Intracardiac foreign body caused by cement leakage as a late complication of percutaneous vertebroplasty
Article information
To the Editor,
Percutaneous vertebroplasty (PVP) is a simple, convenient, and minimally invasive procedure for the management of back pain and spinal instability associated with osteoporotic compression fractures and other osteolytic spinal lesions [1]. Although very rare, cement leakage into the spinal canal or the vascular system has been reported as a troublesome late complication. In this report, we present a case of a foreign body in the heart revealed by transthoracic echocardiography and removed by open heart surgery.
A 75-year-old female patient was admitted for evaluation of progressively worsening dyspnea for 2 months. However, there was no medical history of dyspnea and intermittent palpitation, because she had been fairly active without diff iculty 2 months prior to admission. On examination, her vital signs were blood pressure 110/70 mmHg, heart rate 148 beats/min, respiratory rate 20 breaths/min, and body temperature 37.3℃. Physical examinations were unremarkable. Electrocardiography revealed atrial flutter with rapid ventricular response, whereas it had shown normal sinus rhythm 4 years prior to admission. Chest radiography showed an increased cardiothoracic ratio with mild pulmonary vascular congestion; in addition, radiographic high density was noted in the third lumbar vertebral body (Fig. 1A). With respect to her past medical history, she had undergone PVP at the level of the third and fourth lumbar spine 5 years previously for chronic back pain and had been asymptomatic since that time.

(A) Chest radiography shows the high density (arrows) of the 3rd lumbar vertebral body. (B) Coronary view in the chest computed tomographic scan shows linear high attenuating material (arrow heads) in the right atrium.
Transthoracic echocardiography exhibited severe global decreased wall motion abnormalities of the left ventricle (LV), poor systolic function (ejection fraction [EF], 27%), with rapid heart rate (136 beats/min) and normal LV end-diastolic dimension of 4.6 cm and dilated left atrium (LA) of 4.6 cm. However, moderate-to-severe tricuspid insufficiency (pulmonary artery systolic pressure [PASP], 57 mmHg) was noted, while there were no evidence of LA thrombus or pericardial effusion. Moreover, a calcified linear structure (approximately 6 cm), which was also conf irmed by chest computed tomography (CT) (Fig. 1B), was found in the right atrium (RA) and right ventricle (RV). It was anchored in the RA adjacent to the inferior vena cava opening, passed through the tricuspid valve, and reached around the posterior wall of the RV outflow tract (Fig. 2). As a result of malcoaptation of the tricuspid valve caused by the linear structure passing through the tricuspid opening, a laterally directed eccentric jet flow of moderate-to-severe tricuspid insufficiency was demonstrated. With regard to the increased pulmonary artery pressure, any pulmonary complications of foreign body embolism could not be found by chest CT.
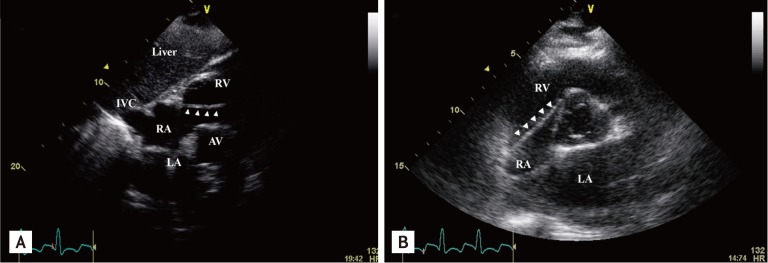
(A) In the subcostal view, the foreign body (arrow heads) is attached to right atrium (RA) near the opening site of inferior vena cava. (B) Parasternal short axis view reveals that the echogenic linear structure (arrow heads) in the RA passed through the tricuspid valve and advanced into the right ventricle (RV). LA, left atrium; IVC, inferior vena cava; AV, aortic valve.
