Drug-resistance pattern of Mycobacterium tuberculosis strains from patients with pulmonary and extrapulmonary tuberculosis during 2006 to 2013 in a Korean tertiary medical center
Article information
Abstract
Background/Aims
We evaluated the trend in the rates of drug-resistant tuberculosis (TB) over time, as well as the difference in the drug-resistance pattern between pulmonary tuberculosis (PTB) and extrapulmonary tuberculosis (EPTB) at a private referral center in South Korea.
Methods
All patients with culture-confirmed TB from 2006 to 2013 were included.
Results
In total, 1,745 patients were included: 1,431 (82.0%) were new cases, and 314 (18.0%) were cases treated previously; 1,610 (92.3%) were diagnosed with PTB, and 135 (7.7%) were diagnosed with EPTB. Multidrug-resistant (MDR) and extensively drug-resistant (XDR) TB were detected in 5.8% and 2.0% of new cases and in 20.1% and 8.6% of previously treated cases, respectively. The MDR TB rate during the study period decreased remarkably, whereas the MDR and XDR TB rates decreased significantly in previously treated cases. No difference in the drug-resistance rate was detected between PTB and EPTB.
Conclusions
The TB drug-resistance rate, particularly that of MDR TB, remained high at a private referral hospital, and the drug-resistance rate did not decrease significantly from 2006 to 2013. This finding underscores the need for a national survey regarding the prevalence of drug-resistant TB to obtain the most accurate and current drug-resistance status in South Korea, including the private sector.
INTRODUCTION
Drug-resistant tuberculosis (TB) is a global concern. However, the overall incidence of TB has been decreasing slowly since 2004 because of the World Health Organization (WHO) efforts through the Stop TB Strategy [1]. Nevertheless, there is no definitive evidence that the incidence of multidrug-resistant (MDR) TB is decreasing, despite this global effort [2]. Although considerable efforts in several countries, including South Korea, have led to a slow decrease in the overall incidence of TB, surveillance indicates that the incidence of drug-resistant TB is rising [3,4,5]. Drug-resistant TB strains in South Korea account for 5.3% to 12.2% of new cases and 13.3% to 41.6% of previously treated cases, whereas MDR-TB strains account for 2.7% to 3.9% of new TB cases and 14.0% to 27.2% of previously treated cases [3,6,7,8].
Drug-resistance is a critical determinant of treatment success. Thus, to improve treatment success, the Mycobacterium tuberculosis drug-resistance pattern in community-based care should be determined. Despite geographical variations, a few studies have reported that drug-resistant TB occurs less often in cases of extrapulmonary tuberculosis (EPTB) than in cases of pulmonary tuberculosis (PTB) [9,10]. However, insufficient data are available regarding the current status of anti-TB drug-resistance in South Korea since 2008. Furthermore, there are no remarkable drug-resistance data for EPTB. Therefore, we evaluated the prevalence of drug-resistance among M. tuberculosis isolates, as well as differences in the drug-resistance pattern among the M. tuberculosis isolates that cause PTB or EPTB.
METHODS
Study population and design
This study was conducted at Inje University Busan Paik Hospital (903-bed, university-affiliated, tertiary referral hospital in Busan, Republic of Korea). Isolates obtained from patients with a positive M. tuberculosis culture at Inje University Busan Paik Hospital from January 2006 through December 2013 were included in this retrospective analysis.
This study identified trends in the resistance rates to anti-TB drugs among M. tuberculosis isolates recovered from patients diagnosed with TB over 8 years, which were determined using the proportional method [7]. We compared the drug-resistance pattern of M. tuberculosis isolates based on patient treatment history. In addition, we compared the drug-resistance pattern of M. tuberculosis isolates that cause PTB with those that cause EPTB.
Laboratory methods
Clinical specimens were cultured on 3% Ogawa medium (Shinyang, Seoul, Korea). The Mycobacteria Growth Indicator Tube 960 System (Becton Dickinson Co., Franklin Lakes, NJ, USA) was introduced at our institution on January 1, 2009. Therefore, both solid and liquid media were used to culture mycobacteria beginning in 2009. All specimens were processed and pretreated, as recommended previously [11]. All M. tuberculosis isolates were sent to the Korean Institute of Tuberculosis (KIT), a WHO-designated Supranational Reference Laboratory, for drug-sensitivity testing (DST). If multiple isolates were obtained from the same patient, only the first isolate was used for DST.
