Duodenal Mucosa-Associated Lymphoid Tissue Lymphoma: A Case Report
Article information
Abstract
Primary duodenal mucosa associated lymphoid tissue (MALT) lymphoma is very rare, and little is known about its clinical course or effective treatment. We describe a case of primary duodenal MALT lymphoma that was resistant to Helicobacter pylori (H. pylori) eradication and regressed after chemotherapy with cyclophosphamide, vincristine, and prednisolone (CVP). A 71-year-old woman was referred to our department because of epigastric pain and dyspepsia. Gastroduodenoscopy revealed an irregular mucosal nodular lesion with ulceration extending from the bulb to the second portion of the duodenum. Histopathological examination of a biopsy specimen disclosed low-grade MALT lymphoma composed of atypical lymphoid cells with lymphoepithelial lesion. Abdominal CT scans revealed 0.5 to 1.5 cm lymph nodes in the peritoneal cavity, suggestive of lymph node metastasis. We successfully eradicated H. pylori but did not see signs of remission. We administered systemic CVP chemotherapy every 3 weeks. After 6 courses of CVP, the patient achieved complete remission and was followed up without recurrence for about a year.
INTRODUCTION
Primary lymphomas of the gastrointestinal tract are the most common type of extranodal lymphoma, accounting for less than 12% of all non-Hodgkin's lymphoma (NHL)1, 2). The majority of these lymphomas arise in the stomach, with less than 30% arising in the small intestine. Among extranodal NHL, mucosa associated lymphoid tissue (MALT)-derived lymphoma (MALT lymphoma) was recognized as a distinct clinicopathological entity in the early 1980s, and can arise in the gastrointestinal tract, lung, eye, salivary gland, and thyroid gland, most frequently in the stomach. Gastric MALT lymphoma is associated with Helicobacter pylori (H. pylori) infection, and the eradication of H. pylori correlates with tumor regression3, 4). However, MALT lymphoma of the duodenum is very rare, and little is known about its treatment or clinical course. Although MALT lymphoma regression after H. pylori eradication has been sporadically reported5, 6), duodenal MALT lymphoma may be resistant to H. pylori eradication7, 8). In the current paper, we describe a case of primary duodenal MALT lymphoma that was resistant to H. pylori eradication and regressed after chemotherapy with cyclophosphamide, vincristine, and prednisolone (CVP).
MATERIALS AND METHODS
A 71-year-old woman was referred to our hospital because of dyspepsia and epigastric pain during the preceding 3 months. She had no allergies or past medical history, and her family history was unremarkable. The physical examination showed tenderness in the epigastrium but no peripheral lymphadenopathy, hepatosplenomegaly, or intra-abdominal mass. Laboratory examinations revealed normal blood counts and biochemistry and normal serum immunoglobulins. Gastroduodenoscopy revealed irregular nodular mucosal lesions with bleeding ulcerations that extended from the bulb to the second portion of the duodenum (Figure 1A). Histopathological examination of a biopsy specimen showed low-grade MALT lymphoma composed of atypical lymphoid cells with a lymphoepithelial lesion (Figure 2), positive for B-cell surface marker L26 (CD20) and negative for cyclin D1, CD3, and CD45RO. In the stomach, endoscopy and histology showed chronic superficial gastritis associated with H. pylori infection. Hospitalization was recommended for staging work-up, but she declined. We decided to eradicate H. pylori by treatment with amoxicillin (1000 mg twice daily), pantoprazole (40 mg twice daily), and clarithromycin (50 mg twice daily) for 1 week. Two months after the completion of antibiotic treatment, however, her symptoms were aggravated. Gastroduodenoscopy disclosed no evidence of H. pylori in the gastric mucosa, but no sign of regression of the duodenal lesion was observed.
