticosteroid and cytotoxic agents32).
We described ten lupus patients accompanied by urinary bladder involvement, including clinical manifestations and radiologic findings of gastrointestinal tract involvement in patients with lupus cystitis, along with a review of the literature.
MATERIALS AND METHODS
We conducted a retrospective chart review on all patients with SLE who were admitted to Kangnam St. Mary’s Hospital from January 1990 to June 1998. Patients were selected for review on the basis of lower urinary tract symptoms, including urinary frequency, urgency or urinary incontinence. Patients with bacterial cystitis or pyelonephritis were excluded. All patients fulfilled the revised criteria for the classification of SLE of the American College of Rheumatology33). Lupus cystitis was diagnosed on the basis of clinical presentations and findings of radiologic studies, cystoscopy or bladder biopsy. Patients with lupus cystitis were evaluated for gastrointestinal manifestations (abdominal pain, nausea, vomiting, diarrhea), clinical outcomes, and radiologic findings of abdominal plain radiograph, small bowel follow through, abdominal ultrasound or abdominal CT. Abdominal ultrasound and CT were performed for all patients with lupus cystitis, who were analyzed for the presence of ascites, bowel or bladder wall thickening, hydronephrosis, hydroureter, sites of bowel involvement and CT comb sign by two experienced radiologists. We defined bladder and bowel wall thickening when the thickness exceeded 3 mm measured by abdominal US or CT. The presumptive diagnosis of mesenteric vasculitis was made by the clinical symptoms of abdominal pain, ascites, the presence of target sign and CT comb sign on abdominal CT which were suggested by Ko SF et al34). Transverse myelopathy was diagnosed when a patient presented with spinal cord dysfunction giving rise to motor, sensory or sphincter disturbance in the absence of structural abnormal lesions, such as tumors, hematomas and collapsed vertebral bodies. The diagnosis of cyclophosphamide-induced cystitis was made by irritative voiding symptoms and hematuria with a previous history of cyclophosphamide therapy. Tuberculous cystitis was confirmed by positive urine AFB smear and culture, with cystoscopic and radiolgic findings of the urinary biadder.
RESULTS
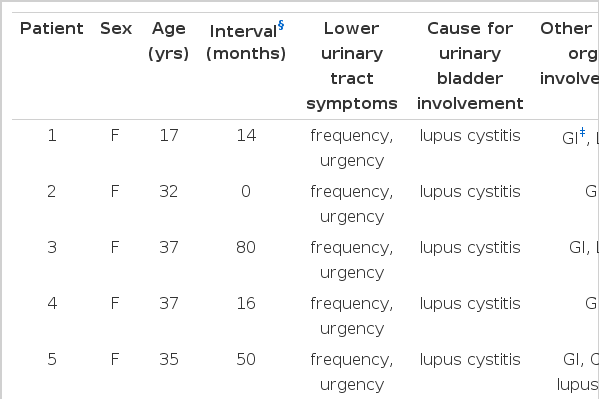
A total of 413 charts were reviewed. Ten consecutive patients, complicated with lower urinary tract symptoms were identified. Table 1 shows demographic and clinical features of the patients included in our study. Underlying etiologies for lower urinary tract involvement were as follows: lupus cystitis in five (5/413, 1.2%), neurogenic dysfunction secondary to acute transverse myelopathy (ATM) in three (3/413, 0.7%), cyclophosphamide-induced cystitis in one and tuberculous cystitis in one. All patients were woman aged 17-46 years (average 30.2 years). In one of the five patients with lupus cystitis, lupus cystitis was the initial manifestation of the lupus. The mean interval between the diagnosis of SLE and the occurrence of lupus cystitis in the remaining 4 patients and acute transverse myelopathy were 40 months (range 14-80) and 54 months (range 39–74), respectively. Cystoscopic examination and biopsy were performed in three of five patients (patients 3,4,5). Findings of small bladder capacity and inflammatory mucosa were observed by cystoscopic exams in each case. The biopsies of the bladder in these patients showed findings of inflammatory cell infiltration with edema and hypervascularity. Although pathologic examinations of the bladder were not performed in patients 1 and 2, diagnosis of lupus cystitis was made on the basis of the following clinical features; lower tract urinary tract symptoms, radiologic findings, good response to steroid administration, no history of cyclophosphamide or radiation therapy, negative urine AFB culture and smear. Malignancy was ruled out by clinical follow-up. Two of the three patients with ATM had lumbar cord