Resistance to anti-TB agents at the KIT is defined as mycobacterial growth in Lowenstein-Jensen medium > 1% using the proportional method and observed at the following critical drug concentrations: isoniazid (INH), 0.2 mg/mL; rifampicin (RFP), 40.0 mg/mL; rifabutin (Rfb), 20.0 mg/mL; ethambutol (EMB), 2.0 mg/mL; streptomycin (SM), 4.0 mg/mL; kanamycin (KM), 4.0 mg/mL; amikacin (Amk), 4.0 mg/mL; capreomycin (CPM), 4.0 mg/mL; ofloxacin (Ofx), 2.0 mg/mL; moxifloxacin, 2.0 mg/mL; levofloxacin, 2.0 mg/mL; prothionamide, 40.0 mg/mL; cycloserine (Cs), 30.0 mg/mL; and para-aminosali cylic acid, 1.0 mg/mL, respectively. Pyrazinamide (PZA) susceptibility was determined using the pyrazinamidase test [7].
Definitions
PTB was defined as TB involving the lung parenchyma. EPTB was defined as TB involving organs other than the lungs; e.g., pleura, without radiographic abnormalities in the lungs, lymph nodes, abdomen, genitourinary tract, skin, joints and bones, or meninges and with the confirmed presence of at least one M. tuberculosis specimen. A patient with both PTB and EPTB TB was classified as PTB [12].
Patients diagnosed with TB were classified into two groups according to their treatment history at the time of diagnosis: new cases included patients who had never received TB treatment or who had received treatment for < 4 weeks, and previously treated cases included patients who had taken anti-TB drugs for at least 4 weeks [13]. Moreover, previously treated cases were classified into three categories of relapse, treatment after failure (TAF), and treatment after interruption (TAI). "Relapse" was defined as patients who had completed their treatment but TB re-developed, "TAF" was defined as patients whose treatment had failed in the past but was resumed, and "TAI" was defined as patients with a treatment history ≥ 1 month, along with a cessation period ≥ 2 months [14].
