The pattern of choosing dialysis modality and related mortality outcomes in Korea: a national population-based study
Article information
Abstract
Background/Aims
Since comorbidities are major determinants of modality choice, and also interact with dialysis modality on mortality outcomes, we examined the pattern of modality choice according to comorbidities and then evaluated how such choices affected mortality in incident dialysis patients.
Methods
We analyzed 32,280 incident dialysis patients in Korea. Patterns in initial dialysis choice were assessed by multivariate logistic regression analyses. Multivariate Poisson regression analyses were performed to evaluate the effects of interactions between comorbidities and dialysis modality on mortality and to quantify these interactions using the synergy factor.
Results
Prior histories of myocardial infarction (p = 0.031), diabetes (p = 0.001), and congestive heart failure (p = 0.003) were independent factors favoring the initiation with peritoneal dialysis (PD), but were associated with increased mortality with PD. In contrast, a history of cerebrovascular disease and 1-year increase in age favored initiation with hemodialysis (HD) and were related to a survival benefit with HD (p < 0.001, both). While favoring initiation with HD, having Medical Aid (p = 0.001) and male gender (p = 0.047) were related to increased mortality with HD. Furthermore, although the severity of comorbidities did not inf luence dialysis modality choice, mortality in incident PD patients was significantly higher compared to that in HD patients as the severity of comorbidities increased (p for trend < 0.001).
Conclusions
Some comorbidities exerted independent effects on initial choice of dialysis modality, but this choice did not always lead to the best results. Further analyses of the pattern of choosing dialysis modality according to baseline comorbid conditions and related consequent mortality outcomes are needed.
INTRODUCTION
The number of end-stage renal disease (ESRD) patients requiring dialysis treatment has been continuously and rapidly increasing over the past few decades. Although there is little controversy that kidney transplantation is the best renal replacement treatment for ESRD, there are many obstacles to its timely initiation, including a shortage of donated organs, cultural differences, or poor socioeconomic status. Consequently, more than 95% of incident ESRD patients are forced to initiate dialysis treatment with hemodialysis (HD) or peritoneal dialysis (PD) [1]. In this situation, choice of dialysis modality is particularly important and known to be influenced by various factors such as geography, patient characteristics and preferences, and medical conditions [2]. Among these factors, the patients’ underlying comorbidities are found to be the major independent determinants of dialysis modality choice [3]. Furthermore, these preexisting comorbidities showed significant interactions with dialysis modality on patients’ outcomes [4,5]. In this light, despite the relevance of surveying the nationwide patterns of dialysis modality choice according to underlying comorbidities and examining associated clinical outcomes, only a few studies have addressed this relationship [6].
We previously reported that, although it is being improved in recent years [7], PD is generally inferior to HD as an initial dialysis modality in Korea in terms of overall survival, and this is largely accounted for by the higher incidence of all-cause mortality, non-fatal acute myocardial infarction (MI), and vascular complications requiring target vessel revascularization [8,9] in incident PD patients. This finding was in contrast to recent studies of large-scale registry data, but the reasons for this inferiority of PD could not be adequately explained [10-12]. Therefore, in this study, we approached this issue first by assessing the pattern of modality choice for incident dialysis patients according to baseline comorbid conditions in Korea, and then evaluated how such choice affected mortality outcomes by calculating the synergy factor (SF) from the interaction analysis based on a multiplicative scale between the various comorbid conditions and dialysis modality [13].
METHODS
Data source and study population
We used the Korean Health Insurance Review and Assessment Service (HIRA) database. The detail of HIRA database organization was described elsewhere [9]. The Institutional Review Board at the HIRA approved our use of the database for this study (IRB No. 3159, 2012).
We initially screened all Korean incident dialysis patients who started dialysis therapy between January 1, 2005 and December 31, 2008. Among them, we only included patients who initiated dialysis treatment during the study period and remained on chronic dialysis therapy for at least 3 months. We excluded patients who were younger than 18 years. Finally, our study included 32,280 eligible patients. Further, we included both the patients who have National Health Insurance and those who have Medical Aid as primary insurance; Medical Aid is a public assistance program for poor individuals who are under the National Basic Livelihood Security System in Korea as a part of the social welfare programs [14]. In all analyses for comparisons between dialysis modalities, an intention-to-treat principle was adopted.
