Concurrent Parathyroid Carcinoma and Hyperplasia in Hyperparathyroidism
Article information
To the Editor,
Parathyroid carcinoma is a rare disease that accounts for less than 1% of all hyperparathyroidism [1]. The incidence of parathyroid carcinoma is extremely low, although the apparent incidence of hyperparathyroidism increased after the introduction of multi-channel auto-analyzers. If increased serum calcium and parathyroid hormone (PTH) levels are sustained postoperatively, metastatic lesions should be suspected [2]. Here, we report a case in which high serum calcium and PTH levels were sustained after resection of a parathyroid carcinoma and a final diagnosis of concurrent parathyroid carcinoma and hyperplasia was made.
A 74-year-old woman was referred to our hospital following loss of consciousness. She had a 4-year history of severe back pain and was diagnosed with spinal stenosis. Despite medical treatment, her back pain persisted. At presentation, she was stuporous and her blood pressure was undetectable. Mechanical ventilation was started and vasopressors administered. Laboratory results included a serum calcium of 17.7 mg/dL and PTH of 713.9 pg/mL. Computed tomography (CT) revealed a left thyroid mass.
Ultrasonography revealed a left parathyroid mass (Fig. 1A). A sesta technetium-99m methoxyisobutylisonitrile (99mTc-sestamibi) scintigram revealed no abnormal uptake (Fig. 2). The patient regained consciousness after intravenous hydration and calcitonin treatment. One month later, she underwent a left parathyroidectomy and hemithyroidectomy. Parathyroid carcinoma with capsular invasion was confirmed histologically (Fig. 3). Given her unstable vital signs intraoperatively, the surgeon could not explore the right thyroid gland accurately.
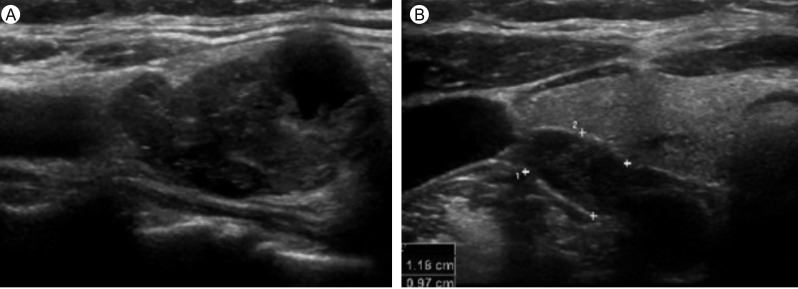
Thyroid ultrasonographic-findings. (A) A 2.8 × 1.5-cm, polymorphic, ill-defined, inhomogenous, and hypoechoic mass is noted in the lower portion of the left lobe of the thyroid gland. (B) A 1.1 × 0.6-cm, oval, well-defined, inhomogenous, and hypoechoic parathyroid gland is noted in the lower portion of the right lobe of the thyroid gland.

Technetium (99mTc)-sestamibi scan. (A) A 15-minute scan after 99mTc-sestamibi injection shows normal thyroid uptake. (B) A 2-hour scan after 99mTc-sestamibi injection shows no parathyroid uptake.
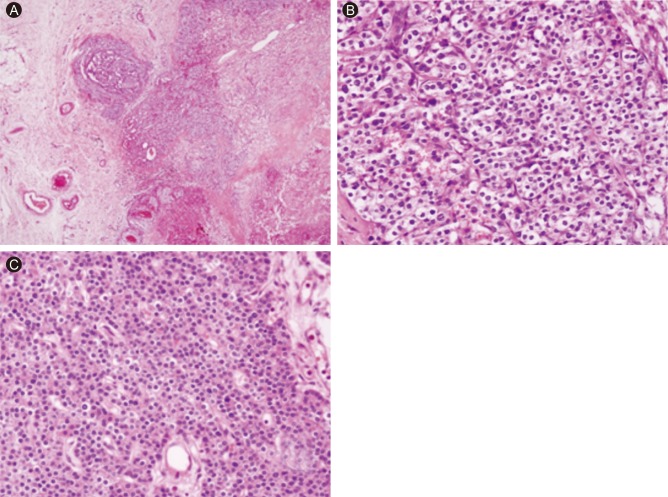
Light microscopic findings. (A) Capsular invasion with extension into the adjacent soft tissue (H&E, × 40). (B) Trabecular growth, clear cytoplasm, an atypical nucleus with atypical mitosis are seen (H&E, × 400). (C) Monotonous cell proliferation without an atypical nucleus or capsulation (H&E, × 400).
