Prevalence of Helicobacter pylori Infection in Patients with Peptic Ulcer Diseases and Non-Ulcer Dyspepsia
Article information
Abstract
Background:
Helicobacter pylori is known to be a cause of active chronic gastritis and has been proposed as an etiologic factor in the development of peptic ulcer disease, but controversy continues regarding the pathogenic importance and mechanism. We examined the prevalence of H. pylori infection in patients with peptic ulcers and non-ulcer dyspepsia.
Method:
749 patients (373 with duodenal ulcer, 303 with gastric ulcer, 73 with non-ulcer dyspepsia) were included. Endoscopic mucosal biopsies were done at antrum, duodenum, and, if present, ulcer margin. The specimens were tested by Gram staining, Giemsa staining, culture, urease testing for identification of H. pylori. Antibody to H. pylori was examined in 83 patient of these patients by ELISA, and the result was compared with the results of bacteriologic studies.
Result:
Prevalence of H. pylori in antral mucosa was higher in patients with duodenal ulcers (81.5%) than in patients with gastric ulcer and non-ulcer dyspepsia (56% and 52.8%) (P<0.05). Also in the duodenal mucosa of non-ulcer sites, and the ulcer margin of patients with duodenal ulcers, the detection rates (12% and 40.7%) were higher than those in the duodenal mucosa of patients with gastric ulcer and non-ulcer dyspepsia (7% and 8%)(p<0.005). Antibody to H. pylori was detected in all patients with duodenal and gastric ulcers and non-ulcer dyspepsia who were tested for antibody. In contrast, the detection rates of antibody in adult control and child control were 33.3% and 27%. Among patients with antibody to H. pylori, H. pylori was detected in 85.7% of patients with duodenal ulcer, 62.5% of patients with gastric ulcers and 22.2% of patients with non-ulcer dyspepsia(p<0.05).
Conclusion:
These data suggest that H. pylori is a possible pathogen for duodenal ulcer by duodenal colonization probably via gastric metaplasia. Also the past or present infection of H. pylori in antral mucosa may play a role at least partially in generation of upper gastrointestinal symptoms.
INTRODUCTION
In 1983, Marshall et al had observed curved bacilli by silver stain in gastroscopic biopsy specimens from patients with peptic ulcer and chronic gastritis and had succeeded in the culture and identification of this organism1). They had reffered to this organism as Complylobacter pyloridis due to the morphologic resemblance to Campylobacter genus2) and proposed the possible a causal role of the bacterium in peptic ulcer diseases. It has been recently recognized as the type species of a new genus-termed ‘Helicobacter’1,3). Now Helicobacter pylori is considered to be a causative organism of active chronic gastritis, but its pathogic role in peptic ulcer disease in not established.
We studied the prevalence of Helicobacter pylori in patients with duodenal ulcer, gastric ulcer and non-ulcer dyspepsia in Korea by several bacteriologic tests and a sereologic test, in order to investigate the possible etiologic role of the bacteria in peptic ulcers and to find the ideal method for the identification of H. pylori.
MATERIALS AND METHODS
1. Patients
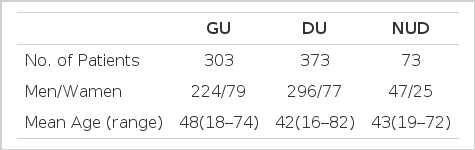
748 patients, who were referred for gastroscopy due to upper gastrointestinal symptoms between 1990 and 1992, were inclued. They included 373 patients with duodenal ulcers, 303 with gastric ulcers and 73 with non-ulcer dyspepsia. There was no difference in sex and age distribution among groups with each disease entities (Table 1).
2. Endoscopic Biopsy
Four pieces of biopsy specimens were taken from the antral mucosa within 5 from pyloric ring, the duodenal mucosa and ulcer margin, respectively. Two samples from each site were fixed in formalin for histology and Giemsa stain, and the other two samples in 1 cc of sterile saline were brought to the microbiology laboratory. All specimens were innoculated for culture within 2 hours after collection. For prevention of bacterial contamination to other sites and false positive results, the forceps and endoscope used were disinfected with benzalconium and 90% alcohol, and rinsed by sterile saline before next use.