The comorbid conditions of the participants were identified by screening the medical records during the year before the initiation of dialysis therapy. The list of comorbidities was determined and scored based on the suggestions of Charlson et al. [15], and ICD-10 (International Classification of Diseases 10th revision) codes were used according to the algorithms proposed by Quan et al. [16].
Measurements and analyses of outcomes
The primary clinical endpoint of interest for our study was all-cause mortality. For assessing event-free survival, we considered the dialysis modality at day 90 to be the initial dialysis modality and used day 90 as the starting point (day 0). That is, the patients analyzed in this study were left-censored for the first event-free 90 days after dialysis initiation, and they were right-censored at December 31, 2009.
Statistical analysis
In comparison analyses, baseline parameters were compared using an independent t test for continuous variables and Pearson chi-square test for categorical variables. There was no missing data on baseline characteristics of participants and their outcomes. Crude incidence rates of mortality were calculated by dividing the number of deaths by the person-years of follow-up, expressed as deaths per 1,000 patient-years; confidence intervals (CIs) were estimated based on a Poisson distribution.
Multivariable-adjusted logistic regression analyses were conducted to estimate odds ratios for the likelihood of choosing an initial dialysis modality between two modalities according to the presence or absence of particular comorbid conditions. Cox proportional hazard regression analyses were performed to evaluate the increase in the absolute mortality risk associated with an initial dialysis modality according to the baseline comorbid conditions.
In addition, to assess the degree of change in the relative risk (RR) for mortality via effect modification between dialysis modality and various baseline comorbid conditions, interaction terms were constructed and entered into multivariable-adjusted Poisson regression analyses to test the statistical significance of these interactions on mortality. Furthermore, we quantified the degrees of these interactions in terms of SF with 95% CIs, based on a multiplicative scale. In brief, SF was calculated from the adjusted RRs. We first estimated the RRs for factor x1 alone (RR1), factor x2 alone (RR2), and both factors combined (RR12). SF was then defined as the ratio of the observed RR for both factors combined and presented as SF = RR12 / (RR1 × RR2). Thus, if SF > 1, this was interpreted as a positive interaction (a synergistic increase in the risk) between the two risk factors [13].
All statistical tests were evaluated using a two-tailed 95% CI, and p < 0.05 was considered statistically significant. All statistical analyses were conducted using the statistical package SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
RESULTS
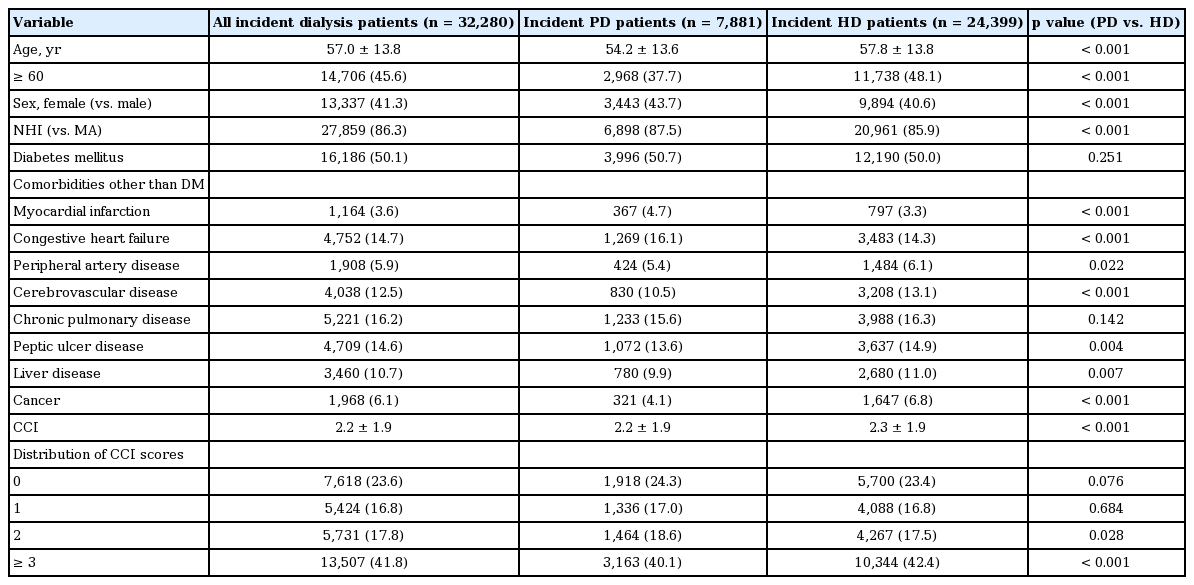
Baseline characteristics