The drug-resistance pattern was classified as follows: any drug-resistance was defined as resistance to any anti-TB drug, monodrug-resistant TB was defined as resistance to only one of the five first-line drugs (INH, RFP, EMB, PZA, and SM), MDR TB was defined as resistance to at least INH and RFP, and extensively drug-resistant (XDR) TB was defined as resistance to any fluoroquinolone and resistance to at least one of three injectable second-line drugs (AMK, CPM, and KM), in addition to MDR [13].
Statistical analysis
Results are presented as medians and interquartile ranges or as numbers (percentages). Continuous data were compared using the Mann-Whitney U test, and categorical data were compared with Pearson chi-square or Fisher exact tests. The drug-resistance trend over time was evaluated using the Cochran-Armitage trend test. All tests were two-sided, and a p < 0.05 was considered to indicate significance. Data were analyzed using IBM SPSS version 21 (IBM Co., Armonk, NY, USA).
Ethics statement
This study protocol was approved by the Institutional Review Board of Inje University Busan Paik Hospital. The requirement for informed consent was waived by the board.
RESULTS
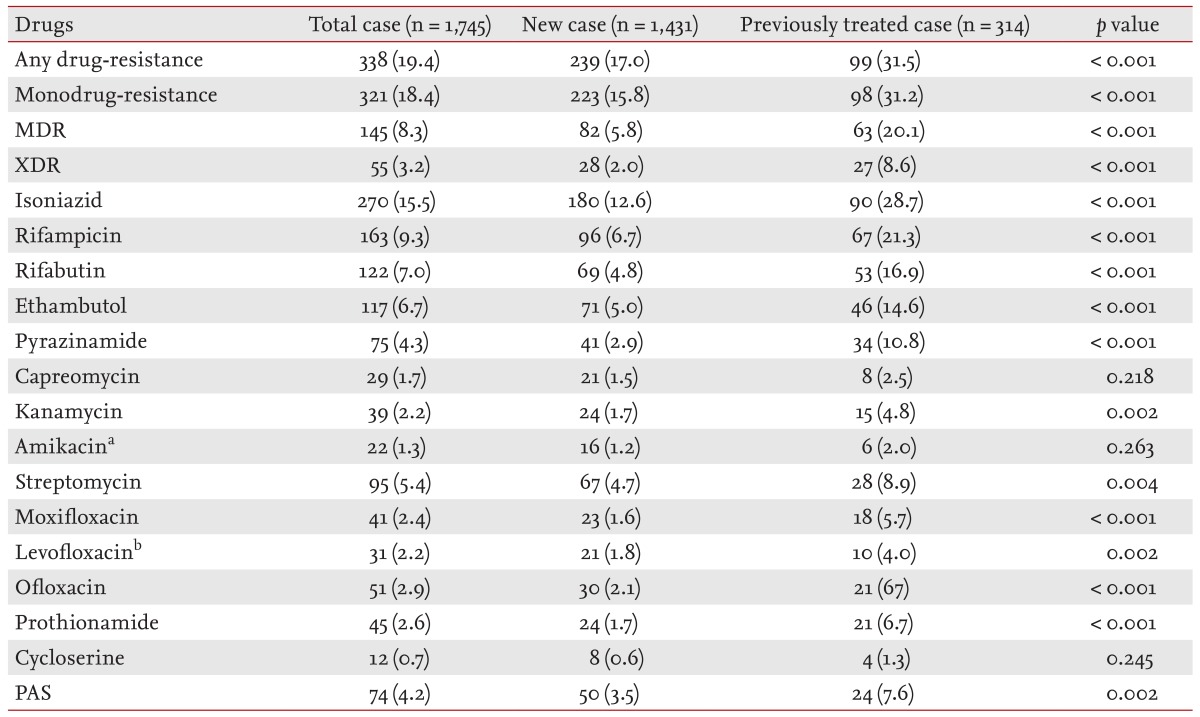