3. Bacteriology
Each fresh endoscopic biopsy specimen was grinded on the ground glass grinder, then were innoculated in chocolate agar and Cristensen’s urea agar for an urease test, and the remainder was smeared over a microscopic slide and stained by Gram’s method. The innoculated agar plates, to which 3 mg/dl vancomycin and 10 mg/dl nalidixic acid were mixed for inhibition of growth of other contaminated bacteria, were incubated for seven days at 37°C in an atmosphere of 17% CO2, 90% humidity.
If specific water drop-like transparent colonies on chocolate agar were formed, they were identified with positive reaction for catalase, urease and oxidase, and inspection of gram-negative curved bacilli with Gram staining.
The Cristensen’s urea agar slants were examined after 30 minutes and 1, 2 and 24 hours of incubation for a change in color from light tan to bright pink. The color change was interpreted as positive.
4. Serology
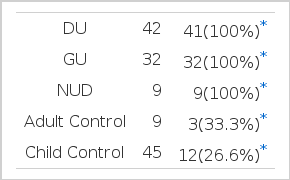
Antibodies to H. pylori were tested in the sera of 42 patients with duodenal ulcers, 32 with gastric ulcers, 9 with non-ulcer dyspepsia, who were subjected to endoscopy, and a control group who did not undergo endoscopy. This control group included 9 asymptomatic adults and 45 children patients admitted in pediatric department for various disease. Fifteen patients with initially positive results for antibody and bacteria were retested after the eradication of H. pylori by antimicrobial therapy for 4 weeks. Antibody was detected by ELISA for the presence of IgG class antibody to H. pylori (Roche Co.).
5. Statistics
Abinomial test and an X2 test were used to test statistcal significance. A probability of less than 5% was considered to be significant.
RESULTS
1. Comparison of Results of Gram Staining, Giemsa Staining, Culture, and Urease Testing for H. pylori:
H. pylori was detected by Gram staining, Giemsa staining, culture and urease test in 71.1%, 65.4%, 56.9% and 40.0%, respectively (Table 2). The highest detection rate was obtained by Gram staining. The correction between Gram staining and Giemsa staining was above 95%. By Giemsa staining, the organism was always noted to be present beneath the mucus layer.
2. The Detection Rate of H. pylori According to Disease Entities:
Table 3 and Figure 1 show the results of bacteriologic studies. Identification of the bacterium by Gram staining, culture or both was considered to be positive. In patients with duodenal ulcer H. pylori was detected in 304 of 373 patients in antral mucosa (81.5%). In contrast, in patients with gastric ulcer and non-ulcer dyspepsia, the detection rates of H. pylori were 56% and 52.8%, respectively (p<0.01) (Table 3).
The detection rate of H. pylori in duodenal mucosa was higher in patients with duodenal ulcer than in patients with gastric ulcer and non-ulcer dyspepsia (12% vs 7% and 8%) (p<0.05) and there was no difference in the detection rate between patients with gastric ulcer and those with non-ulcer dyspesia.
In patients with duodenal ulcer, the detection rate of H. pylori in the ulcer margin was higher than in non-ulcer sites of the duodenum (40.7% vs 15%) (p<0.005), but in gastric ulcer patients there was no significant difference in the detection rate of H. pylori between the ulcer margin and non-ulcer site of antrum (54% and 56%).
3. The Detection Rate of H. pylori According to Sex and Age:
There was no significant difference in the detection rate of H. pylori according to age and sex in groups of each disease entities.
4. The Detection of Antibody to H. pylori:
Antibody to H. pylori was detected in all of 42 patients with duodenal ulcer, 32 with gastric ulcer and 9 with non-ulcer dyspepsia who were tested. In contrast, the antibody was detected in 3 of 9 normal healthy adult controls (33.3%) and 12 of 45 child controls (26.6%) (p<0.05) (Table 4). Antibody to H. pylori was detected in 13 of 15 patients who had the antibody before treatment and who retested after the eradication of H. pylori.
5. Comparison of the Results of Serologic Testing and Bacteriologic Testing:
Among the patients with antibody to H. pylori was demonstrated by bacteriologic tests in 36 of 42 patients with gastric ulcer (85.2%), 20 of patients with gastric ulcer (62.0%) and 2 of 9 patients with non-ulcer dyspepsia (22.2%) (p<0.05) (Table 5).