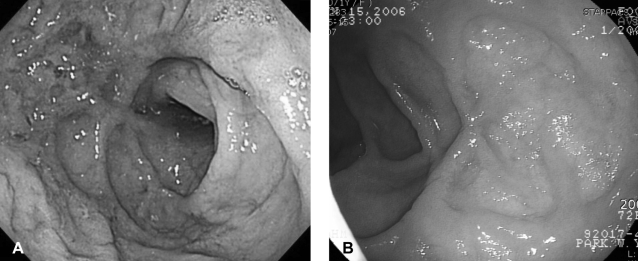
Gastroduodenoscopy. The initial gastroduodenoscopy reveals irregular nodular mucosal lesions with bleeding ulcerations extending form the bulb to the second portion of the duodenum (A). After 6 courses of chemotherapy, the follow-up gastroduodenoscopy shows complete regression of duodenal MALT lymphoma (B).

Histological examination of initial biopsy specimens from the duodenal lesion. A. Atypical lymphoid cells invading duodenal mucosa (H&E stain ×100). B. A lymphoepithelial lesion indicative of MALT lymphoma (H&E stain, ×200).
Thereafter, the patient was admitted for further evaluation and treatment of the duodenal MALT lymphoma. Chest CT scans showed no evidence of lymph node enlargement in the mediastinum. Abdominal CT scans revealed 0.5 to 1.5 cm lymph nodes in the peritoneal cavity, suggestive of lymph node metastasis (Figure 3A). Bone marrow biopsy showed no evidence of lymphoma involvement. The patient was classified as having stage EII2 MALT lymphoma according to the Ann Arbor classification modified by Musshoff9). We administered systemic chemotherapy with cyclophosphamide, vincristine, and prednisolone (CVP) every 3 weeks, which was well tolerated except for transient hair loss, and epigastric pain resolved after 2 cycles of chemotherapy. After 6 courses of CVP, the patient achieved complete remission (CR) (Figure 1B, 3B) and was followed up without recurrence for about a year.
DISCUSSION
Gastric MALT lymphoma has been considered to boe preceded by the acquisition of MALT as consequence of H. pylori infection. The involvement of H. pylori in the pathogenesis of monoclonal lymphoid proliferation may be due to a H. pylori-reactive T-cell-mediated reaction10). In contrast to gastric MALT lymphoma, the relationship between duodenal MALT lymphoma and H. pylori infection has not been established. For duodenal MALT lymphoma, H. pylori eradication may5, 6) or may not7, 8) lead to lymphoma regression. Here, H. pylori eradication did not cure duodenal MALT lymphoma.
Lepicard et al. reported four cases of duodenal MALT lymphoma treated with oral cyclophophamide (100 mg per day) for 18 months11). Tumor infiltration was limited to the duodenal wall in one case and was associated with locoregional lymphadenopathies in three cases. Three patients achieved CR and one achieved partial remission. However, two of the four patients with CR showed relapse microscopically after 2 years. These results suggest that oral cyclophosphamide may be a reasonable treatment option for slowly progressive disease. However, the long-term effects of this treatment strategy and the best approach to relapse remain to be determined. Ochi et al. reported regression of the MALT lymphoma confined from mucosa to submucosa of the duodenum after long-term treatment with clarithromycin12), which may have resulted from inhibition of lymphocyte activation. On the other hand, Ventrucci et al. reported a case of primary MALT lymphoma of the papilla of vater that regressed after eight monthly courses of CVP13). In our case, H. pylori eradication did not lead to lymphoma regression. Abdominal CT scans suggesting involvement of lymph nodes in the peritoneal cavity and the aggravation of symptoms prompted the use of systemic chemotherapy with 6 cycles of CVP, which was well tolerated and led to CR.
To the best of our knowledge, this is the first case report of a duodenal MALT lymphoma that showed complete remission with CVP chemotherapy. Given the indolent nature of this tumor, monotherapy with cyclophosphamide or clarithromycin may be a reasonable option for MALT lymphoma confined to the mucosa or submucosa of the duodenum. However, systemic chemotherapy may be optimal when there is locoregional lymph node involvement.