The DST results of the M. tuberculosis culture isolates obtained from 1,745 patients during the 8-year study period were analyzed for changes in drug-resistance patterns (Table 1). Among the 1,745 TB cases, 1,431 patients (82.0%) had no history of TB treatment (new cases), and 314 (18.0%) had a history of TB treatment for ≥ 1 month (previously treated cases). Of the 314 previously treated cases, 254 (80.1%), 48 (15.3%), and 12 (3.8%) were relapse, TAI, and TAF cases, respectively. Among the patients, 1,610 (92.3%) had PTB, and 135 (7.7%) had EPTB (45 cases of concurrent EPTB/PTB classified as PTB according to the definition). The most common disease site of the EPTB cases was the pleura, followed by the bones and joints. The median age of the patients was 54 years, and 1,024 (58.9%) of the patients were male.
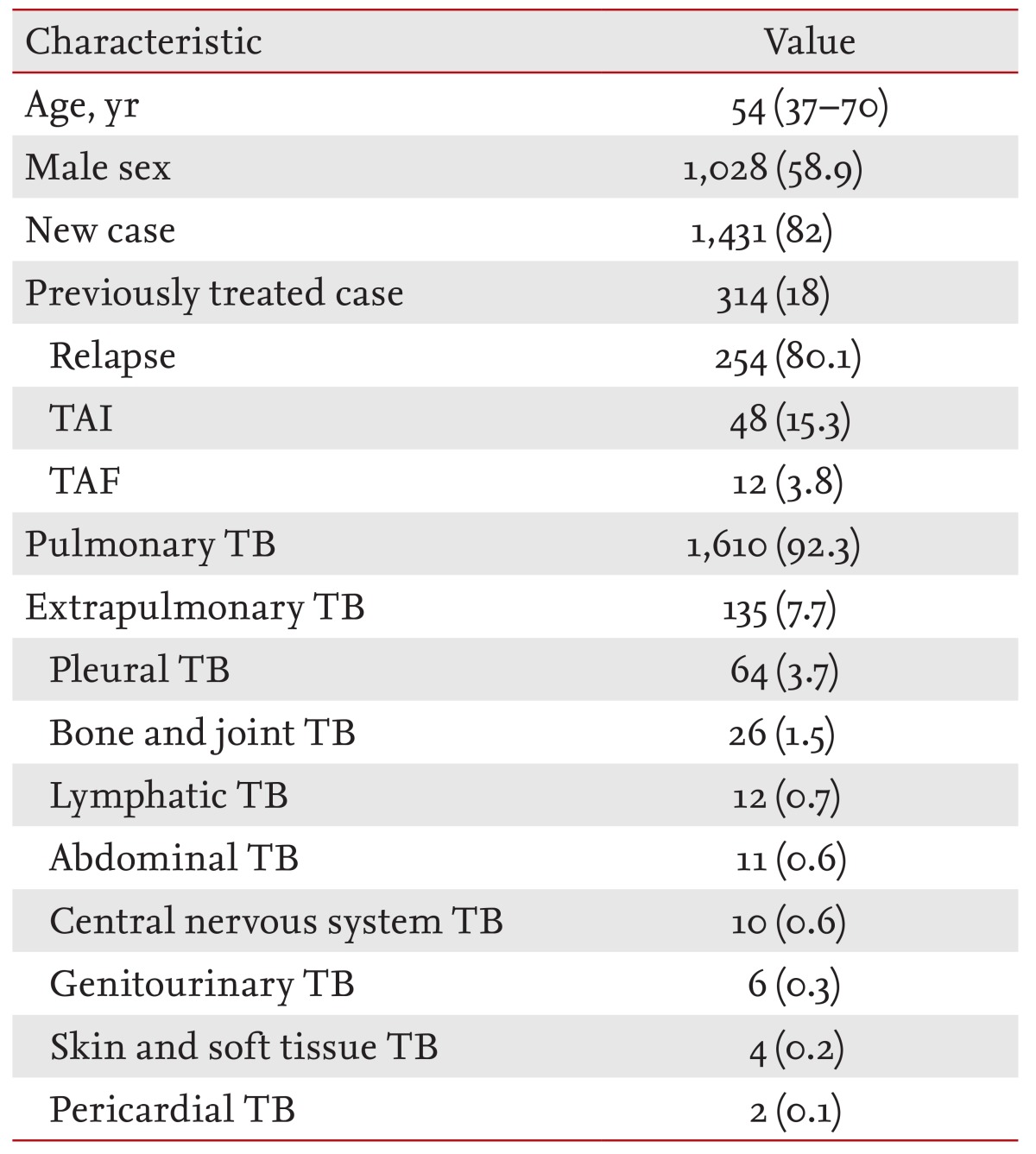
Demographic and clinical characteristics of the patients diagnosed with tuberculosis from 2006 to 2013 (n = 1,745)
M. tuberculosis drug-resistance trend
Among the M. tuberculosis strains isolated from the 1,745 patients, 1,406 (80.6%) and 1,423 (81.5%) were susceptible to all anti-TB drugs and all first-line drugs tested, respectively. Among them, 338 (19.4%), 321 (18.4%), 145 (8.3%), and 55 (3.2%) were any-drug-resistant, monodrug-resistant, MDR, and XDR TB, respectively. A trend analysis performed according to the drug-resistance pattern classification did not show a decrease in the rates of any-drug-resistant TB, monodrug-resistant TB, or MDRTB, except XDR TB (Fig. 1). The drug-resistance patterns of all cases for each anti-TB drug are summarized in Table 2. A significant decline in the drug-resistance rates to PZA, CPM, KM, and Ofx was observed during the 8-year study period.
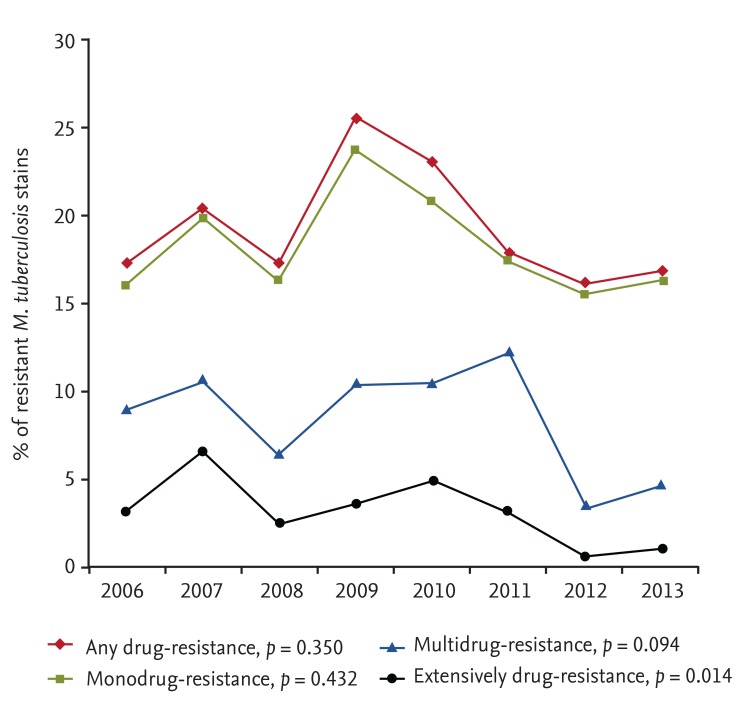
Trends in resistance rates to anti-tuberculosis drugs among Mycobacterium tuberculosis strains recovered from all 2006 to 2013 cases.
