Percutaneous Mitral Valvuloplasty Using the Double Balloon Technique: Immediate Results and Determinant Factors of Increasing Mitral Regurgitation
Article information
Abstract
Percutaneous mitral valvuloplasty (PMV) was successfully performed in 112 (95%) out of 118 patients (32 M, 80 F, mean age: 38±11 years) with mitral stenosis. There was a significiant increase in the mitral valve area (MVA) from 0.9±0.2 to 2.0±0.7 cm2 p<0.0001, a decrease in the mean mitral gradient from 17±6 to 6±3 mmHg, p<0.001, and a rise in cardiac output from 4.3±0.8 to 4.8±1.2 L/min, p<0.001.
The morphologic features of the mitral stenosis was evaluated using echocardiographic score. Patients with a low-score (≤8) had more effective dilation of mitral stenosis compared to patients with a high-score over 8 (0.9 to 2.2 vs 0.8 to 1.6 cm2, p<0.001), despite the similar EBDA/BSA (effective balloon dilating area/body surface area). The patients with good results after PMV (MVA ≥ 1.5 cm2) were more likely to be in normal sinus rhythm (p<0.0001), younger age (p<0.001), smaller left atrial size (p<0.05), and lower total echoscore (p<0.002), especially in leaflet mobility (p<0.02) and degree of calcification (p<0.002), compared to patients with relatively poor result after PMV (MVA < 1.5 cm2). There were no differences in EBDA/BSA, calcification on fluoroscopy, and history of previous surgical commissurotomy between the 2 groups. Mitral regurgitation (MR) developed or increased in severity in 41 (37%) cases. The patients with an increase in MR had relatively smaller initial MVA (p<0.001) and more thickened valve leaflets (p<0.02). Although there was an increasing trend in total echoscore and EBDA as the severity of the MR increased, those were statistically not significant. Complications included embolic episode in 3 (3%), cardiac tamponade in 3 (3%), and creation of ASD (Qp/Qs≥1.5) in 22 (20%).
Thus this data suggest that valvuloplasty using the double-balloon technique is a safe and effective procedure in selected patients; mitral valve dilation was more effective in younger patients with normal sinus rhythm, smaller left atrium, more mobile and less calcified valve leaflets and lower total echoscore; and an increase in MR after valvuloplasty appeared to be related to initial mitral valve area and valvular thickening.
INTRODUCTION
Mitral balloon valvuloplasty has been established as an effective therapy of mitral stenosis in selected patients1–10), and the mechanism is the splitting of the commissures toward the mitral annulus, resembling the changes seen after surgical commissurotomy11). Therefore, surgical mitral commissurotomy can be avoided in the majority of patients with mitral stenosis. Although an increase in mitral regurgitation after valvuloplasty is frequently seen after this procedure, the determinant factors of increasing mitral regurgitation have not been adequately studied.
Thus, the purpose of this study was to establish the relationship between the increase in mitral regurgitation and the morphologic features of the valvular or subvalvular apparatus by 2-dimensional echocardiography in 118 patients who had a successful mitral balloon valvuloplasty.
METHOD
1. Patients
The patients population included 112 patients with successful PMV out of 118 patients who presented with moderate to severe symptomatic mitral stenosis. There were 32 male and 80 female patients with a mean age of 38±11 years (range 17 to 66 years). The criteria for inclusion was isolated moderate to severe mitral stenosis, either pure or with mild mitral or aortic regurgitation (less than grade 2 out of 4) but no evidence of visible left atrial thrombi and recent systemic embolic episode. Twenty nine patients were in NYHA class II, 73 class III, and 10 class IV. Sixty two patients were in normal sinus rhythm and 50 had atrial fibrillation. Twenty one patients had associated mild mitral regurgitation and 37 had mild aortic regurgitation. Seven patients had fluoroscopic calcification in the valvular and/or subvalvular apparatus of the mitral valve and 7 had previous surgical commissurotomy. The mean total echoscore was 7.8±1.4.
2. Echocardiographic Evaluation of Valvular and Subvalvular Morphology
Two dimensional and Doppler echocardiographic examination were performed before and 1–2 days after mitral valvuloplasty. Images were acquired using a Hewlett-Packard 77020A Ultrasound imager equipped with a 2.5 MHz phase-array transducer. The morphologic features of the stenotic mitral valve and subvalvular structure were evaluated using a semiquantitative scoring system (echocardiographic score 1–4 represents the severity of valve mobility, thickening, calcification, and subvalvular lesions, respectively). The scores from all individual features were added up each patient to obtain a total score12,13).
