Clinical outcomes of gastric variceal obliteration using N-butyl-2-cyanoacrylate in patients with acute gastric variceal hemorrhage
Article information
Abstract
Background/Aims
To evaluate the long-term efficacy and safety of endoscopic injection of N-butyl-2-cyanoacrylate (NBC; Histoacryl) for treatment of bleeding gastric varices.
Methods
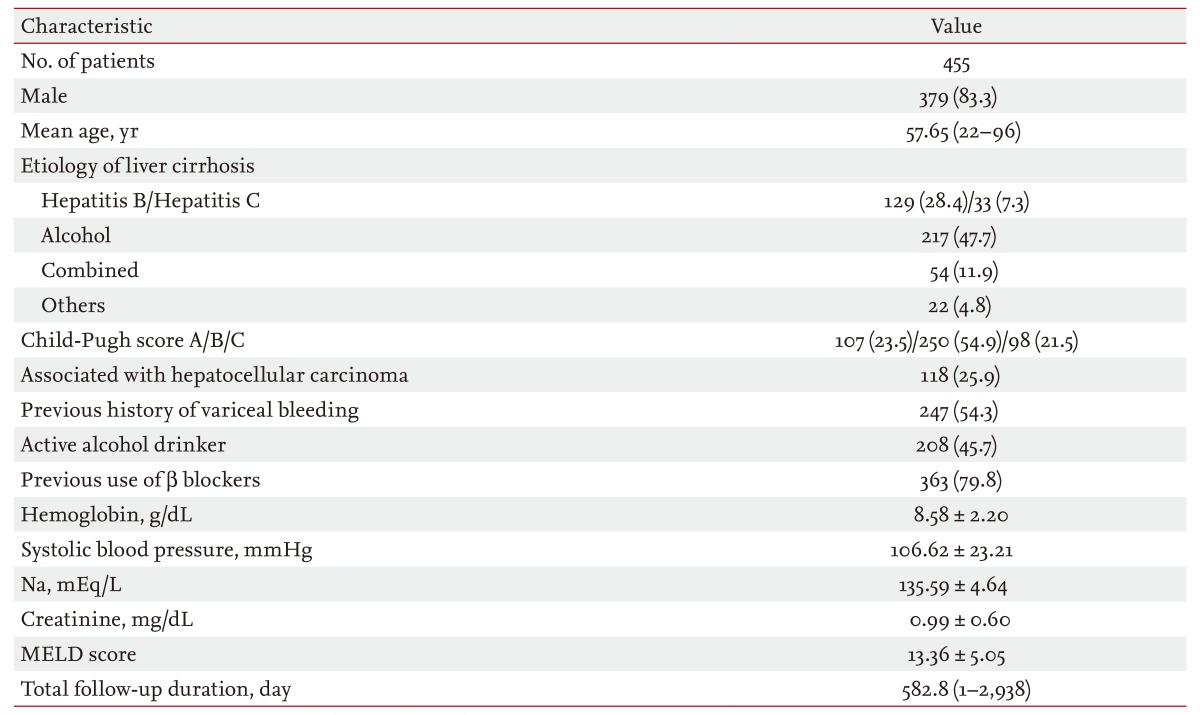
We retrospectively analyzed the records of 455 patients with gastric variceal hemorrhage (GVH) who were consecutively treated with NBC from January 2004 to July 2013, with a mean follow-up period of 582 days. The patients' endoscopic findings, initial hemostasis, complications, rebleeding rates, and bleeding-related death rates were reviewed.
Results
Hemostasis was achieved initially in 96.9% (441/455) of patients; rebleeding occurred in 35.2% (160/455), and the bleeding-related death rate was 6.8% (31/455) during follow-up. Complications included fever (6.8%), abdominal pain (3.7%), diarrhea (1.3%), spontaneous bacterial peritonitis (0.7%), bacteremia (0.4%), and embolism (0.2%). A red-color sign on concomitant esophageal varices (EVs) (p = 0.002) and previous history of variceal bleeding (p < 0.001) were significant risk factors for rebleeding within 1 year. The Child-Pugh score (p < 0.001), presence of hepatocellular carcinoma (p = 0.001), and failure of initial hemostasis (p < 0.001) were the risk factors most closely associated with bleeding-related death.