M. tuberculosis drug-resistance according to previous treatment status
According to previous treatment status, 1,191 new cases (83.2%) were susceptible to all anti-TB drugs, whereas 68.5% (215/314) of previously treated cases were susceptible to all anti-TB drugs. The resistance patterns to each anti-TB drug based on previous treatment status are summarized in Table 3. The previously treated TB cases had a higher rate of resistance to almost all anti-TB drugs, except CPM and Cs, compared with that of new TB cases. In addition, patients with any-drug-resistant TB, monodrug-resistant TB, MDR TB, and XDR TB were more likely to belong to the previously treated group. The resistance patterns to each anti-TB drug according to previously treated cases of relapse, TAI, and TAF are summarized in Table 4. TAF and TAI cases had a higher rate of resistance to almost all anti-TB drugs, compared with that of the relapse cases.
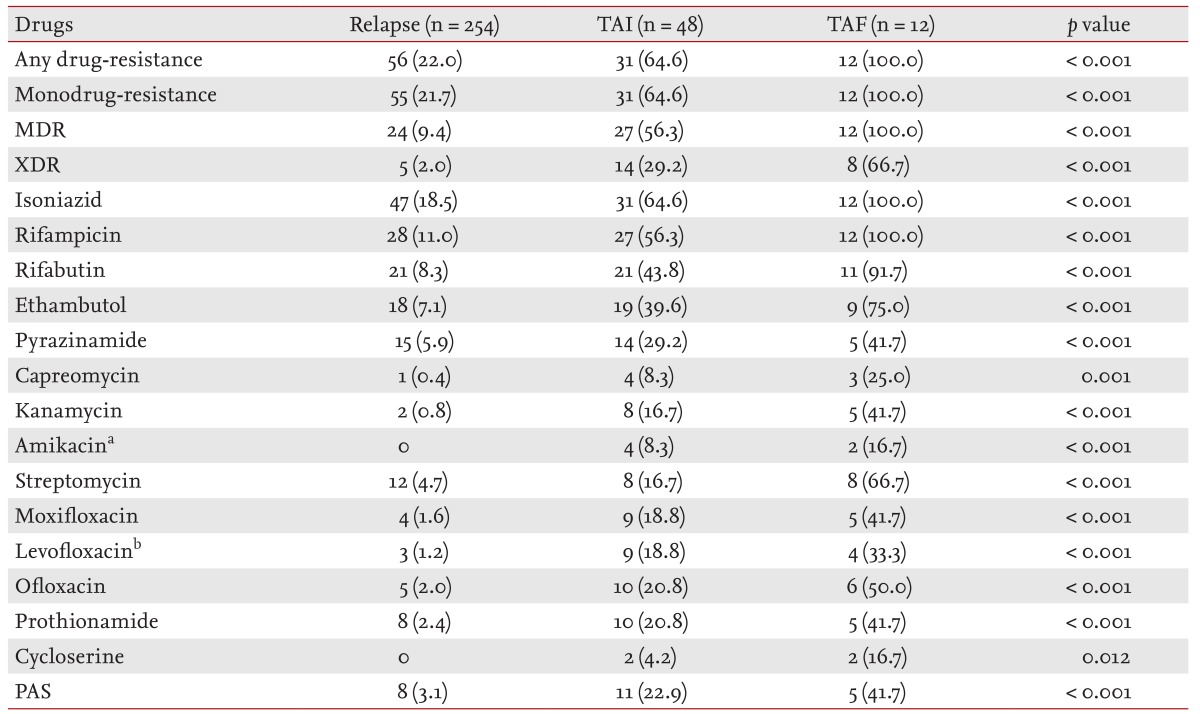
Resistance to anti-tuberculosis drugs according to previously treated cases of relapse, TAI, and TAF (n = 314)
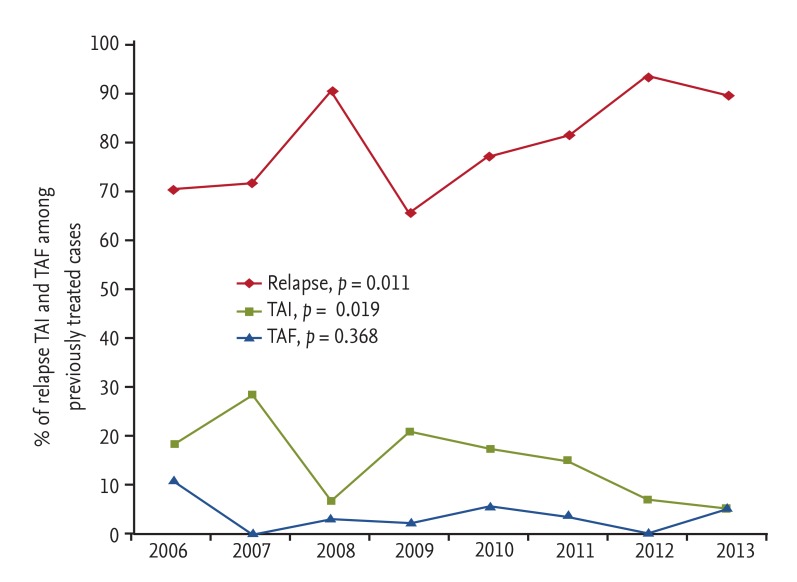
A trend analysis performed according to previous treatment status showed a significant decrease in the rates of MDR TB and XDR TB in the group of previously treated cases but not in the group of new cases (Fig. 2). Moreover, a trend analysis performed according to previously treated cases of relapse, TAI, and TAF showed a significant increase in the proportion of relapse and a significant decrease in the proportion of TAI cases. However, no marked change in the TAF trend was detected (Fig. 3).