A total of 32,280 eligible patients who initiated dialysis therapy between January 1, 2005 and December 31, 2008, were analyzed. When comparing patients who initiated dialysis therapy with PD versus HD, incident PD patients were significantly more likely to be younger and female, and more likely to have National Health Insurance (vs. Medical Aid) than incident HD patients. While the prevalence of diabetes and chronic pulmonary disease (CPD) was similar, the overall distribution of comorbid conditions was significantly different between patients on PD and those on HD (Table 1). The severity of comorbidities assessed by the Charlson comorbidity index (CCI) was also significantly different, and a high comorbidity burden (CCI ≥ 3) was significantly more prevalent in incident HD patients than in incident PD patients. During the median follow-up of 24.5 months (range, 3.1 to 59.0) and 67,541 patient-years, 7,820 deaths were observed, for an overall estimated death rate of 116 deaths (95% CI, 113 to 118) per 1,000 patient-years.
Comparison of the absolute mortality risk between PD and HD according to baseline comorbid conditions
As shown in Fig. 1, we performed Cox proportional regression analyses and found that overall absolute mortality risk adjusted for all baseline covariates listed in Table 1 was significantly 23% higher in the patients initiating dialysis with PD than those with HD. Then, we explored whether this trend was also apparent in various subgroups according to baseline comorbid conditions, and found that the patients initiating dialysis with PD generally have a significant higher absolute risk for mortality than those with HD across all subgroups. However, some exceptions were noted; there were no significant differences in mortality rates between PD and HD in the patients with age < 60 years, Medical Aid as their primary insurance, liver disease, cancer, or no comorbidity.
Comparisons of multivariable-adjusted mortality risks between peritoneal dialysis (PD) and hemodialysis (HD) by subgroups (adjusted hazard ratios [HRs] and 95% confidence intervals [CIs] for mortality by multivariable-adjusted Cox proportional hazard regression analyses). NHI, National Health Insurance; MA, Medical Aid; DM, diabetes mellitus; MI, myocardial infarction; CHF, congestive heart failure; PAD, peripheral artery disease; CVD, cerebrovascular disease; CPD, chronic pulmonary disease; PUD, peptic ulcer disease; LD, liver disease.
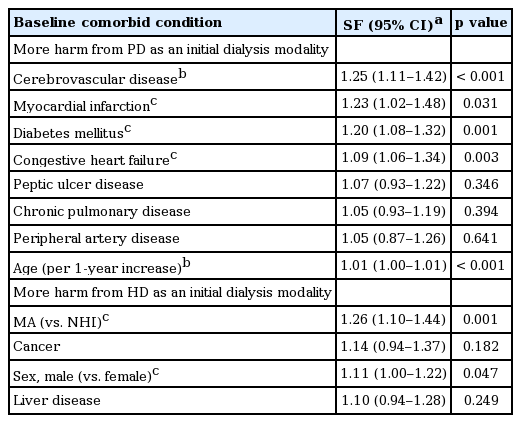
The pattern of choosing dialysis modality according to each comorbid condition and related mortality outcomes in all incident dialysis patients
First, we examined which baseline comorbid conditions were independently associated with the choice of a particular dialysis modality in all incident dialysis patients. After adjusting for all baseline conditions listed in Table 1, prior histories of MI, congestive heart failure (CHF), and diabetes were independently associated with a higher likelihood of receiving PD as an initial dialysis modality, whereas prior histories of cancer, cerebrovascular disease (CVD), and liver disease; Medical Aid as primary insurance; male gender; and a 1-year increase in age were independently associated with a higher likelihood of receiving HD as an initial dialysis modality (Table 2, Fig. 2, black bars).