lesions and the remaining one patient had thoracic cord lesion. Magnetic resonance imaging of the affected spinal cord showed no abnormal findings. Electromyographic exam was performed in all three patients and showed conduction defect in the corresponding spinal cord level. Cerebrospinal fluid studies of three patients revealed increase in protein with decreased sugar. Patient 9 had been treated with 75 milligrams of oral cyclophosphamide a day to manage lupus nephritis for approximately two years. Bilateral hydroureteronephrosis, mucosal irregularity and bladder contraction were observed on excretory urogram and CT. Her cystoscopic exam revealed a reduction in bladder size and some patchy areas of erythema. Cystoscopic bladder biopsy specimen in this patient showed extensive urothelial changes and fibrosis of the lamina propria. Urine AFB smear and culture were done in all ten patients. Only one patient (patient 10) had positive results of urine AFB smear and culture. Cystoscopic exam in this patient revealed reduced bladder size and red and edematous mucosa, especially around the ureteric orifice. Intravenous urogram showed a small irregular bladder, narrowing of both distal ureters and bilateral hydroureteronephrosis. Thickened urinary bladder wall and bilateral hydroureteronephrosis were also demonstrated in CT. There was no evidence of pulmonary and any other site of mycobacterium tuberculosis infection in this patient. Gastrointestinal manifestations concurrently occurred in all patients with lupus cystitis. Six of the ten patients had lupus nephritis, three of five patients with lupus cystitis (patients 1,3,5), one of three patients with acute transverse myelopathy, one patient with cyclophosphamide-induced cystitis and one patient with tuberculous cystitis. A central nervous system vasculitis was demonstrated in one patient with lupus cystitis (patient 5) during admission. The decreased level of C3 or C4 was observed in eight of ten patients; in all of five patients with lupus cystitis, two of three patients with ATM and one patient with cyclophosphamide-induced cystitis. Anti-ds DNA antibody was positive in one of five patients with lupus cystitis (patient 3) and in a patient with cyclophosphamide-induced cystitis. Bladder wall thickening on CT was observed in all patients with lupus cystitis, cyclophosphamide induced cystitis and tuberculous cystitis.
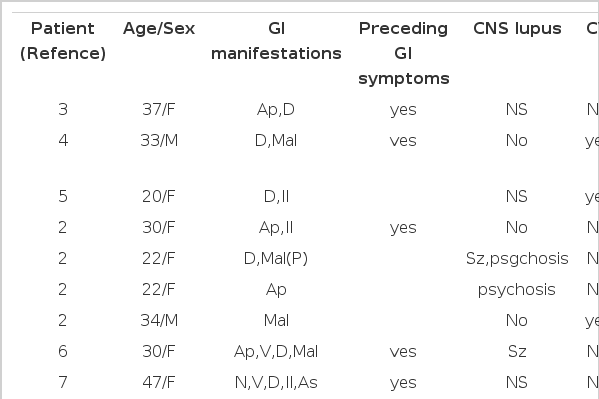
Table 2 demonstrates the clinical features of gastrointestinal tract involvements in reported patients with lupus cystitis, including our five cases. Gastrointestinal manifestations, such as abdominal pain (n = 5), vomiting (n = 5), nausea (n = 3) and diarrhea (n = 3) were observed during the periods of lupus cystitis. On physical examination, rebound tenderness was observed in all patients except one (patients 5). All our five patients had a preceding history of gastrointestinal manifestations before the onset of lupus cystitis. Two patients (patient 1,5) had recurrent episodes of mesenteric vasculitis which was diagnosed on the basis of diagnostic criteria suggested by Ko SF et al. The number of episodes of mesenteric vasculitis in patient 1 and 5 were 2 and 6, respectively. Intestinal biopsy was done in two patients (patients 3,4) in whom no evidence of vasculitis was found. As for treatment of lupus cystitis, four patients (patients 1,2,3,5) were given intravenous methylprednisolone (1mg/kg/day) until satisfactory clinical improvements were accomplished, then followed by oral prednisolone. Within 14 days of steroid therapy, gastrointestinal and lower urinary tract symptoms were markedly improved in three patients (patients 1,2,3). In patient 5, gastrointestinal symptoms did respond well to steroids, but her genitourinary tract symptoms were not markedly improved. Cyclophosphamide pulse therapy (500 mg /day) for a day and bilateral percutaneous nephrostomy were also performed on this patient. A patient (patient 4) recovered without steroid or immune suppressive agents.