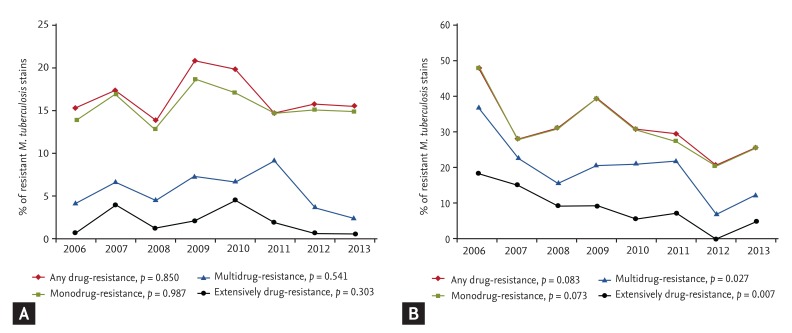
Trends in resistance rates to anti-tuberculosis drugs among Mycobacterium tuberculosis strains according to treatment history from all 2006 to 2013 cases. (A) New cases, (B) previously treated cases. All drug-resistance rates are the same as the monodrug-resistance rate, except in 2011.
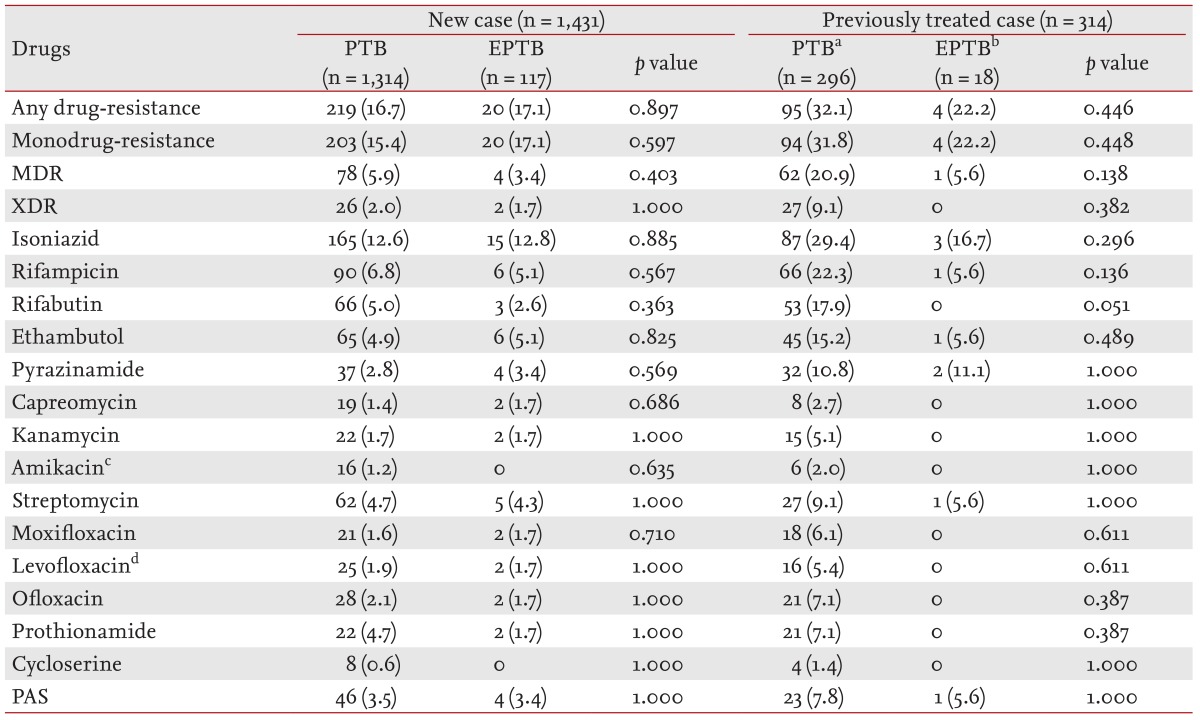
M. tuberculosis drug-resistance according to pulmonary/extrapulmonary involvement and previous treatment status
The drug-resistance patterns to each anti-TB drug according to PTB/EPTB and previous treatment status are summarized in Table 5. Of the 314 previously treated cases, 296 (94.2%) had PTB, and 18 (5.7%) had EPTB. Among the 296 PTB cases, 237 (80.1%), 47 (15.9%), and 12 (4.1%) were relapse, TAI, and TAF cases, respectively. In contrast, 18 EPTB cases were almost relapse (94.4%), except one. No significant difference was observed in the drug-resistance rate between PTB and EPTB based on previous treatment status.