3. Procedure
Valvuloplasty was performed with a cardiac surgical team on standby. Double balloon technique was used in all 112 patients. Right heart catheterization was performed percutaneously from the right internal jugular vein with a thermodilution Swan-Ganz catheter. A 7F pigtail catheter was placed percutaneously in the aortic root through the left femoral artery to monitor systemic blood pressure and to guide the trasseptal puncture site. A transseptal puncture of the left atrium was performed from the right femoral vein with an 8F Mullin’s transseptal sheath and dilator (USCI) and a modified Brockenbrough needle. Systemic heparinization was achieved by 100 U/kg heparin. A 7F wedge balloon catheter was introduced into the left atrium, left ventricle and placed into the ascending aorta through the Mullin’s sheath. A 0.038 inch 260 cm long exchange guide wire was passed via the wedge balloon catheter, and the distal tip was placed in the descending aorta below the diaphragm.
The Mullin’s sheath and wedge balloon catheter were then removed, leaving the guide wire behind. The interatrial septum was dilated with an 8 mm balloon dilating catheter (Mansfield). A second exchange guide wire was passed through the same atrial puncture parallel to the first wire through a special double-lumen catheter (Block). One balloon dilating catheter (Mansfield) was advanced over one of the guide wires through the left atrium and across the mitral valves. A second balloon dilating catheter was passed parallel to the first one over the other guide wire. The 2 valvotomy balloon catheters were inflated simultaneously by hand until the indentation of the balloon due to the stenotic mitral valve disappeared. Inflation-deflation time was approximately 15–20 sec and balloon inflations were done 2 to 3 times to ensure that the balloon catheters were in correct position across the mitral valve.
The balloon size was selected on the basis of effective balloon dilating area per body surface area. A combination of 2 separate balloon catheters, ranging from 15 to 25 mm, was used in all patients. Immediately after the valvuloplasty, the balloon dilatation catheters were removed. Thereafter cine left ventriculography in the right anterior oblique view was performed in all patients to evaluate the severity of mitral regurgitation. Finally a right heart oxymetric study was performed to assess left-to-right shunting through the atrial septum.
Right and left heart pressure, mitral gradient, and cardiac output were measured before and after PMV. Cardiac output was determined by thermodilution in most of the patients. However if left-to-right shunting occurred after PMV, systemic blood flow was obtained according to the Fick’s principle, using the superior vena cava oxygen content as the mixed venous sample. The mitral valve area was calculated by Gorlin’s formula. The procedure was completed within 2 hours in all patients.
3. Grading of Mitral Regurgitation
To assess the severity of mitral regurgitation, the left atrium was divided into 4 equal segments extending from the annular plane to the superior wall of the left atrium.
Mitral regurgitation was graded from 1+ to 4+ according to the distribution of the regurgitant jet within the atrium12). Grade 1+ represents abnormal systolic flow that extended to the proximal quater of the left atrium and grade 4+ represents regurgitant flow extending beyond 3 quaters of the left atrium. In patients with atrial fibrillation. Doppler assessment of mitral regurgitation was taken from the average of multiple beats.
4. Statistical Analysis
Hemodynamic measurements before and after valvuloplasty were compared using the Student’s paired t test for parametric data. To identify the factors that influence immediate results after valvuloplasty, the study group was divided into those patients with MVA ≥ 1.5 cm2 after PMV and those patients with MVA < 1.5 cm2. In order to evaluate the determinants of the increasing mitral regurgitation, the entire group was divided into those patients who had new or an increase of mitral regurgitation by grade one or more after valvuloplasty and those in whom mitral regurgitation did not develp or change.
Comparisons of these 2 groups were made using the Student’s unpaired t-test and Anova one way test. The frequency of events was compared by the Chi-square or Fisher’s exact test.
Multiple regression analysis was performed in the standard manner with a commercial statistical package, SPSS/PC+. Differences were considered significant at p<0.05. Data are presented as mean±SD.
RESULTS
The procedure was discontinued in 1 patient because of failure of the balloon to traverse the stenotic mitral orifice. One patient has hemopericardium due to injury to the posterior wall of the left atrium by transseptal procedure and has emergency mitral valve replacement. In 1 patient with previous surgical commissurotomy, the procedure was completed technically but the mitral valve orifice couldn’t be dilated because of severe subvalvular thickening and heavy calcification.
1. Hemodynamic Variables
Balloon valvuloplasty resulted in an increase in mitral valve area from 0.9±0.2 to 2.0±0.7 cm2 (p<0.0001, Fig. 1), and a significant decrease in transmitral pressure gradient from 17±6 to 6±3 mmHg (p<0.0001). PMV resulted in a significant decrease in mean pulmonary arterial pressure from 29±14 to 20±9 mmHg (p<0.0001), and left atrial pressure decreased from 22±7 to 9±5 mmHg (p<0.0001, Fig. 2). Calculated pulmonary vascular resistance decreased significantly from 226±168 to 175±119 dyne.sec.cm-5 (P<0.0001). Cardiac output determined by thermodilution increased from 4.3 to 4.8 L/min.