Two of the five patients with lupus cystitis died. One patient (patient 5) expired during admission because of CNS vasculitis. The other patient (patient 4) expired secondary to pulmonary hemorrhage two years later. During follow-up, three live patients had no recurrence of lower urinary tract involvement. Duration of follow-up period in these patients was 50 months, 27 months and 32 months, respectively.
Radiologic findings in our five patients with lupus cystitis and previously reported cases are shown in Table 3. Abdominal plain radiograph showed paralytic ileus in all patients and ascites in three of five patients (patients 2,3,5). Small bowel follow-through was checked in one patient (patient 2) which revealed a thumbprinting appearance of the duodenal third portion and ascending colon. Abdominal ultrasound was and CT disclosed both ascites and bilateral hydroureteronephrosis in all patients. Abdominal ultrasound showed thickened small bowel wall in one patient (patient 3) and thickened bladder wall in one patient (patient 5). Follow-up abdominal ultrasound was done in three of five patients (patients 2,4,5) and revealed no abnormality in patients 2 and 4, and little interval change in case 5. The interval between initial and follow-up exam in patients 2, 4, and 5 were 32, 14 and 10 days, respectively. Bladder wall thickening was identified in all five patients with lupus cystitis on abdominal CT. Bowel wall thickening was observed in four of the five patients (patients 1,2,3,4). Target sign was identified in three of five patients (patients 1,2,4). Two of the five patients disclosed CT comb sign (patients 1,2). The main sites of thickened bowel wall on abdomen CT were as follows; duodenum and jejunum in three (patients 1,2,3), ileum in four (patients 1,2,3,4), ascending colon in three (patients 1,2,4) and transverse, descending and rectosigmoid colon in one patient (patient 2). Follow-up CT during admission was made in two of five patients (patients 4,5). The interval between initial and follow-up CT exam in these patients was 20 and 26 das, respectively. The resolutions of thickened bladder and bowel wall and hydroureteronephrosis were demonstrated in one patient (patient 4). But there was little interval change on follow-up CT in the other patient (patient 5). In patient 3, eight months later she was readmitted because of dyspnea. She had no gastrointestinal and lower urinary tract manifestations. Abdominal CT performed at that time showed no abnormality.
