Two dislodged and crushed coronary stents: treatment of two simultaneously dislodged stents using crushing techniques
Article information
Abstract
Coronary stent dislodgement is a rare complication of percutaneous coronary intervention. We report a rare case of dislodgement of two intracoronary stents. On withdrawal of two balloon catheters, one with a guide wire was mechanically distorted from the left main (LM) to the proximal left anterior descending artery (LAD) while the other was dislodged from the LM to the ostial left circumflex artery. The stent in the LAD could not be retrieved into the guide catheter using a Goose neck snare, because it was caught on a previously deployed stent at the mid LAD. A new stent was quickly deployed from the LM to the proximal LAD, because the patient developed cardiogenic shock. Both stents, including a distorted and elongated stent, were crushed to the LM wall. Stent deployment and crushing may be a good alternative technique to retrieving a dislodged stent.
INTRODUCTION
Drug eluting stents are currently utilized in the majority of percutaneous coronary intervention (PCI) procedures because they decrease restenosis and cause revascularization. A rare but serious complication of stents is dislodgement, which can lead to embolization, emergency coronary bypass graft surgery, or even death [1,2]. Stent dislodgement is more likely in lesions that are severely calcified and significantly angulated [3-5]. The incidence of stent dislodgement during PCI appears to have decreased in recent years, probably due to improved equipment design and to the almost universal use of premounted stents. Retrieval of a dislodged stent can be performed either percutaneously or surgically [6]. Various devices have been used, such as a small balloon catheter, a snare loop, grasping forceps, and basket retrieval devices [7-9]. If stent retrieval is not possible, crushing the stent against the wall is the alternative technique to prevent embolization [1,10]. We report an extremely rare case in which two intracoronary stents became simultaneously dislodged. One remained distorted and elongated from the proximal left anterior descending artery (LAD) through the left main (LM) to the ascending aorta, while the other was crushed from the LM wall to the left circumflex artery (LCX) ostium.
CASE REPORT
A 58-year-old female patient was admitted to the cardiology department due to a 7-day history of chest pain. She had hypertension but electrocardiography was normal and cardiac enzymes were in the normal range. Left coronary angiography performed via the left radial artery showed irregular significant tubal stenosis of the mid LAD, tubular 50% narrowing of the LM, severe stenosis of the ostial LAD, and narrowing of the ostial left circumflex coronary artery (Fig. 1A and 1B). Right coronary angiography showed no significant narrowing of the right coronary artery (Fig. 1C). We recommended off-pump coronary artery bypass (OPCAB) for the LAD lesion and we planned to undergo PCI in the LCX lesion after OPCAB. Five days later, she underwent OPCAB, in which anastomoses were formed of the left internal mammary artery (LIMA) to the first diagonal branch (D1), and the right internal mammary artery (RIMA) to the distal LAD. Seven days postoperatively, follow-up coronary angiography revealed intact graft flow from the RIMA to the distal LAD, (Fig. 2A), but completely occluded graft flow from the LIMA to the D1 (Fig. 2B). Therefore, PCI was planned for the LM, the ostial and mid LAD, and the ostial LCX. A 7 Fr extraback-up (EBU) guiding catheter (Medtronics, Santa Rosa, CA, USA) was engaged at the ostium of the LM. Runthrough wires (Termo, Tokyo, Japan) were placed in the distal LAD and LCX. Initially, a 3.0 × 15 mm Xience stent (Abbott Vascular, Santa