Trismus in cephalic tetanus from a foot injury
Article information
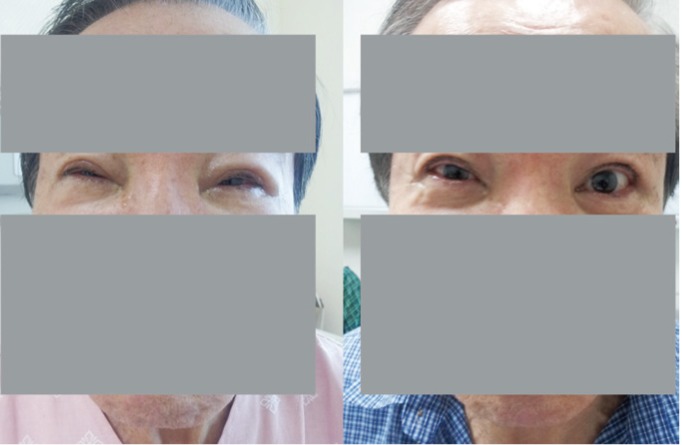
A 65-year-old man presented complaining of progressive inability to open his mouth and eyes and difficulty swallowing that had begun 20 days earlier. He had sustained a penetrating injury to his left foot caused by scissor tips approximately 6 weeks earlier. The foot injury was clean and had healed. His vital signs were stable without fever. The white blood cell count and C-reactive protein were within normal limits. His primary tetanus vaccination status was unclear. Magnetic resonance imaging and magnetic resonance angiography of the brain were normal. The patient was diagnosed with cephalic tetanus based on his history of penetrating injury, intense trismus, facial nerve paralysis, and exclusion of an alternative diagnoses. Treatment was initiated with tetanus immunoglobulin (HTIG, 500 U), metronidazole (500 mg q8h), and diazepam (10 mg q8h). Over the next 14 days, his rigidity improved slowly, and he was able to open his mouth (Fig. 1) and eyes (Fig. 2).
Tetanospasmin, an exotoxin produced by Clostridium tetani, is the cause of tetanus. Cephalic tetanus is a rare form of localized tetanus and almost always occurs only following craniofacial injuries. This case developed after injury to an area remote from the head, which explains the relatively long incubation period. Treatment involves wound debridement, adequate active and passive immunization, antibiotics, benzodiazepines, and aggressive supportive care. Passive immunization with HTIG at a lower dose (500 U) appears to be as effective as a higher dose (10,000 U). About two-thirds of cephalic tetanus progress to generalized tetanus with a poor prognosis.
When a patient presents with trismus and paralysis of one or more cranial nerves, cephalic tetanus should be included in the differential diagnosis. A remote, healed peripheral injury can be a source of cephalic tetanus.
Notes
No potential conflict of interest relevant to this article is reported.