Conclusions
This study provides a comprehensive overview of the outcomes and prognostic factors of patients with GVH. The results may help in the selection of effective treatment strategies for patients with GVH.
INTRODUCTION
The prevalence of gastric varices (GVs) in patients with portal hypertension varies from 18% to 70% [1,2]. Although gastric variceal hemorrhage (GVH) is less common than esophageal variceal hemorrhage, it tends to be more severe, requires more transfusions, and has a higher mortality rate (45%) [3]. GVH also has a high rebleeding rate of 34% to 89% [4].
Treatment options for GVH include endoscopic treatment (including sclerotherapy and band ligation), transjugular intrahepatic portosystemic shunt creation, and balloon-occluded retrograde transvenous obliteration. Although limited data exist on the optimal management for GVH, the first-line treatment recently advocated for GVH is endoscopic obliteration using N-butyl-2-cyanoacrylate (NBC; Histoacryl, B. Braun Dexon GmbH, Spangenberg, Germany) [5,6].
NBC polymerizes from liquid glue to a plastic cast on contact with blood in the varix; this can control active variceal bleeding [7]. NBC injection achieves primary hemostasis in 70% to 100% of patients with acute GVH and has a low complication rate [6,8,9]. Eighty percent of cases of rebleeding occur within 1 year [10]. Despite published reports, limited data exist on rebleeding rates according to time, predictors of bleeding-related death, and long-term efficacy and safety of endoscopic obliteration of GV with NBC.
Therefore, we evaluated the long-term efficacy and safety of endoscopic gastric variceal obliteration (GVO) with NBC to treat GVH. The efficacy, prevalence of complications, ability to predict rebleeding, and bleeding-related death rate were analyzed.
METHODS
Patients
Four hundred and fifty-five patients who were diagnosed with GVs and underwent variceal obliteration with NBC at Chonnam National University Hospital, Gwangju, Korea, from January 2004 to July 2013 were selected retrospectively. Patients diagnosed and treated at other institutions before referral to our center were excluded. The patients were followed until death or until July 2013. Patients' demographics, etiology of GV, Child-Pugh score, endoscopic findings, effectiveness of endoscopic treatment, and clinical and endoscopic follow-up were recorded and analyzed.
Endoscopic GV obliteration using NBC
Patients with upper gastrointestinal bleeding and features suggesting cirrhosis underwent upper endoscopy as soon as possible after admission (within 12 hours).
Endoscopy was performed using a forward-viewing endoscope (GIF Q 260, Olympus, Tokyo, Japan). Histoacryl (NBC) was prepared as follows: the injection needle was primed with water followed by a 1:1 mixture of Histoacryl and Lipiodol (Guerbet, Roissy, France). The varices, depending on their size, were injected with a bolus of 1 to 4 mL of the solution.
A disposable sclerotherapy needle (needle diameter, 2.3 mm; MTW, Endoskopie, Wesel, Germany) was used for injection. The catheter was introduced into the working channel of the endoscope and advanced. Following localization of the bleeding varix, the needle was exposed and inserted into the base of the varix, and an assistant injected the Histoacryl-Lipiodol mixture. After removal of the needle from the varix, the assistant injected normal saline to flush the remaining glue from the catheter. Both the endoscopist and endoscopy assistant used goggles as part of the universal precaution guidelines and to decrease the likelihood of accidental glue-induced damage to their eyes.