DISCUSSION
Systemic lupus erythematosus can affect every organ system, and lower urinary tract diseases have been known to be rare complications of SLE. The 1.2% prevalence of lupus cystitis in our study is similar to that in a report described by Koike et al.29), but it may be overlooked because patients with lupus cystitis often have concurrent systemic manifestations35). The pathogenesis of lupus cystitis has not been documented, but immune complex mediated vascular injury or abnormal cytokine production and cellular activation in the bladder were suggested as an underlying mechanism of lupus cystitis25). The combination of gastrointestinal symptoms and lupus cystitis seems unique to patients with SLE. About thirty nine cases of lupus cystitis including our five patients have been reported in the literature. Twenty nine patients in these cases (78.4%) had concurrent gastrointestinal tract manifestations. As in our patients (patients 1,2,3,5), gastrointestinal symptoms preceded the onset of lupus cystitis in about half of the patients with lupus cystitis which was accompanied by gastrointestinal involvement. Two reported cases had the history of gastrointestinal tract involvement, and cystitis occurred later without gastrointestinal manifestations20–21). The associated gastrointestinal manifestations in reported patients with lupus cystitis were similar to those in our study; diarrhea (17/24, 70.8%), vomiting (11/24, 45.8%), abdominal pain (10/24, 41.7%), ascites (7/24, 29.2%), ileus (7/24, 29.2%), nausea (6/24, 25.0%), malabsorption (4/24, 16.7%) and protein losing enteropathy (1/24, 4.2%). Studies for malabsorption or protein-losing enteropathy were not performed in our patients. Biopsy findings of intestinal tract have been reported in six patients with lupus cystitis, and evidence for vasculitis on light microscopic exam was found in three of the six patients4,8,10,13,18,20). Tissue deposition of immune complexes or complements have been reported in the gastrointestinal wall, as well as in bladder wall, which suggests that common autoantigen of both urinary bladder and gastrointestinal tract might play an important pathologic role4,8). In our study, intestinal biopsy was performed in two patients (patients 3,4), in whom no evidence of vasculitis was found on light microscope. Orth et al.2) suggested that the central nervous system was frequently associated with lupus cystitis. About eight lupus cystitis patients with CNS symptoms have been reported in the literature, and seizure was the most common manifestation (5/8, 62.5 %). In our study, two patients were related to CNS involvement. One (patient 5) had seizure during the episode of lupus cystitis, the other (patient 3) had a history of seizure related to SLE. Although vasculitis has been considered to be the most possible cause for CNS manifestations in patients with lupus cystitis, no definite evidence for vasculitis has been described in the reported cases. Brain MRI in patient 5 demonstrated findings of vasculitis, and this might be the first case showing evidence of CNS involvement secondary to vasculitis in lupus cystitis patients. Orth et al.2) also suggested that SLE patients with histologic bladder changes were found to have pulmonary hemorrhage more frequently than those without. But no additional case of pulmonary hemorrhage has been reported, except our one patient (patient 4). The association between lupus cystitis and major organ involvement in which vasculitis is thought to be the underlying pathogenesis was disproved by some reports26,29). In contrast to idiopathic interstitial cystitis, lupus cystitis is reported to be frequently associated with hydroureteronephrosis, which is usually due to fibrosis of the ureterovesical junction or detrusor muscle spasm resulting in vesicoureteral reflux2). Bilateral hydroureteronephrosis was observed in all lupus cystitis patients presenting with gastrointestinal manifestations, including our five patients. Interestingly, eight reported cases of lupus cystitis, who showed no gastrointestinal tract involvement, did not have hydroureteronephrosis. All patients with lupus cystitis accompanied by gastrointestinal tract involvement, except two patients (patient 6, our patient 4), were treated with steroids. An initial dose of 40 mg–60 mg of prednisolone was given to most patients. Steroid pulse therapy was performed in seven patients. Seven patients, including our one patient (patient 5), underwent intravenous cyclophosphamide pulse therapy. Gastrointestinal symptoms improved in all patients, except two patients in whom intestinal perforation occurred. The reason why symptoms of lower urinary tract and gastrointestinal tract improved without steroid therapy or immune suppressive drugs was not clear in our patient 3. A case of spontaneous remission of contracted bladder and hydroureteronephrosis with generalized autoimmune phenomenon was previously reported37). According to the report by Koike et al.29) the prognosis of urinary bladder function in patients with lupus cystitis was closely related to the period from the appearance of the symptoms to the initiation of steroid therapy. Ten patients with lupus cystitis complicated by gastrointestinal tract involvement, including our two cases, have been reported to be dead. However, patients with only cystitis were alive. The causes for death were as follows; infection in three, disseminated intravascular coagulation related to intestinal perforation in one, intestinal bleeding with uremia in one, intracranial hemorrhage in one, CNS vasculitis in one, pulmonary hemorrhage in one, and not determined etiology in two patients. Our patient 4 died two years later because of pulmonary hemorrhage.