DISCUSSION
Spiral organisms have been noted on the gastric mucosa on many occasions over the last 100 years4,5). However, the failure in culture of the organism has caused the organism to be ignored. In 1983 the first successful culture of the spiral gram-negative bacteria from the human stomach was performed by Marshall and Warren, and they proposed an association between the presence of the spiral organism on the gastric mucosa and antral gastritis1). By light microscopy, and in the guanine plus cytosine content of their DNA, these microaerophillic organisms resembled Campylobacters, and so were named Campylobacter pyloridis. However, its ultrasructure and fatty acid composition were found to be very different from those of Campylobacter, and so Goodwin proposed to name the organism Helicobacter pylori6).
Since Marshall suggested that H. pylori was associated with peptic ulcer, especially duodenal ulcer, many reports supported the possibility that H. pylori is a causative factor of duodenal ulcer7,9), but in several reports the association of H. pylori and duodenal ulcer was not noticeable10,11). In this study the detection rate of H. pylori in duodenal ulcer patients was 81.5% and this rate was significantly higher than supported a strong association between H. pylori and duodenal ulceration.
Although the pathogenesis of H. pylori in duodenal ulcer was not clearly established, it has been proposed that gastric metaplasia in the duodenum serves a precursor of duodenal ulceration by providing a nidus for H. pylori colonization and subsequent inflammation12–14). In our study the detection rate of H. pylori in the non-ulcer site of duodenal mucosa (12%) and duodenal ulcer margin (40.7%) of gastric ulcer (71%) and non-ulcer dyspepsia (8.0) (p<0.005). This finding supported the possibility of duodenal colonization of H. pylori and subsequent ulceration. In our study, H. pylori was detected highly beneath the mucus layer of duodenal mucosa in patients with duodenal ulcer. This finding strongly suggests the possible etilogic role of H. pylori colonization in the pathogenesis of duodenal ulcer, although we could not demonstrate gastric metaplasia in duodenal mucosa of duodenal ulcer patients. Malfertheiner et al also have demonstrated intra-and intercellular infiltration of H. pylori of the duodenal epithelium by EM15).
In patients with gastric ulcer, the detection rate of H. pylori in antral mucosa was lower than in patients with duodenal ulcer (50% vs 81.5%) (p<0. 05) and was not different from that of patients with non-ulcer dyspesia.
In this study the positive rates of culture and urease testing were lower than those of Gram and Giemsa stain. The positive rates of these stains are similar to the results of other reportists16). The lower detection rate of culture media is due either to the delay in inoculation of bacteria in culture media or to difficulty in maintaining humid and microaerobic conditions. Thus we suggest the need of the combination of culture and stains for high detection rate of H. pylori.
In this study, antibody to H. pylori was detected in all of 83 patients with gastric and duodenal ulcer and non-ulcer dyspepsia who were tested for antibody to H. pylori, in contrast to the lower detection rate (33.3%) in asymptomatic individuals. This finding supports that gastritis due to the present or past infection of H. pylori may be a causative factor of upper gastrointestinal symptoms. Several studies reported that the eradication of H. pylori with colloidal bisthmus significantly improved upper gastrointestinal symptoms and histologic gastritis17,18).
Whether the presence of the antibody to H. pylori means past or present infection is not clear. In our study, 4 weeks after the eradication of H. pylori by colloidal bisthmus subcitrate and metronidazole, the antibody-postive patients was higher in patients with duodenal ulcer (85.7%) than in patients with gastric ulcer (62.5%) and non-ulcer dyspepsia (22.2%). Therefore, we propose that in patients with duodenal ulcer, ulcer formation may be due to reduced power of the eradication of the organism after infection.
Several epidemiologic studies revealed that the frequency of H. pylori in asymptomatic individuals increased with age19,20), but this age-associated increase was not present in patients with peptic ulcer20). In our study, there was no significant difference in the detection rate of H. pylori according to age in patients with duodenal and gastric ulcer and non-ulcer dyspespsia as well. This result supported the possibility that H. pylori may play a role, et lest partially, in the generation of upper gastronintestnal symptoms.
In conclusion, although the pathogenetic mechanism of H. pylori in duodenal ulceration is not clear, H. pylori is closely associated with duodenal ulcer.