Definition
Active GVH was def ined as spurting or oozing of blood from a GV. Evidence of recent bleeding was defined as the presence of a white nipple or red plugs. GVs were categorized according to the classification system used by Sarin and Kumar [1]: a GOV type 1 (GOV1) appears as a continuation of esophageal varices (EVs), extending for 2 to 5 cm below the gastroesophageal junction whereas a GOV type 2 (GOV2) extends beyond the junction into the fundus of the stomach [1]. The morphology of the GV was classified according to the system proposed by Hashizume et al. [11]: tortuous (F1), nodular (F2), or tumorous (F3).
Successful initial hemostasis was defined as cessation of bleeding with no recurrence for 2 days [10]. Rebleeding was defined as bleeding related to esophageal and GVs, a new onset of hematemesis, coffee grounds vomitus, hematochezia, or melena, with a pulse rate > 100 beats per minute and blood pressure < 90 mmHg after a 24-hour period of stable vital signs and normal hemoglobin concentration [12]. Bleeding-related death was defined as any death within 6 weeks of the index bleeding [13].
Ethics statement
Written informed consent was obtained from all patients regarding the nature and the purpose of the treatment, and this study was approved by the Institutional Review Board of Chonnam National University Hospital.
Statistical analysis
Continuous variables are expressed as means ± standard deviation. Student t test and Pearson chi-square test were used to compare the baseline characteristics of the patients. Factors that were significant on univariate analysis were entered into a stepwise multivariate analysis to determine which risk factors retained statistical significance and which were merely dependent on other factors. Kaplan-Meier analysis was used to examine the cumulative survival and time to death and the log-rank test was used to compare differences between groups. Null hypotheses of no difference were rejected if p values were < 0.05, or equivalently, if the 95% confidence intervals of odds ratio estimates excluded one. We performed the statistical analysis using SPSS version 20.0 (IBM Co., Armonk, NY, USA).
RESULTS
Baseline characteristics
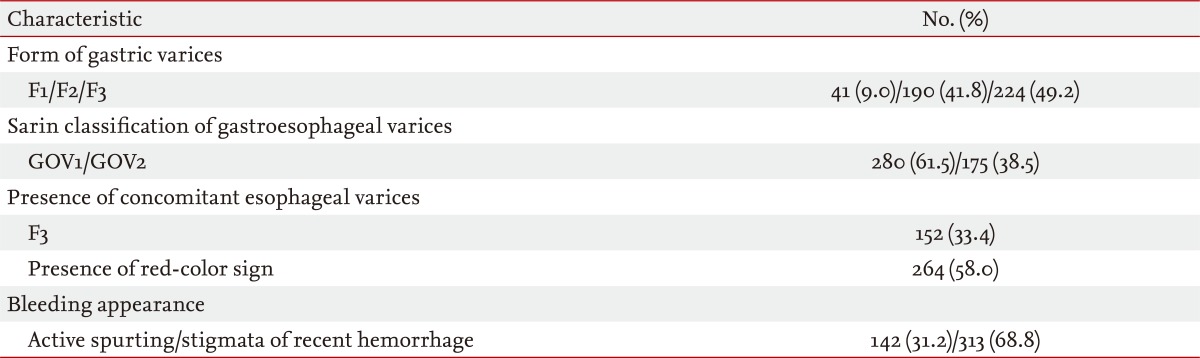
The baseline clinical characteristics and endoscopic findings of the enrolled patients are shown in Tables 1 and 2. The mean duration of follow-up was 582.8 days (range, 1 to 2,938). The mean age of patients was 57.65 years (range, 22 to 96). There were 379 males (83.3%) and 76 females (16.7%). One hundred and twenty-nine patients (28.4%) were positive for hepatitis B surface antigen (HBsAg), 33 (7.3%) were antibody-positive for hepatitis C virus, 217 (47.7%) were chronic alcohol drinkers, and 54 (11.9%) had a multifactorial liver disease. The patients' Child-Pugh classes were: A, 23.5%; B, 54.9%; and C, 21.5%. One hundred and eighteen patients (25.9%) had concomitant hepatocellular carcinoma (HCC). Two hundred and forty-seven patients (54.3%) had a previous history of variceal bleeding. The form of GVs was F1 in 41 patients (9%), F2 in 190 (41.8%), and F3 in 224 (49.2%). Two hundred and eighty patients (61.5%) had GOV1 and 175 (38.5%) had GOV2.
