Coronary Artery Intervention after Cytostatics Treatment in Unstable Angina Patient with Essential Thrombocythemia. A Case Report and Literature Review
Article information
Abstract
Essential thrombocythemia (ET) is a clonal disorder of myeloid stem cells that causes thrombocytosis. As a result, ET can lead to vascular thrombosis and tissue ischemia; the association of coronary artery abnormalities such as myocardial infarction or unstable angina is rare. Here we describe a 45-year-old male patient with essential thrombocythemia who presented with unstable angina. Elective coronary angiography showed total occlusion of mid right coronary artery and mid left anterior descending coronary artery. ET was confirmed by a bone marrow biopsy; treatment was started with antiplatelet therapy including aspirin and clopidogrel along with cytostatic therapy with hydroxyurea and anagrelide. After the initiation of the treatment, the platelet count decreased to 20×104/µL. In addition, percutaneous coronary angioplasty was successfully performed with stent placement at the right coronary artery without hemorrhagic or thrombotic complications.
INTRODUCTION
Essential thrombocythemia (ET) is a chronic myeloproliferative disorder characterized by clonal proliferation of magakaryocytes, which in turn leads to thrombocytosis1). Thrombosis and hemorrhage are typical complications in patients with the disease1). The rate of major thrombotic complications, such as acute coronary syndrome or cerebral ischemic attack has been reported, in one large study of patients with essential thrombocythemia, to be 7%2). There have been two prior reports of cases of acute coronary syndrome, as a complication of ET, successfully treated with PCI in combination with cytostatic therapy3, 4). Here we report successful coronary artery stent placement after cytostatic treatment, with hydroxyurea and anagrelide, in a patient with ET who presented with unstable angina.
CASE REPORT
A 45-year-old male was admitted to our hospital due to substernal chest discomfort on mild exertion, which occurred three weeks prior to presentation. The frequency and severity of his angina increased over time and the patient described a squeezing chest pain with an onset three days prior to presentation. The past medical history included hypertension, diagnosed three years ago, and smoking history of ten pack-years. There was no family history of coronary artery or hematologic disease. At the time of admission he was on aspirin and anti-hypertensive medications. On physical examination, the blood pressure was 130/80 mmHg and the heart rate was 70 beats per minute. The heart sounds were unremarkable with normal S1 and S2 sounds. The lungs were clear on auscultation. The electrocardiogram showed no ST-segment change, T wave inversion or pathologic Q waves suggestive of myocardial ischemia. No abnormality was found on chest roentgenogram. On complete blood count, the hemoglobin was 13.9 g/dL, white blood cell count was 9,400/L, and the platelet count was 106×104/µL. Electrolytes, renal and liver function tests were not remarkable. Levels of CK-MB and Troponin-T were within normal range. Total serum cholesterol was 161 mg/dL, triglyceride was 95 mg/dL and high-density lipoprotein was 39 mg/dL. Serum homocystein level was 12.7 nmol/mL (reference range 5-15 nmol/mL), and hsCRP was 1.91 mg/L (reference range <3 mg/L). Prothrombin time, activated partial thromboplastin time and fibrinogen level were within normal range. The iron profile was not remarkable. Bone marrow study showed a hypercellular marrow with markedly increased megakaryocytes, and a normal myeloid/erythroid ratio (Figure 1). Chromosomal analysis of bone marrow cells revealed a normal 46, XY karyotype with no evidence of bcr/abl rearrangement. Liver and spleen were not enlarged on sonogram images. An elective coronary angiography, two days after admission, showed total occlusion at the mid right coronary artery (RCA) with well-developed collaterals from proximal RCA to PD and PL branches. In addition, there was diffuse irregular, up to 70%, luminal narrowing with haziness noted at the proximal RCA. The left coronary angiography showed a 40% luminal narrowing at the mid left anterior descending artery (LAD). The echocardiography, performed three days after admission, showed no regional wall motion abnormality with about 60% of left ventricular ejection fraction. On color Doppler imaging, there was no significant valvular stenosis or regurgitation noted. There was a relaxational abnormality observed in the diastolic filling pattern. The patient was taking aspirin 100 mg/day, clopidogrel 75 mg/day, atenolol 25 mg/day, diltiazem 90 mg/day and nicorandil 15 mg/day from the day of admission. The chest pain was controlled by medical treatment; therefore, we decided to postpone coronary artery intervention until the platelet count reached a normal level. Treatment with hyroxyurea 500 mg/day and anagrelide HCl 1 mg/day was started as cytostatic therapy. The platelet count was normalized (23×104/µL) five weeks after initiation of cytostatic therapy, and coronary artery intervention was then performed. The totally occluded mid RCA lesion was thought to be a chronic total occlusion because of the presence of good collateral flow from the proximal RCA. We thought that the proximal RCA, stenotic lesion with haziness, resulted from a plaque rupture resulting in an occlusive thrombus, and caused the ischemic symptoms that the patient presented with. Two coronary stents were placed at the proximal and mid RCA. No residual stenosis was observed after the procedure (Figure 2). The LAD lesion was not treated. The patient was discharged two days after the procedure without any hemorrhagic or thrombotic complication; he remained on aspirin, clopidogrel, hydroxyurea, and anagrelide. The patient was free of symptoms for six months during the follow-up period, and his platelet count remained within normal range.