The elevated serum calcium and PTH levels decreased after resecting the left parathyroid carcinoma, but were still elevated compared to normal. To detect remnants or metastatic lesions, f luorodeoxyglucose positron emission tomography was performed, but no abnormalities were found. Ultrasonography detected a mildly enlarged parathyroid gland on the right inferior side, which had previously been very small (Fig. 1B). She underwent surgical exploration of the right parathyroid glands 1 month later. The right superior parathyroid gland was of normal size and histology and was preserved. In contrast, the right inferior parathyroid gland was mildly enlarged with grossly normal morphology, but hyperplasia was confirmed histologically (Fig. 3C). Ultimately, three parathyroid glands were removed and the serum calcium and PTH levels dropped to 8.1 mg/dL and 14.8 pg/mL, respectively.
The etiology of parathyroid carcinoma is still unknown. There have been several reports on concurrent disease in the other parathyroid glands, such as carcinoma, adenoma, or hyperplasia [3]. These reports suggest that parathyroid adenoma and hyperplasia may change into carcinoma. However, the findings are controversial due to the low incidence [4].
Primary hyperparathyroidism usually involves slightly elevated hypercalcemia (to 1 mg/dL), while parathyroid carcinoma produces much higher serum calcium levels (> 14 mg/dL) [1]. The laboratory findings suggested that our patient had a parathyroid carcinoma. The skeletal system involvement is greater in parathyroid carcinoma, and includes hyperparathyroid bone disease. In contrast, the skeletal system is involved in 5% of patients with benign hyperparathyroidism [2]. Although our patient was diagnosed with spinal stenosis before her presentation, it is possible that her back pain was induced by parathyroid carcinoma. On physical examination, a mass in the parathyroid area of the neck is an important sign for distinguishing between adenoma and carcinoma of the parathyroid gland, because it occurs in 30% to 76% of all parathyroid carcinomas. Although the laboratory results and clinical symptoms and signs can help distinguish between benign and malignant tumors, a definitive diagnosis is difficult preoperatively. Histological differences are useful for the differential diagnosis, such as the criteria for malignancy proposed by Schantz and Castleman [4]: 1) the presence of a trabecular growth pattern, mitotic figures, and capsular or vascular invasion; and 2) the presence of nodal or distant metastasis. Recently, loss of parafibromin immunostaining helped with the differential diagnosis of parathyroid carcinomas from adenomas in Asians and may serve as a prognostic marker in patients with parathyroid carcinomas [5]. In our case, the left parathyroid mass exhibited capsular invasion with extension into the adjacent soft tissue and trabeculum, clear cytoplasm, and atypical nuclei with atypical mitoses, suggesting carcinoma. In contrast, the right inferior parathyroid gland exhibited monotonous cell proliferation without atypical nuclei and capsulation, suggesting hyperplasia.
The most effective treatment of parathyroid carcinoma is complete removal of the primary lesion during surgery [1,5]. If patients with benign adenomas or hyperplasia are suspected of having concurrent parathyroid carcinoma, the surgeon should explore all four parathyroid glands. If the frozen pathology suggests cancer or the quick intact PTH levels do not decrease significantly after mass removal, all lesions on the same side of the thyroid lobe and any suspicious tissues around the lesions should be removed. In our patient, all lesions on the left side were removed, but the right side was explored later because CT, ultrasonography, and 99mTc-sestamibi scintigraphy revealed that the right parathyroid gland was normal and the surgeon could not continue the operation as the patient's vital signs deteriorated.
Serum calcium and PTH levels are useful for postoperative follow-up because normal levels indicate successful surgery. If patients have elevated serum calcium and PTH levels, additional action should be taken to localize remnant or metastatic lesions. 99mTc-sestamibi scintigraphy may be useful for localizing parathyroid tumors, including benign and malignant lesions, although no abnormal uptake was detected with both the parathyroid carcinoma and hyperplasia in our patient.
Parathyroid carcinoma is rare and its concurrence with different pathologies in the other parathyroid glands is extremely rare. Because the elevated postoperative serum calcium and PTH levels suggested remnant or metastatic lesions, additional action was taken. In our patient, the elevated serum levels returned to normal after surgical removal of another parathyroid gland. Parathyroid hyperplasia was confirmed histologically. In this case, we were unable to evaluate the other parathyroid glands during the first operation; nevertheless, no abnormal findings appeared during either the first-look operation or during subsequent imaging studies, including CT, 99mTc-sestamibi scintigraphy, and ultrasonography. We believe that the postoperative serum calcium and PTH levels are very useful for detecting not only remnant or metastatic parathyroid lesions, but also concurrent parathyroid hyperplasia or adenoma.
Notes
No potential conflict of interest relevant to this article is reported.