Clara, CA, USA) was implanted in the mid LAD (Fig. 3A). Using a 2.5 × 15 mm Ryujin balloon (Termo), ostial segments of the LCX and LAD were alternatively dilated. Next, we used minicrush techniques. First, a 2.5 × 12 mm Xience stent was positioned in the proximal LCX more distally and was then pulled back to the point that the proximal marker of the LCX stent contacted the body of the main vessel stent. A 3.5 × 23 mm Xience stent was then introduced into the distal LM to the proximal LAD to overlap the mid LAD stent. However, it could not be delivered to the target lesion despite multiple attempts to advance the stent distally. We felt that further aggressive dilation was required. When we attempted to retrieve the stents into the guide catheter, both stents simultaneously detached from the stent balloons and two guide wires were placed in the center of the stents (Fig. 3B). We initially planned to retrieve the dislodged stent in the LM to the proximal LAD using a 5 mm Gooseneck snare (St. Jude Medical, Sylmar, CA, USA). After the stent was successfully snared, we retracted the snare without removing the whole system, because the other stent had dislodged in the LM to the ostial LCX. When we retracted the snare, the stent was distorted and elongated into the guide catheter, preventing withdrawal using the guide catheter. At that time the patient was stable, so we decided to remove the two dislodged stents surgically. When the entire system including the guide catheter and wires were removed, the stent remained from the LM to the ascending thoracic aorta (Fig. 3C). Later the patient developed severe chest pain, which was followed by cardiogenic shock. Immediately, another 7 Fr EBU guiding catheter was engaged at the ostium of the LM and coronary angiography showed nearly total occlusion at the distal portion of the LM with thrombolysis in myocardial infarction 1 flow due to an intracoronary thrombus (Fig. 4A). The ostial segment of the LAD was dilated using a 2.5 × 15 mm Ryujin balloon to 8 atmosphere (atm) and a new 3.5 × 23 mm Xience stent was introduced into the mid LM to the proximal LAD across the LCX lesion and deployed (Fig. 4B), restoring the blood pressure to 125/75 mmHg. After a new Pilot wire (Abbott Vascular) was placed in the distal LCX, the ostial LCX was additionally dilated using a 2.5 × 15 mm Ryujin balloon to 14 atm. Although the blood flow in the distal LCX was slightly decreased due to dissection by the guide wire, the final result on coronary angiography was good (Fig. 4C). Subsequently, both stents, including the distorted and elongated stent, were crushed to the LM wall (Fig. 4D). Five days postoperatively, the patient was discharged in stable condition on triple antiplatelet agents including cilostazol. Six months later, she presented with chest pain and mild dyspnea, so coronary angiography was repeated, which showed no evidence of restenosis or progressive disease (Fig. 5).

(A) A diagnostic coronary angiography showed irregular significant tubular stenosis of the mid left anterior descending artery (LAD) in the anterior posterior (AP) cranial view and (B) tubular 50% narrowing of the left main, severe stenosis of the ostial LAD and narrowing at the ostial left circumflex artery in the right anterior oblique caudal view. (C) Right coronary angiography showed no significant narrowing of the right coronary artery in the AP cranial view.
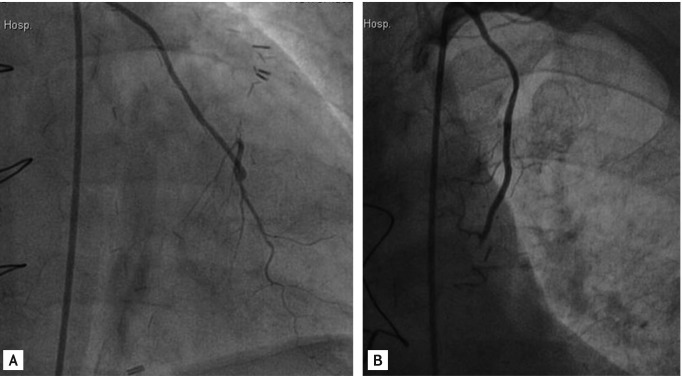
(A) Following coronary artery bypass graft, follow-up coronary angiography revealed that graft flow from the right internal mammary artery to the distal left anterior descending artery was intact in the anterior posterior (AP) view, (B) but graft flow from the left internal mammary artery to the D1 (the first diagonal branch) was totally occluded in the AP view.