Results of sclerotherapy with NBC
The results of GVO with NBC are shown in Table 3. The overall success rate of initial hemostasis (no recurrent bleeding within 48 hours) was 96.9% (441/455). A mean dose of 1.02 ± 0.733 mL NBC was injected in each patient. Rebleeding occurred in 160 patients (35.2%) within 1 year. The bleeding-related death rate was 6.8% (31/455). Treatment-related complications occurred in 33.8% of patients (154/455).
Rebleeding according to liver function and classification of GVs
The rates of rebleeding for F1, F2, and F3 GVs were 10%, 41.9%, and 48.1%, respectively. The rate of rebleeding was 65.6% for patients with GOV1 and 34.4% for patients with GOV2. The rates of rebleeding were 23.4% for patients with Child-Pugh class A liver disease, 55% for patients with class B, and 21.5% for patients with class C.
Predictive factors for rebleeding according to time
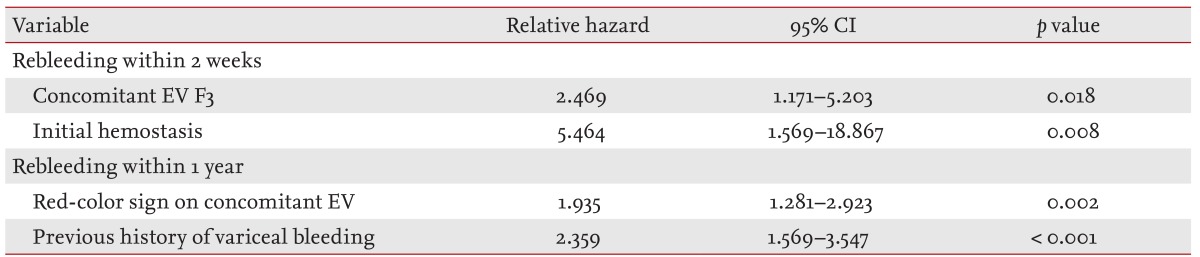
The analyses of potential predictive factors for rebleeding according to time are illustrated in Table 4.
Univariate analysis showed that concomitant F3 EV (p = 0.011) and failure of initial hemostasis (p = 0.004) were associated with rebleeding within 2 weeks. On multivariate analysis, concomitant F3 EV (p = 0.018) and failure of initial hemostasis (p= 0.008) were associated with rebleeding within 2 weeks.
Univariate analysis showed that concomitant F3 EV (p = 0.009), the red-color sign on concomitant EV (p = 0.001), serum sodium concentration < 135 mEq/L (p = 0.046), and a previous history of variceal bleeding (p < 0.001) were associated with rebleeding within 1 year. On multivariate analysis, the red-color sign on concomitant EV (p = 0.002) and previous history of variceal bleeding (p < 0.001) were associated with rebleeding within 1 year.
Cause of bleeding-related death
During the long-term follow-up, 31 patients (6.8%) died. Seventeen (54.8%) died of hepatic failure, nine (29%) of recurrent bleeding, three (9.7%) as a consequence of initial hemostasis failure, and two (6.5%) due to progression of HCC.
