Unusual cause of back pain in a 13-year-old boy: a thoracic osteoblastoma
Article information
A 13-year-old boy was referred to Chosun University Hospital for evaluation of inflammatory back pain. He had previously been healthy but complained of persistent back pain and an unsteady gait commencing several months prior. The pain did not respond to medical treatment and buttock discomfort developed. His motor power was intact and he was able to walk without any assistance. A physical examination revealed pain on percussion of the T4 spinous process, reduced sensation below the T5 level, increased muscle tone, positive ankle clonus, and positive Babinski signs. Computed tomography revealed an aggressive osteolytic lesion at the T4 vertebral body, with posterior extensions (Fig. 1A and 1B). Magnetic resonance imaging (MRI) revealed a relatively well-defined, soap bubble-like mass lesion at the T4 level (Fig. 1C). T2-weighted MRI images showed severe anterior displacement and compression of the spinal cord at the T4 level (Fig. 1D). He underwent emergency decompressive surgery and marginal excision of the tumor via T3-T5 laminectomy. Histopathological examination revealed reactive woven bone, fibroblasts, and osteoclast-like giant cells; these findings were consistent with osteoblastoma (Fig. 2). The thoracic pain and numbness of the lower extremities resolved immediately after surgery. He was transferred to the oncology department to undergo radiotherapy.
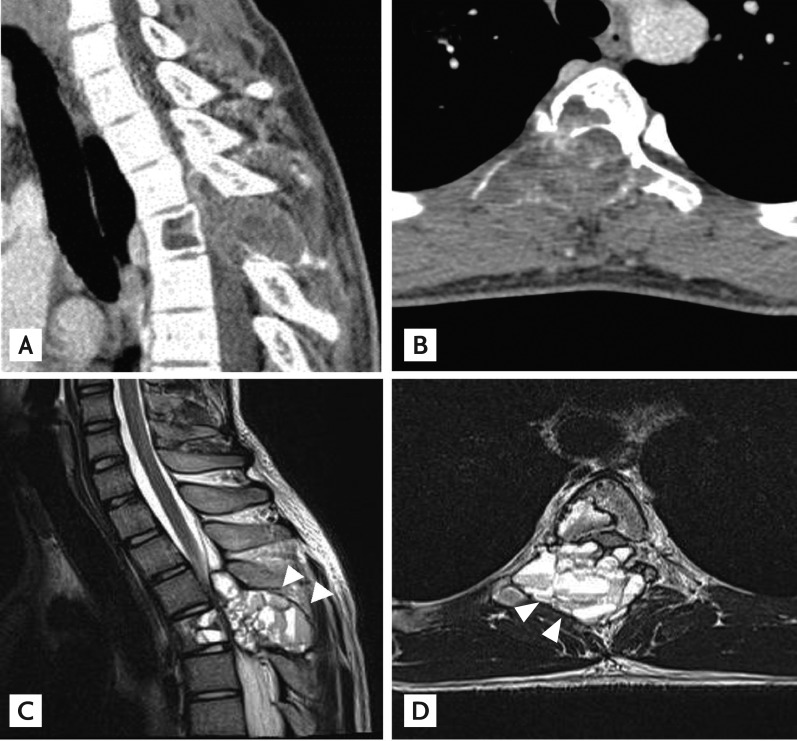
(A) A preoperative computed tomography scan reveals osteolytic destruction of the T4 vertebral body. (B) An axial scan shows a destructive mass involving both the anterior and posterior elements. (C) Sagittal T2-weighted magnet ic resonance imaging (MRI) reveals severe spinal cord compression attributable to the well-defined, soap bubble-like epidural mass with the traditional fluid-fluid level sign (arrowheads). (D) Axial T2-weighted MRI shows a well-delineated epidural mass featuring anterior displacement and compression of the spinal cord at the T4 level (arrowheads).
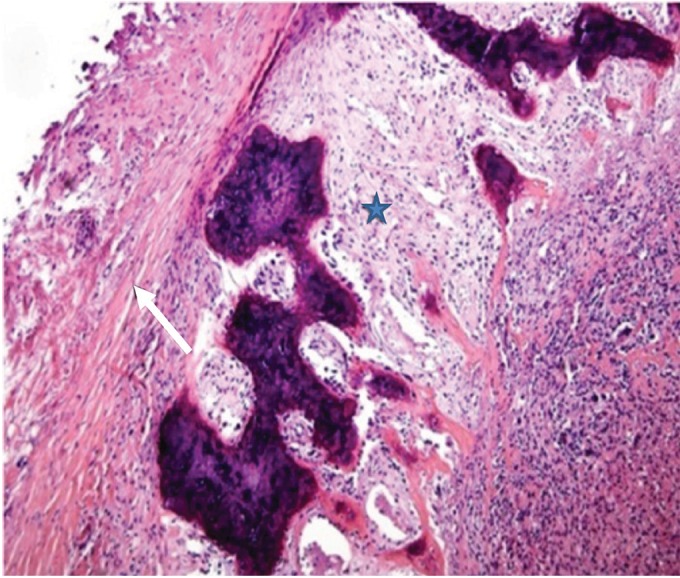
Histopathological examination shows spaces separated by fibrous septa (arrow) and reactive woven bone, fibroblasts, and osteoclast-like giant cells (star), consistent with an osteoblastoma (H&E, ×100).
An osteoblastoma is a rare, benign bone neoplasm comprising fewer than 1% of primary bone tumors. The tumor tends to form expansible masses, and exhibits high growth potential. An osteoblastoma can undergo malignant transformation. When osteoblastomas involve the spine, the tumors generally affect the posterior elements, and occur only rarely in the thoracic spine, to cause back pain (for example, in the young male whom we treated). Although osteoblastoma of the thoracic spine is considered to be an extremely rare cause of back pain, the tumor can aggressively involve a vertebral body, even in a young male.
Notes
No potential conflict of interest relevant to this article was reported.