M. tuberculosis drug-resistance to PTB according to age
The highest prevalence of drug-resistance was observed in the 50 to 59 year age group among new patients with PTB (any drug-resistance, 20.3%; monodrug-resistance, 18.5%; MDR, 8.6%; and XDR, 1.8%) (Table 6).
DISCUSSION
In this study, we investigated changes in TB drug-resistance patterns and differences in the drug-resistance pattern among new and previously treated TB cases. In addition, we compared the prevalence of drug-resistant TB observed in patients with PTB with that observed in patients with EPTB. The major findings were as follows. The rates of MDR and XDR TB in the private referral hospital remained high, but a slow decrease over time was suspected, particularly for previously treated TB cases. This finding may have been affected by changes in the proportions of relapse and TAI cases over time. In addition, although we evaluated a small number of EPTB cases, no difference in the drug-resistance rate between cases of PTB and EPTB was detected.
Determining the change in the TB drug-resistance rate over time and its current status in a region or nation are essential to adequately administer anti-TB regimens and achieve treatment success. According to the annual report of the Korea Centers for Disease Control and Prevention of 2012, 1,212 MDR TB cases were reported via the national TB monitoring system, which is a large burden in Korea despite a national effort [15]. However, no information regarding whether these were new or previously treated cases is available, despite the fact that a TB treatment history is a potent risk factor for MDR TB [16]. In addition, the proportions of patients with any-drug-resistant or monodrug-resistant TB are also unknown. According to the most recently published data regarding drug-resistance rates in 2009 in a public health center, the percentage of any-drug-resistant TB strains was 12.6% of new cases and 20.0% of previously treated cases. In addition, the percentage of MDR strains was 2.8% of new cases and 8.5% of previously treated cases [17].
However, the number of TB cases treated in the private sector has been increasing continuously and was 90.4% in 2012, as assessed by the national TB monitoring system [15]. Several studies have analyzed the TB drug-resistance rate in the Korean private sector [3,6,17,18,19,20,21]. Unfortunately, no reported data are available regarding the drug-resistance rate in the private sector after 2009. Furthermore, patients diagnosed with MDR or XDR TB since 2011 must be hospitalized to prevent transmission of drug-resistant pathogens based on the revised Korean National Tuberculosis Control program. Therefore, a more accurate evaluation of the drug-resistance rate among TB cases in private sector clinical settings and the trend in the drug-resistance rate among TB cases is needed.
According to previous studies performed in the private sector based on TB strains identified before 2009 [3,6,17,18,19,20,21], the any-drug-resistant TB rate was 15.0% to 20.4%, the monodrug-resistant TB rate was 6.4% to 17.6%, the MDR TB rate was 4.4% to 13.2%, and the XDR TB rate was 0.5% to 1.4%. In addition, MDR TB accounted for 2.9% to 5.1% of new cases and 9.3% to 41.8% of previously treated cases, whereas XDR TB accounted for 0.3% to 1.1% of new cases and 2.2% to 47.3% of previously treated cases. These studies show that any-drug-resistant and MDR TB decreased from 2001 to 2006. However, no definitive trend was observed for the gradual decrease from 2007 to 2008.