The patient had commenced diuretics with furosemide (increased to 80 mg daily) and β-blockers with carvedilol (up to 12.5 mg twice daily) for dyspnea and atrial flutter. The symptoms of chest discomfort and dyspnea seemed to be related at least in part to the foreign body in the heart. We considered the foreign body in the RA and RV to be a potential source of pulmonary thromboembolism or infarction in the near future and thus recommended surgical removal, even if the etiology of the clinical symptoms was not entirely correlated with the foreign body. Surgical findings revealed that the 6 cm long linear intracardiac foreign body was a calcified and fragile material (Fig. 3), and that it was attached to the confluence site of the inferior vena cava and RA, and reached to the RV. The foreign body was excised at its attachment, preserving the tricuspid valve.

(A) Operation photograph showing a linear material (arrowheads) in the right ventricle and right atrium. (B) Photograph of gross specimens showing cement materials that were removed from right atrium and ventricle; foreign body was broken into two pieces.
On follow-up echocardiography, systolic function was not much improved (EF 33%); however, the severity of tricuspid regurgitation was decreased from moderate to mild. The patient subsequently became free from dyspnea and chest discomfort, while atrial flutter remained.
After discharge, she visited the outpatient clinic regularly for management of heart failure.
PVP is an effective, minimally invasive procedure used mainly for the treatment of vertebral fractures in osteoporosis and metastasis. During the procedure, polymethylmethacrylate is injected into the lesion of the vertebral body, and organizes within a short time. Complications after PVP include bleeding at the puncture site, inaccurate needle placement, pain exacerbation, local infection, leakage of polymethylmethacrylate cement into the spinal canal or paravertebral tissues, perivertebral venous leakage, and pulmonary embolism [2]. There is always a risk of cement migration into the vena cava, which may result in pulmonary embolism. Vasconcelos et al. [3] have reported an incidence of 16.6% for minor passage of cement into perivertebral veins, including one case in which a minute amount of cement reached the inferior vena cava. Other cases have reported multiple cardiac perforations after PVP [4].
Usually, symptoms or signs of cement leakage complications occur during, immediately or within several months after the procedure. However, in the present case, the foreign body could not enter the pulmonary circulation because of the length and rigid nature of the material; otherwise, there would have been catastrophic complications. Thus, we speculated that the pathological process of heart failure progressed gradually, taking 5 years for the clinical manifestation of dyspnea to become apparent.
As regards the cause of heart failure, there was a possibility of acute exacerbation of chronic heart failure, and some explanations seem possible. Other than the conventional risk factors, such as old age, hypertension and diabetes, the shortening of ejection time or diastolic relaxation time in rapid heart rate could cause heart failure, such as tachycardia-induced heart failure [5], as is frequently seen in patients with atrial flutter or fibrillation. Although the foreign body might have increased tricuspid insufficiency, it was not the only cause of the heart failure. In other words, we do not know the cause of the aggravation of dyspnea. However, in this case, the symptom improved after heart rate control. The foreign body could increase PASP and tricuspid insufficiency severity. High pulmonary artery pressure can be caused by left heart failure. The foreign body was not solely responsible for dyspnea and could not have been an immediate cause of dyspnea. When the cause of heart failure is unknown, the symptom may be attributed to tricuspid insufficiency exacerbated by a foreign body, although pharmacological treatments such as diuretics and digoxin are used in heart failure. A definite relationship between the foreign body and atrial flutter with tricuspid insufficiency leading to heart failure could not be demonstrated in the present case. Although the foreign body was found incidentally, it might have been the source of pulmonary thromboembolism, valvular heart disease, or cardiac perforation in the near future. Because of the jamming caused by the linear structure in the tricuspid valve, we assumed that the heart failure with atrial flutter in our patient could be partly attributed to the foreign body; this is supported by the patient's clinical course after removal of the foreign body. Thus, given the deleterious effects of a foreign body on cardiovascular complications, surgical removal of the foreign body should be performed.
Here, we report a foreign body in the RA and RV complicating PVP 5 years previously. In this case, we exerted effort to prevent complications arising due to the foreign body. It is important to consider the possibility of late manifestation of complications; a high index of suspicion is also required in patients who have a cardiac foreign body, especially those with a history of PVP.
Notes
No potential conflict of interest relevant to this article is reported.