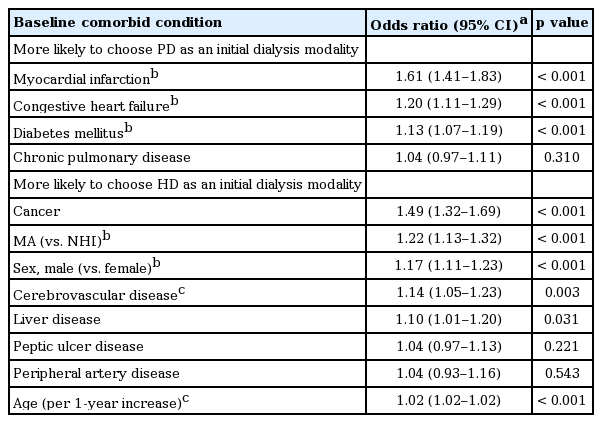
Multivariable-adjusted likelihood to choose dialysis modality according to baseline comorbid conditions in all incident dialysis patients
The pattern of choosing dialysis modality according to baseline comorbid conditions and related mortality outcomes. Black bars: multivariable-adjusted likelihood to choose dialysis modality according to baseline comorbid conditions in all incident dialysis patients (adjusted odds ratios and 95% confidence intervals [CIs] by multivariable-adjusted logistic regression analysis for choosing each dialysis modality). Red bars: multivariable-adjusted likelihood to experience more harm from one modality than from the other modality in all incident dialysis patients (adjusted synergy factors and 95% CIs based on a multiplicative interaction between initial dialysis modality and baseline comorbid conditions on mortality). Red shaded area: the pattern of choice for dialysis modality in this condition consequently increased the mortality risk (p < 0.05). Blue shaded area: the pattern of choice for dialysis modality in this condition consequently conferred the survival benefit (p < 0.05). MA, Medical Aid; NHI, National Health Insurance; HD, hemodialysis; PD, peritoneal dialysis.
Next, as shown by p values of interaction analyses in Fig. 1, we found that the relative degrees of risk for mortality increased by PD were significantly modified by the presence or absence of a particular comorbid condition. Therefore, we further examined the effects of these interactions between the independent determinants of initial modality choice and various baseline comorbid conditions on mortality (Table 3, Fig. 2, red bars). Among the independent determinants that led to the choice of PD as an initial modality, prior histories of MI, diabetes, and CHF showed a significant positive interaction with the initiation of dialysis with PD; that is, increased the risk of mortality when initiating dialysis treatment with PD. On the other hand, having Medical Aid as primary insurance and male gender were significant independent determinants of dialysis initiation with HD, and these choice patterns were eventually associated with a synergistically increased risk of mortality. In contrast, a history of CVD and a 1-year increase in age, which were significant independent determinants of dialysis initiation with HD, were associated with worse survival with PD (better survival with HD) (Table 3, Fig. 2).
The pattern of choosing dialysis modality according to each comorbid condition and related mortality outcomes in all incident dialysis patients < 60 years
When stratifying by age, we found that, in patients younger than 60 years, prior histories of MI, CHF, CPD, and diabetes were independently associated with a higher likelihood of receiving PD as an initial dialysis modality, whereas having Medical Aid as their primary insurance, male gender, a history of cancer, and a 1-year increase in age were independently associated with a higher likelihood of receiving HD as an initial dialysis modality (Supplementary Table 1).