In our study, the any-drug-resistant TB rate was 19.4%, the monodrug-resistant TB rate was 18.4%, the MDR TB rate was 8.3%, and the XDR TB rate was 3.2%. In addition, any-drug-resistant TB accounted for 17.0% of new cases and 31.5% of previously treated cases. Monodrug-resistant TB accounted for 15.8% of new cases and 31.2% of previously treated cases. MDR TB accounted for 5.8% of new cases and 20.1% of previously treated cases. Finally, XDR TB accounted for 2.0% of new cases and 8.6% of previously treated cases. Although the drug-resistance trend among all TB cases did not decline remarkably over the study period, except XDR TB, the proportions of MDR and XDR TB decreased gradually among previously treated cases. This observation could be a result of the significant increase in the proportion of relapse cases and a decrease in the proportion of TAI cases during the study period. Because the drug-resistance rate is much higher in TAI cases than that in relapse cases, it may have affected the gradual decrease in the drug-resistance rate of the previously treated cases.
Although drug-resistant TB is a critical determinant of treatment success in a TB control program, few studies have compared the drug-resistance pattern of PTB with that of EPTB. In addition, three studies have reported that MDR TB occurs less frequently in EPTB cases than it does in PTB cases [9,10,22]. Thus, we compared the pattern of drug-resistance in EPTB with that observed in PTB. However, we found no difference in the drug-resistance rate between PTB and EPTB according to previous treatment status.
MDR TB was less frequent among patients with EPTB than it was among those with PTB, which was similar to results reported previously. However, the drug-resistance rates of almost all anti-TB drugs, except that of Rfb, were not different. In reports from Taiwan and Russia [10,22], the monodrug-resistance rate in patients with EPTB was also significantly lower than that in patients with PTB.
A possible explanation for this finding is that all cases were culture-confirmed cases. Thus, it was possible that many drug-sensitive EPTB cases were excluded. In an actual clinical setting, many EPTB cases are diagnosed without culture because isolating M. tuberculosis from an EPTB site is difficult, although the WHO recommends culturing specimens from a suspected extrapulmonary site. In fact, the proportion of EPTB cases among all TB cases was lower (7.7%) in our study than the 21.8% reported in the USA, the 27.5% reported in Russia, and the 21.4% reported in Taiwan [9,10,22]. Another possible explanation is that the proportion of drug-resistant strains of infectious TB bacilli in a community affects similar drug-resistance to PTB and EPTB. In contrast, another possible explanation is that studies conducted outside Korea were based on the specimen site, without considering concurrent EPTB and PTB [10]. In addition, another study excluded cases of concurrent EPTB and PTB [9]. In our study, we classified pulmonary and EPTB separately, as recommended by the WHO [12], although we found few concurrent EPTB and PTB cases (n = 45).
This study had several limitations. First, it was performed in a single tertiary referral center; thus, the results may not reflect the overall situation in South Korea. Second, a lack of information regarding the DST for previous TB infections in the previously treated TB cases precluded ascertaining whether drug-resistance was attributable to inadequate or incomplete treatment or whether it was the result of a previous infection with a resistant strain. We attempted to obtain past DST records of previously treated cases via the public health center; however, many of these records could not be traced. Third, some previously treated cases in the private sector may have been misclassified as new cases. Moreover, new drug-resistant patients may have a greater tendency to visit a tertiary hospital, which may have affected our results, as the new drug-resistant and MDR rates were higher than those reported from public health centers.
In conclusion, the TB drug-resistance rate, particularly that of MDR TB, remains high at a private referral hospital, and the drug-resistance rate did not decrease significantly from 2006 to 2013. However, the proportions of MDR and XDR TB cases since 2006 are suspected to have decreased consistently among previously treated cases. This finding may be a result of the significant increase in the proportion of relapse cases and a decrease in the proportion of TAI cases over time. In addition, we found no remarkable difference in the drug-resistance rate between PTB and EPTB. However, a national survey of the prevalence of drug-resistant TB should be conducted to obtain the most accurate drug-resistance status in South Korea, including the private sector. However, this will require a vast amount of time and financial investment.
KEY MESSAGE
The tuberculosis (TB) drug-resistance rate, particularly that of multidrug-resistant TB, remains high at a private referral hospital, and the drug-resistance rate did not decrease significantly from 2006 to 2013.
No remarkable difference in the drug-resistance rate was observed between pulmonary tuberculosis and extrapulmonary tuberculosis.
Acknowledgments
The authors thank Ms. Sarah Jang and Seolah Kim for their help with data collection and analysis.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.