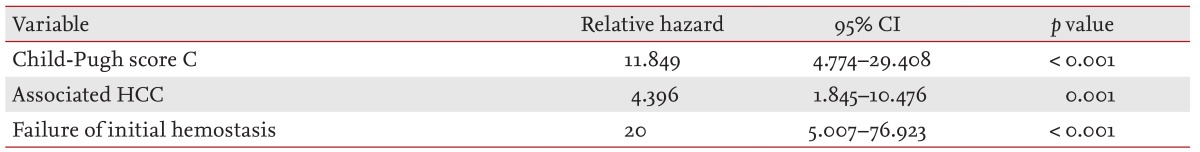
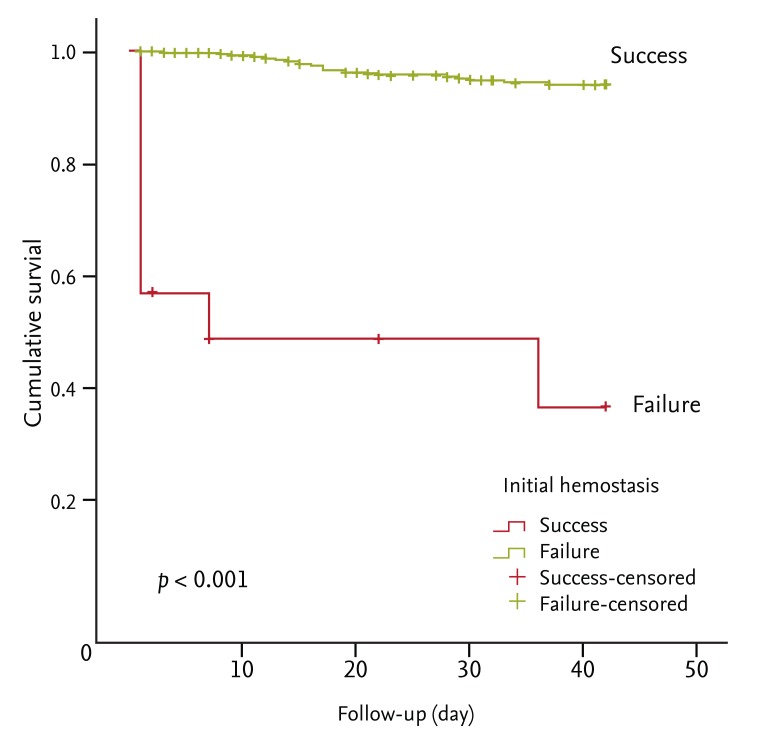
Predictive factors for bleeding-related death
An analysis of potential predicting factors for bleeding-related death is shown in Table 5 and Figs. 1,2,3. Univariate analysis showed that a red-color sign on concomitant EV (p = 0.018), the Child-Pugh score (p < 0.001), the model for end-stage liver disease (MELD) score ≥ 25 (p = 0.011), associated HCC (p < 0.001), and failure of initial hemostasis (p = 0.001) were associated with bleeding-related death. On multivariate analysis, the Child-Pugh score (p < 0.001), HCC (p = 0.001), and failure of initial hemostasis (p < 0.001) were associated with bleeding-related death.
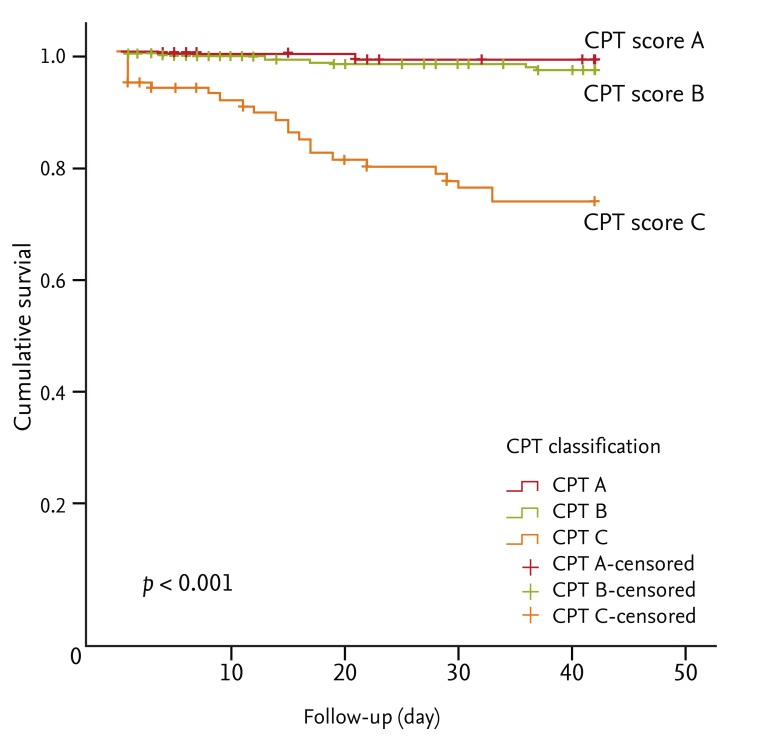
Kaplan-Meyer analysis of bleeding-related deaths according to Child-Pugh classification by log-rank test (p < 0.001). CPT, Child-Pugh-Turcott.