The consequences of this choice are shown in Supplementary Table 2 and indicate that, among the determinants independently associated with the choice of PD as an initial modality, prior histories of MI and diabetes synergistically increased the risk of mortality when starting dialysis treatment with PD. On the other hand, among the determinants independently associated with the choice of HD as an initial modality, having Medical Aid as their primary insurance synergistically increased the risk of mortality when starting dialysis treatment with HD. In contrast, a 1-year increase in age, which was a significant independent determinant of dialysis initiation with HD, was associated with worse survival with PD (better survival with HD) (Supplementary Table 2).
The pattern of choosing dialysis modality according to each comorbid condition and related mortality outcomes in all incident dialysis patients ≥ 60 years
In patients aged 60 years or older, prior histories of MI and CHF were independently related to the choice of PD as an initial dialysis modality, whereas prior history of cancer, liver disease, or CVD; male gender; and a 1-year increase in age were independently associated with a higher likelihood of receiving HD as an initial dialysis modality (Supplementary Table 3). Among the significant determinants that led to the choice of PD as an initial modality, a prior history of CHF was significantly related to the synergistically increased risk of mortality when combined with the initiation of dialysis treatment on PD. On the other hand, among the significant determinants that led to the choice of HD as an initial modality, a prior history of cancer and male gender were significantly related to the synergistically increased risk of mortality when combined with the initiation of dialysis treatment on HD (Supplementary Table 4).
The pattern of choosing dialysis modality according to the severity and number of comorbidities and related mortality outcomes
Finally, we sought to evaluate the interaction effects between the pattern of modality choice and the severity and number of comorbidities on mortality outcomes. As shown in Table 4, Fig. 3, there was no significant difference in the odds of choice for either type of dialysis modality according to the severity of comorbidities assessed by CCI or the number of comorbidity (≥ 1 comorbidities vs. no comorbidity). However, looking at the consequences of such choice, we found that, as the severity and the number of comorbidities increased, the mortality risks of patients initiating dialysis therapy with PD were significantly increased compared to those initiating with HD; this trend was evident even from a CCI score of 1 or higher (p for trend < 0.001) (Table 5, Fig. 4).
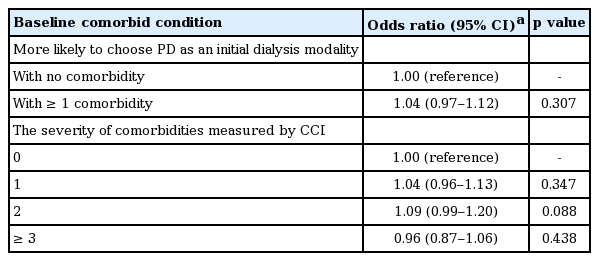
Multivariable-adjusted likelihood to choose PD as an initial dialysis modality according to the number and severity of comorbidities measured by CCI in all incident dialysis patients
Multivariable-adjusted likelihood to choose peritoneal dialysis (PD) as an initial dialysis modality according to the number and severity of comorbidities measured by Charlson comorbidity index (CCI) in all incident dialysis patients (adjusted odds ratios and 95% confidence intervals by multivariable-adjusted logistic regression analysis for choosing each dialysis modality). HD, hemodialysis.

Multivariable-adjusted likelihood to experience more harm with PD as an initial dialysis modality according to the number and severity of comorbidities measured by CCI in all incident dialysis patients

Multivariable-adjusted likelihood to experience more harm with peritoneal dialysis (PD) as an initial dialysis modality according to the number and severity of comorbidities measured by Charlson comorbidity index (CCI) in all incident dialysis patients (adjusted synergy factors and 95% confidence intervals based on a multiplicative interaction between initial dialysis modality and the number/ severity of comorbidities on mortality). HD, hemodialysis. aThe increases in the number of comorbidities (≥ 1 comorbidities vs. no comorbidity) and CCI scores significantly associated with the increase in mortality when accompanied by PD as an initial dialysis modality (p < 0.05).
DISCUSSION
In the current study, we found that some comorbid conditions were independently related to the choice of dialysis modality, and that this choice might not always lead to the best mortality outcome. Instead, such choices often synergistically increased mortality. To approach this issue is far from simple because preexisting comorbidity conditions are not the only determinant of dialysis modality in both physicians and patients, but various other factors are also involved.