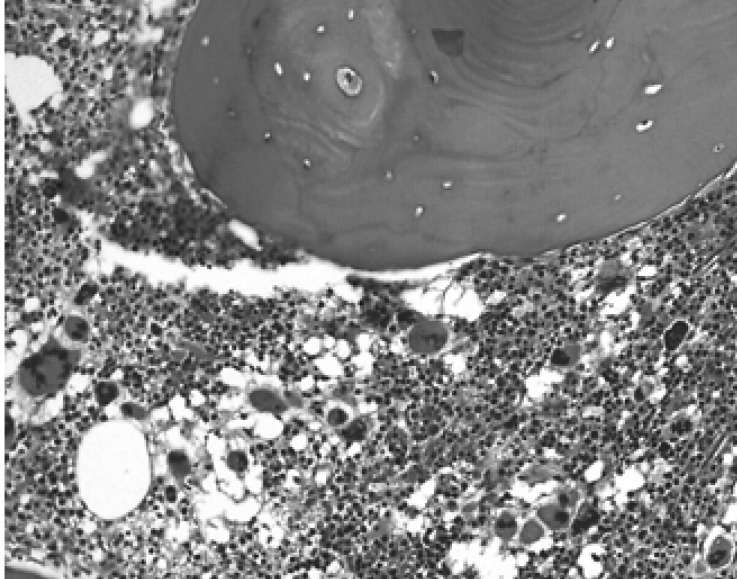
Bone marrow biopsy. Abundant number of megakaryocytes with atypical forms is shown, consistent with the diagnosis of essential thrombocythemia (H&E stain, ×200).
DISCUSSION
ET occasionally presents with arterial and/or venous thrombosis, and less frequently with hemorrhagic complications. These thrombotic and vascular complications are the main causes of death in patients with ET1, 5, 6). Although ET may cause vascular thrombosis and tissue ischemia, coronary artery involvement, with acute coronary syndrome, is very uncommon. Only about 21 such cases have been described in the medical literature, and four of these cases were reported to be treated with coronary angioplasty and stent placement3, 4, 7, 8).
Among the four patients with an acute coronary syndrome complication of ET, two patients received percutaneous coronary angioplasty with stent placement without any cytostatic therapy. These patients suffered from the complication of stent thrombosis after the procedure7, 8). The other two had unstable angina as a complication of ET and they received percutaneous angioplasty with stent placement along with cytostatic and antiplatelet therapy3, 4). Their post-procedure course was uneventful, and they were discharged without any thrombotic complication.
With advancement and availability of coronary angioplasty techniques, coronary intervention with stent placement, for ET patients, is becoming common. However, as described above, the rate of in stent thrombosis is very high (two out of two cases) in patients who were not given cytostatic and antiplatelet agents. These facts suggest that aggressive inhibition of platelet aggregation and production, before and after angioplasty, might play an important role in the treatment of coronary artery diseases in patients with ET.
There are two forms of cytostatic therapy, cytostatic agents and platelet apheresis Prompt and aggressive use of hydroxyurea is warranted in any patient with who has active cardiovascular ischemia6). The recommended starting dose is 1 5~30 mg per kilogram of body weight per day; however, the dose should be adjusted to achieve optimal control of thrombocytosis without the complications of anemia or leucopenia9-11). The appropriate time to perform coronary angioplasty, with stent placement, should be based on individual patient presentation. It is reasonable to perform PCI after the platelet count is less than 40×104/µL, as long as recurrent ischemia can be prevented with medical treatment11). Mitsunori et al. reported a successful PCI with stent insertion after three weeks of cytostatic therapy with 1,500 mg/day of hydroxyurea. However, we administered 400 mg/day of hydroxyurea for five weeks in our case.
In patients with acute myocardial infarction or unstable angina/non-ST elevation myocardial infarction, primary PCI or early invasive intervention must proceed without hesitation regardless of the patients??platelet counts. In an emergency situation, platelet apheresis can provide effective and relatively safe reduction of platelet counts in a short time11). Tansel et al. reported a case with successful platelet apheresis after PCI in patients with ET7). As the beneficial effect of platelet apheresis is generally short-lived it is essential to initiate cytostatic therapy at the same time11).
Anagrelide and alpha-interferon are additional cytostatic agents. A report from Sandra et al., and our own experience, suggests that no thrombotic complication with anagrelide use along with coronary artery interventions. The antithrombotic effect of these agents has never been proven; moreover their use is limited in certain situations i.e. alpha interferon is contraindicated in thyroid disease or in patients with psychiatric disorders; anagrelide is contraindicated in patients with severe cardiovascular disease and used with caution in patients who have documented coronary ischemia9).
Antiplatelet agents, aspirin and adenosin dephosphate inhibitor are usually given to the patients who have PCI; aspirin appears to be beneficial also in patients with ET. The incidence of thrombosis was significantly reduced following aspirin administration particularly at a lower dose (100 mg/d)12). However, the proper maintenance dose, duration of treatment and benefit of aspirin and adenosin dephosphate have to be further defined in future clinical investigations in patients with coronary artery disease and ET. It is probable that the platelet glycoprotein IIb/IIIa receptor inhibitor plays a crucial role in treating ET-associated ischemic syndromes with coronary thrombus. There is one case report documenting the successful use of abciximab with PCI in ET-associated coronary thrombosis13).
In conclusion, antiplatelet cytostatic treatment played a critical role in coronary angioplasty with stent placement in patients with ET and coronary artery disease. Further clinical trials are needed to evaluate the efficacy of these agents in coronary artery disease with ET.