Mean mitral valve area (MVA) increased from 0.9 to 2.0 cm2 after valvuloplasty. *p<0.0001 for pre vs post; MVA (1): by Gorlin’s method; MVA (2): by 2-dimensional echocardiography; MVA (3): by doppler pressure half time.
Hemodynamic parameters showed significant improvements after valvuloplasty Mean mitral gradient (MG) decreased from 17 to 6, mean left atrial pressure (LAP) decreased from 22 to 9 mmHg, mean pulmonary artery pressure (PAP) decreased from 29 to 20 mmHg. *p<0.001 for pre vs post.
Symptomatic improvement after valvuloplasty in hospital course occurred in all but 4 patients. One hundred six patients were judged to be in NYHA class I and II. Two patients underwent successful mitral valve replacement after inadequate valvuloplasty. Twenty four patients increased mitral regurgitation by one plus, 13 patients increased by 2 plus and 4 patients increased mitral regurgitation by 3 plus.
2. Predictors of Good Results
Although the mitral valve area immediately after dilatation increased in almost all of the patients, 17 patients (15%) had relatively poor results (MVA after PMV < 1.5 cm2). In order to evaluate the factors influencing the immediate results, we compared clinical and echocardiographic variables between these 17 patients and the remaining 95 patients with MVA of 1.5 cm2 or more after valvuloplasty. Mitral valve dilation was more effective in younger patients (p<0.0001) with normal sinus rhythm (p<0.0001), smaller left atrium (p<0.05), more mobile (p<0.02) and less calcified valve leaflets (p<0.002) and lower total echo-score (p<0.002, Table 1). However, initial MVA, valvular thickening, subvalvular lesions and EBDA/BSA were not significantly different between the 2 groups. We compared the echocardiographic variables between the patients with low echo-score (≤8) and those with high echo-score (>8). The patients with low echo-score had a smaller left atrium (p<0.01) and more increase in MVA (p<0.0001) after valvuloplasty, despite a similarity in effective balloon dilating area (Table 2). Multiple regression anaysis of these variables was performed, and we found the single most important factor influencing the immediate results was total echocardiographic score.

Comparison of Clinical and Echocardiographic Parameters Between Patients with MVA < 1.5 and with >1.5 cm2 After PMV
3. Mitral Regurgitation
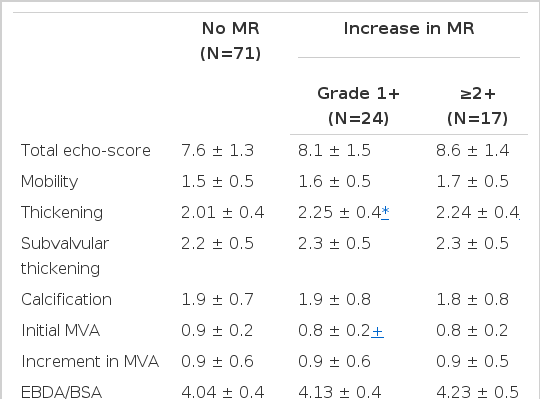
Mitral regurgitation either developed or increased in severity in 41 patients (37%). New mitral regurgitation developed in 31 patients and increased in 10. An increase in mitral regurgitation by grade 1+ occurrred in 24 patients (21%), by grade 2+ in 13 (12%) and grade 3+ in 4 (4%). To evaluate echocardiographic variables affecting the increase in mitral regurgitation after valvuloplasty, the patients were divided into 3 groups, no mitral regurgitation in 71 patients, increase in mitral regurgitation by grade 1+ In 24, by grade 2+ or more in 17. The valvular thickening (p<0.02) and initial mitral valve area (p<0.001) were statistically significant factors affecting an increase in mitral regurgitation (Table 3). Although there was an increasing trend in the total echoscore and EBDA as the severity of the mitral regurgitation increased, those were statistically insignificant. Multiple regression analysis suggested that the most important factor of worsening mitral regurgitation after valvuloplasty was a smaller initial mitral valve area.