During the study period, patients with diabetes, MI, or CHF had a significantly higher likelihood of being regarded as proper candidates for initiating dialysis therapy with PD, but all of these comorbid conditions synergistically increased the intrinsic mortality risk posed by PD per se. On the other hand, even though Medical Aid as primary insurance and male gender led to avoidance of PD as an initial dialysis modality, those conditions were found to significantly decrease the mortality risk conferred by PD per se (increased mortality risk with HD). A preferred implementation of PD for patients with diabetes has also been documented in several previous reports [3,17-19]. This finding can be explained by the belief in the potential advantages of PD over HD for maintaining more stable hemodynamic status, particularly under diabetes-related autonomic dysfunction and the absence of requirements for usable vascular access, which is difficult to achieve due to diabetes-related atherosclerotic calcification. However, contrary to this view but in accordance with our study, a large proportion of studies to date indicate that PD is associated with worse outcomes than HD when performed in diabetic patients [20-22]. Whether diabetes per se should be recognized as a contraindication to the use of PD remains highly controversial and far from being definitively answered [23].
In addition, a considerable number of studies have suggested that PD has possible advantages compared to HD in patients with underlying cardiac dysfunction. In particular, patients with medical treatment-resistant CHF have few therapeutic options other than heart transplantation, surgical plasty, or extracorporeal ultrafiltration. In such cases, short-term use of PD provides symptomatic relief and improvement of various cardiac indices [24,25]. In a similar way, PD is regarded as also having potential benefits for patients with coronary artery disease. Partly due to less abrupt hemodynamic disturbance than HD, PD is associated with a low probability of development of myocardial stunning represented by regional wall motion abnormalities, which are frequently observed in HD [26]. However, these inferences are based on small-scale observations that are neither adequately validated nor were evidenced in large-scale studies; rather, dialysis initiation with PD is associated with significantly higher mortality risk than with HD in incident ESRD patients with underlying CHF [5,27] or coronary artery disease [4]. Supporting these findings, a substantial number of studies have suggested that PD might be related to a greater atherogenic vascular risk than HD given a higher prevalence of dyslipidemia [28], a higher level of atherogenic lipoprotein(a) [29], and a higher prevalence of overhydration-related high blood pressure [30,31]. Continuous exposure to high glucose load induced by PD fluid might also contribute to PD-related cardiac compromise, possibly mediated through hyperinsulinemia with insulin resistance, hyperleptinemia, or inflammation with oxidative stress [32,33]. On the other hand, older patients or those with prior CVD were more likely to choose HD as an initial dialysis modality, and this trend in choice consequently conferred a survival benefit. Consistent with this, the relative advantages of HD over PD in elderly patients have been shown in previous reports [17,34], particularly in those with diabetes or longer dialysis vintage [35]. The cause of higher mortality with PD versus HD in elderly patients is not clear. However, it should be noted that cardiovascular mortality, as the most common cause of general ESRD patients, cannot solely account for this; rather, as the age of ESRD patients increases, noncardiovascular causes of mortality were more predominant than cardiovascular causes [20]. This pattern is especially apparent in PD-treated patients with diabetes, female gender, and advanced age [34]. In addition, partly due to functional impairments in handling PD equipments including PD solution exchange, and in performing PD-related selfcare, patients with CVD are not only less likely to initiate dialysis treatment with PD but also have potential disadvantages that can lead to PD-related adverse outcomes. In a long-term follow-up study of the patients who experienced a stroke, the most common cause of death was cardiovascular disease, with a rate of 67.4% [36]. This high atherosclerotic burden prior to and post stroke might not only be further complicated by the abovementioned metabolic derangements induced by PD, but also independently associated with an increased risk of PD peritonitis, which is an independent predictor of mortality [37,38].