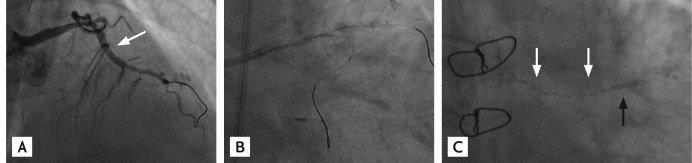
(A) A 3.0 × 15 mm Xience stent (white arrow) was implanted in the mid left anterior descending artery, anterior posterior (AP) cranial view. (B) Both stents were totally detached from the stent balloons, AP caudal view. (C) When the entire systems were removed, one stent (white arrows) remained from the left main (LM) to the ascending thoracic aorta and the other stent (black arrow) remained in the shaft of the LM, AP caudal view.

(A) When cardiogenic shock developed, coronary angiography showed total occlusion at the distal portion of left main (LM) with thrombolysis in myocardial infarction 1 flow, anterior posterior (AP) caudal view. (B) A new 3.5 × 23 mm Xience stent (white arrow) was deployed from the mid LM to the proximal left anterior descending artery (LAD) across the ostium of the left circumflex artery (LCX), right anterior oblique (RAO) caudal view. (C) After the ostial LCX was dilated using a 2.5 × 15 mm Ryujin balloon, coronary angiography showed slightly decreased blood flow in the distal LCX and totally recovered blood flow in the distal LAD in the RAO caudal view. (D) A new 3.5 × 23 mm Xience stent (black arrow) was used to crush the two dislodged stents (white arrows) to the LM wall, AP view.

A 6-month follow-up coronary angiography showed no evidence of restenosis or progressive disease, (A) right anterior oblique caudal view and (B) anterior posterior caudal view. (C) The previously dislodged and crushed stents (white arrows) remained and the previously deployed stent (black arrow) from the mid left main to the proximal left anterior descending artery was intact, left anterior oblique view.
DISCUSSION
The incidence of stent dislodgement ranges between 0.3% and 8%, although this has markedly decreased due to the technological advancement of stent mounting [1,2]. Dislodgement of a stent can be secondary to extreme coronary angulation, highly calcified coronary arteries, inadequate coronary artery predilation, direct stenting, and interference by a previously deployed stent [3-5]. In this case, the stent was dislodged due to interference with the previously deployed stent at the mid LAD, not due to inadequate predilation or a severely calcified coronary artery, because the previous stent had been easily delivered to the target lesion in the mid LAD. Percutaneous stent retrieval can be successfully performed using various techniques, including a small-balloon technique, a double-wire technique, or a loop snare [7,8]. The snare loop is relatively safe and easy to use, has a low rate of complications, and appears to be very effective [9]. If stent retrieval is not possible, a new stent can be used to crush it against the vascular wall, thereby preventing migration [10]. In our case, the dislodged stent could not be retrieved using a snare loop, although the stent was successfully snared. Because cardiogenic shock developed and coronary angiography showed nearly total occlusion at the distal LM, a new stent was deployed. Crushing dislodged stents against the vessel wall is an important alternative strategy that is not as problematic as is generally thought, but the long term safety of this technique in the LM coronary artery has not been sufficiently documented. Therefore, a 1-year follow-up coronary computed tomography angiography will be performed to assess location of the distorted stent. Although stent dislodgement is rare, thanks to the development of improved devices, it is still a very serious problem in interventional cardiology because stent embolization or acute thrombotic events are usually fatal. Stent dislodgement can occur due to arterial tortuosity and calcification, direct stenting, or the inadequate coaxiality of the guide catheter; therefore, adequate predilation may help to prevent stent dislodgement. Also, when resistance is felt during undeployed stent withdrawal, removal of the entire system may help to prevent stent dislodgement. An interventional cardiologist should be well aware of various emerging retrieval techniques.
Notes
No potential conflict of interest relevant to this article is reported.