4. Complications
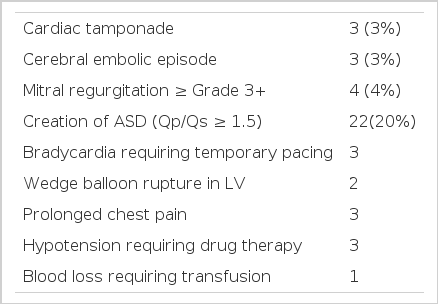
Major complications included cardiac tamponade in 3, cerebral embolic episode in 3, severe mitral regurgitation in 4 patients, and creation of significant left to right shunt (Qp/Qs>1.5) in 22 (20%). Although we did not have mortality during the procedure, one of 3 with cerebral embolism developed cerebral infarction and died 7 days after the procedure. One of 3 with cardiac tamponade had emergency mitral valve replacement and the remaining 2 patients had received pericardiocentesis followed by successful mitral valvuloplasty on the following day. Three patients developed bradycardia requiring temporary pacing. Prolonged chest pain after the procedure occurred in 3, hypotension requiring drug therapy in 3, and wedge balloon rupture in the left ventricle in 2 patients (Table 4)
DISCUSSION
Since the initial report of successful percutaneous transvenous mitral commissurotomy by Inoue in 198413), PMV using balloon catheter has been used as an effective nonsurgical therapy for the least few years even in the patients with calcific mitral stenosis and restenosis after surgical commissurotomy14,15). Recently, PMV has become the treatment of choice for selected patients with moderate to severe mitral stenosis without significant mitral regurgitation, but mitral regurgitation can develop following this procedure.
This study has demonstrated immediate hemodynamic improvement after PMV, but 37% of the patients either developed or increased mitral regurgitation after this procedure.
With current technology, effective balloon dilatation may not be achieved by using a single balloon16). Thus we performed valvuloplasty using the double balloon technique in all of our patients. Immediate hemodynamic changes after technically successful PMV resulted in a significant increase in mitral valve area and cardiac output and a significant decrease in the mean diastolic transvalvular mitral gradient, left atrial pressure, pulmonary artery pressure, and pulmonary vascular resistance.
These hemodynamic data are in agreement with previous reports1–6). Previous investigators suggested that the major determinant of the outcome is the morphologic severity of the mitral valve17,18), which is consistent with analysis of the results after surgical commissurotomy19). A simple comparison of echocardiographic and clinical variables between the good and relatively poor results (MVA after dilation <1.5 cm2) groups demonstrated that younger age, normal sinus rhythm, smaller left atrial size, and lower total echo-score, especially mobility and degree of calcification, are related to good results after valvuloplasty.
In our study, the total echocardiographic score is the most important factor on the immediate outcome by multiple regression analysis. Moreover we found that patients with low echo-score (≤8) had a more significant increase in MVA than those with high echo-score (>8) after the PMV despite a similar effective balloon dilating area. Although it has been suggested that the balloon size might have an important role for immediate hemodynamic results, the difference in mean EBDA/BSA between the 2 groups was not statistically significant.
Mitral regurgitation is an important complication of percutaneous balloon valvuloplasty. The importance of this complication after valvuloplasty or surgical commissurotomy has been emphasized by its association with a poor prognosis20,21). However the factors that may influence the production or exacerbation of mitral regurgitation after valvuloplasty have not been clearly established.
Palacios IF, et al.22) reported that the only important factor of worsening mitral regurgitation was EBDA/BSA. In our study, although we have used relatively larger EBDA/BSA (mean 4.02), the incidence of increasing mitral regurgitation occurred in 37% of the patients, but only 10% of them had grade 3+ increment in mitral regurgitation after the valvuloplasty. In selected patients with low echo-score (<8), especially with preserved mobility and less thickened mitral valve, valvuloplasty could be performed successfully without an increase in mitral regurgitation using relatively large balloons with an EBDA/BSA between 4.3 and 4.5.
A Uni-variate analysis of echocardiographic findings between those patients with and without an increase in mitral regurgitation demonstrated that valvular thickening and smaller initial valve area were important factors for the worsening of mitral regurgitation. Although there was an increasing trend in total echo-score and EBDA/BSA as the severity of the mitral regurgitation increased, those were statistically insignificant. There were no statistical differences in age, sex, cardiac rhythm, previous surgery and fluoroscopic calcification between the 2 groups with and without increasing mitral regurgitation.
CONCLUSION
This study demonstrated that the immediate results after valvuloplasty are mainly determined by valve morphology, that is total echocardiographic score. However age, cardiac rhythm, and left atrial size before valvuloplasty appear to be related to the immediate outcome. The factors related to the worsening of mitral regurgitation after dilation appear to be valvular thickening and smaller initial valve area.
The mean total echo-score of our study patients was 7.8 and the mean age was 38 years old, which suggest that our patients were relatively younger in age and had a lower echo-score compared to patients of other studies1,8,9,14). These patients with less advanced valvular deformity had the most favorable immediate results after valvuloplasty, which suggests that it is preferable to perform the procedure before advanced valvular deformities appear.
Acknowledgements
We wish to thank Jong-Koo Lee for his review of the manuscript and Mr. Chang-sun Choi for his devoted technial assistance.