When analyzed by age (≥ 60 years vs. < 60 years), we can observe that, as age increases, the number of comorbid conditions as well as the degree of risk increase independently related to the choice of a particular dialysis modality was decreased, suggesting that age itself might serve as the primary prognostic factor. However, underlying cardiac morbidities such as MI or CHF was consistently synergistically increased the risk of mortality when initiating dialysis treatment with PD, irrespective of age groups.
In this study, we also found that the number or severity of comorbidities was not a determinant of the dialysis modality choice. However, increased mortality was observed in a significant linear trend when patients with a higher comorbidity initiated dialysis with PD compared to HD (p for trend < 0.001). The distribution of the degree of comorbidities measured by CCI or other parameters between incident patients on HD and PD is not consistent across studies. It has been reported that, in Canada, the United States, and Europe, patients with a higher comorbidity level tend to start dialysis therapy with HD instead of PD [6,18,19,39], whereas, in Columbia, incident PD patients have a significantly higher degree of comorbidity than HD patients [40]. How dialysis modalities modify the mortality risk according to the degree of comorbidities has also been investigated in a few studies. In agreement with our findings, studies investigating the European ERA-EDTA (The European Renal Association-European Dialysis and Transplant Association) and Australia and New Zealand registries commonly showed the superiority of PD over HD for survival in patients with no comorbidity, but this effect disappears as the number of comorbidities increases [6,41]. Also in a large Taiwanese cohort stratified by CCI score, the patients belonging to the group with the highest CCI score had a significant 21% higher mortality risk with PD than with HD [42].
When focusing on HD, we found that patients who were male and had Medical Aid as their primary insurance were significantly more likely to start dialysis treatment with HD, but this choice was associated with an increase in mortality risk. The trend that incident ESRD patients on PD were of higher socioeconomic status than those on HD was in accordance with previous studies [18,39]. This difference may result from several parameters that are difficult to measure, such as hygiene status, accessibility to medical service, or reimbursement factors [43].
We should note the limitations of this study and necessary precautions in interpreting the results. First, since the comorbidities listed in this study were assessed by reviewing the diagnosis codes claimed, the possibility of underestimation or oversimplification of the comorbidity burden or of missing the effects of other important conditions not addressed in this study could not be excluded. Second, due to the limitations of the dataset, we could not access either the causes of death or the information on dialysis-related factors potentially affecting patients’ mortality such as HD adequacy, nutritional status, infection rates, or other non-conventional risk factors. Fourth, and most importantly, we focused only on the relative degrees of advantage or disadvantage of one modality versus the other modality using SF based on multiplicative interaction analyses. Therefore, caution is required when interpreting the results.
In conclusion, we found that some types and severity of comorbidities exerted independent effects on the choice of dialysis modality, but this choice did not always lead to the best outcomes. Based on our observations, the overall worse outcomes of incident PD patients compared to HD patients during the study period might result from, at least in part, more frequent use of PD in the patients with prior MI, CHF, diabetes or with a higher degree of comorbidity. To improve the survival rate of dialysis patients, further intensive investigation of the pattern of choosing dialysis modality according to baseline comorbid and other conditions, and reviews of the related consequences on mortality outcomes are warranted.
KEY MESSAGE
1. Some types and severity of comorbidities exerted independent effects on the choice of dialysis modality, but this choice did not always lead to the best outcomes.
2. The overall worse outcomes of incident peritoneal dialysis (PD) patients compared to hemodialysis patients during the study period (between January 1, 2005 and December 31, 2009) might result from more frequent use of PD in the patients with prior myocardial infarction, congestive heart failure, diabetes or with a higher degree of comorbidity.
3. Further intensive investigation of the pattern of choosing dialysis modality according to baseline comorbid and other conditions, and reviews of the related consequences on mortality outcomes are warranted to improve the survival rate of dialysis patients.
Notes
No potential conflict of interest relevant to this article was reported.
Supplementary Materials
Multivariable-adjusted likelihood to choose dialysis modality according to baseline comorbid conditions in incident dialysis patients aged less than 60 years
Multivariable-adjusted likelihood to experience more harm from one modality than from the other modality in incident dialysis patients aged less than 60 years