Table 3 shows radiologic findings in patients with lupus cystitis presenting with gastrointestinal manifestation in reported cases and in our study. Small bowel follow-through or barium enema demonstrated thickened mucosal folds of the bowel wall and a thumbprinting appearance suggesting acute bowel ischemia in four patients, including our one patient (patient 2)3,4,10). Abdominal ultrasound can be useful for the evaluation of gastrointestinal tract involvement in lupus patients accompanied by intestnal vasculitis37). Bowel wall thickening was demonstrated by abdominal ultrasound in one of five patients in our study (patient 3), and it was reversed on follow-up examination. Abdominal CT is a helpful radiologic tool for the evaluation of the gastrointestinal tract. CT findings of gastrointestinal tracts in patients with lupus cystitis presenting with abdominal symptoms have been rarely reported14,15,18,19). Ascites and thickening of the bowel wall were common findings, which were in accordance with our results. These CT findings can be found in many conditions, such as ischemic colitis secondary to vasculitis, shock, mesenteric vascular thrombosis, inflammatory bowel disease, infectious colitis, radiation enteritis and bowel edema associated with portal hypertension38). In our study, two patients (patients 1,2) met diagnostic criteria for lupus mesenteric vasculitis suggested by Ko S. et al34). Although CT comb sign was not demonstrated in two patients (cases 3,4), mesenteric vasculitis was considered the most possible cause for gastrointestinal manifestations. This result may be explained by the fact that this exam was performed after GI symptoms had improved. The interval between the onset of symptoms of cystitis with gastrointestinal manifestations and abdominal CT exam in patients 3 and 4 were 3 months and 2 months, respectively. Any parts of the gastrointestinal tract may be involved in SLE. Interestingly, the bowels supplied by the superior mesenteric artery were preferentially involved in our study. These observations are in accordance with the findings of Ko SF et al34). There has been four reports of lupus cystits showing reversible thickening of the bowel and urinary bladder wall on follow-up CT14,15,18,19). In our study, follow-up CT was performed in 2 patients (patients 3,4) and abnormal radiologic findings of bowel and bladder were reversed in these patients. Acute peritonitis was considered as a most possible cause for the abdominal pain in patient 5 on the basis of radiologic findings and clinical manifestations. Peritoneal inflammation, which is presumably due to deposition of immune complexes in the mesenteric vessels, can result in abdominal pain and ascites. Ascites examination were performed in two patients (patients 3,5), which revealed an exudative effusion with few white blood cells that was sterile when cultured. Although paralytic ileus observed in our patients on abdominal X-ray was a nonspecific findings, it was thought to be associated with ischemic bowel disease. This was supported by the findings of abdominal ultrasound or CT.
In conclusion, our study suggests that bladder abnormality can be caused by diverse etiologies, such as lupus cystitis, cyclophosphamide-induced cystitis, tuberculosis infection and neurogenic bladder secondary to transverse myelopathy. Lupus cystitis must be considered in the differential diagnosis of patients with SLE presenting with gastrointestinal symptoms of unknown causes and lower urinary tract symptoms. Gastrointestinal manifestations in patients with cystitis varies from mild symptoms to severe complications, such as intestinal hemorrhage or perforation which might lead to death. Therefore, early recognition of gastrointestinal involvement in patients with lupus cystitis must be made by radiologic studies as well as by clinical symptoms, and adequate treatment must be initiated.