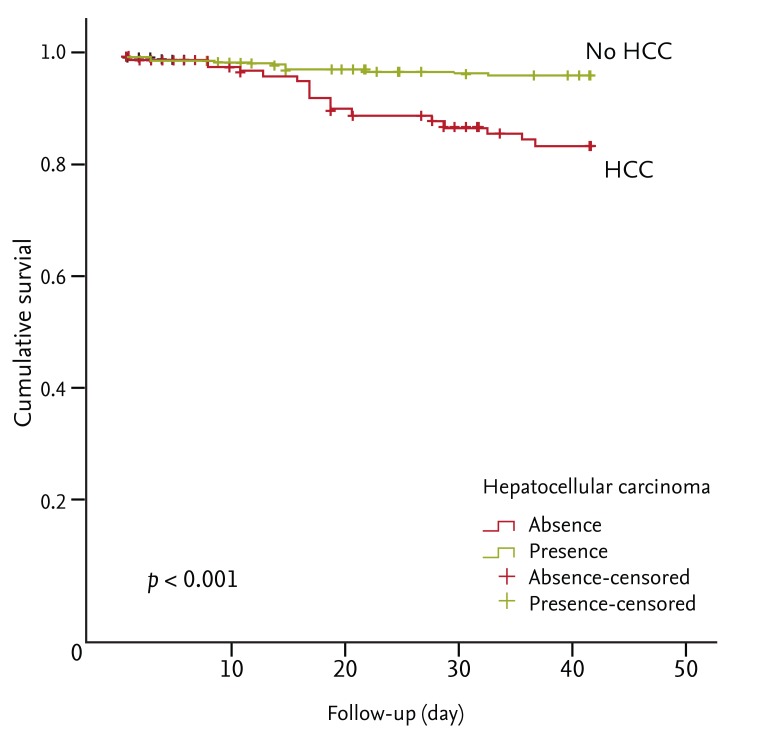
Kaplan-Meyer analysis of bleeding-related deaths according to the absence or presence of hepatocellular carcinoma (HCC) by log-rank test (p < 0.001).
DISCUSSION
The reported GVH-related mortality rate is ~30% in patients with portal hypertension [14,15]. Furthermore, GVH can cause bacteremia and spontaneous bacterial peritonitis, which can exacerbate decompensated liver function [16]. Therefore, prophylaxis and control of GVH are crucial for improving survival in portal hypertension patients. Although survival rates have improved, the bleeding related-mortality rate remains as high as 20% [17].
Hemorrhage from GVs is generally more serious and more often fatal than is hemorrhage from EVs [3]. Treatment of GVs is difficult, and the long-term efficacy and safety of the widely used NBC injection sclerotherapy have not been established. Although some recent studies have described the efficacy and safety of NBC sclerotherapy [8,9,10,18], a study involving a larger population of patients was required.
The present large retrospective study has demonstrated the long-term efficacy and safety of GVO using NBC for controlling GVH. The ability to obtain initial hemostasis, the low prevalence of serious complications, and the relatively favorable risk of rebleeding and bleeding-related death are all advantages of NBC sclerotherapy. The rate of initial hemostasis with NBC injection was 96.95%, which is consistent with the 90% to 97% reported by other studies [19,20,21].
Some studies have reported an early rebleeding rate of 0% to 28% within 48 hours [3,7,10] and rebleeding in 23.3% of patients from 3 days to 16 months after GVO [6]. Consistent with those reports, bleeding recurred in 5.3%, 6.8%, 12.7%, 27.5%, and 35.2% of our patients within 1, 2, 4 weeks, 6 months, and 1 year after NBC sclerotherapy, respectively. We also analyzed the predictive factors for rebleeding according to elapsed time after treatment, failure of initial hemostasis, and concomitant F3 EV within 2 weeks. A red-color sign on concomitant EV and previous history of variceal bleeding were associated with rebleeding within 1 year. Concomitant F3 EV and a red-color sign on concomitant EV were significant risk factors for acute and late rebleeding. Therefore, concomitant high-risk EV should be treated with prophylactic EV ligation after GVO as soon as possible. Inconsistent with other studies [3,19], we found that the size of GV, location of GV (GOV1 vs. GOV2), and Child-Pugh score were not associated with rebleeding. We hypothesized that this difference was associated with frequent rebleeding due to concomitant EV, which may act as a confounding factor. The Child-Pugh score was not associated with rebleeding but was related to bleeding-related death. According to one study [13], the 6-week mortality rate of uncontrolled GV bleeding is 25% to 30%. Another study found a mortality rate of 12.5% due to rebleeding immediately after NBC sclerotherapy [6]. After controlling GVH with NBC, the bleeding-related death rate in our study was 6.8%, which is consistent with the other reports [8,10].
The Child-Pugh score, concurrent HCC, and failure of initial hemostasis were most predictive of bleeding-related death. Some studies have shown that the Child-Pugh score and associated HCC are risk factors for bleeding-related death [6,22,23], while another study reported that MELD score is a risk factor [24,25]; our study showed these relationships only on univariate analysis.
Treatment-related complications occurred in 34.1% of our patients, a result comparable to previous reports. Our study had several limitations. First, it was a retrospective single-center study, so the results may not be generalizable to other patient populations. Second, follow-up endoscopy was not performed in all patients.
In conclusion, NBC injection for treatment of GVH is a highly effective (96.9%) and safe method of achieving primary hemostasis. The complication rate was 33.8%, but most complications were not serious.
Concomitant F3 EV and red-color sign on concomitant EV were significant risk factors for acute and delayed rebleeding. Therefore, concomitant high-risk EV should be treated with prophylactic EV ligation after GVO as soon as possible.
The Child-Pugh score, concurrent HCC, and failure of initial hemostasis were significantly associated with the bleeding-related death rate.
This study provides a comprehensive overview of the survival outcomes and prognostic factors of patients with GVH in a single center. The results may help physicians to select an effective treatment strategy for patients with GVH.
KEY MESSAGE
The rate of initial hemostasis of gastric variceal obliteration using N-butyl-2-cyanoacrylate in patients with gastric variceal hemorrhage was 96.9%; rebleeding occurred in 35.2% of patients, and the bleeding-related death rate during the follow-up was 6.8%.
Rebleeding occurred in 35.2% of patients within 1 year. Concomitant F3 esophageal varice (EV) and failure of initial hemostasis were associated with rebleeding within 2 weeks. Concomitant EV, red-color sign, association with hepatocellular carcinoma (HCC), and previous history of upper gastrointestinal bleeding were associated with rebleeding within 1 year.
Predictors for bleeding-related death were the Child-Pugh score, association with HCC, and failure of initial hemostasis.
Acknowledgments
This study was supported by grants from Chonnam National University Hospital, Gwangju, Korea.
Notes
No potential conflict of interest relevant to this article was reported.