Long-term Therapy of Hypertension*
Article information
INTRODUCTION
Hypertension is a major chronic disorder which calls for a long-term treatment. The success or failure of the treatment of chronic diseases depends largely on the compliance of patients. So, the success of the treatment of hypertension will be influenced by good compliance, ideal antihypertensive agents and the improvement of the system which can lower medical expenses.
The long-term use of antihypertensive agents causes adverse effects and tolerances. Some kind of antihypertensive agents have an effect on the metabolic aspects, particularly like the worsening of the serum lipids and lowering of the glucose tolerance.
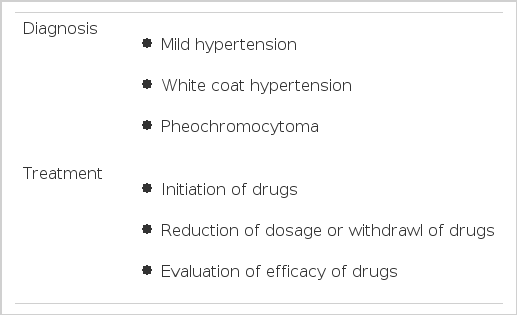
Recently, the availability of the ambulatory blood pressure monitoring is being emphasized in the diagnosis of hypertension, the timing of initiation or withdrawal of antihypertensive agents and evaluation of the efficacy of the drugs.
On the other hand, the frequency and the predicting parameters of the complication, which occurs during the treatment, should be considered in relation with other risk factors and special consideration is needed for the selection of the antihypertensive agent when the concurrent disorder is present.
We1,2) have urged the interest of physicians on the several problems as above which were accompanied by the long-term therapy with antihypertensive agents, and would like to report the result of analysis of the data, which has been gathered in the hypertension clinic of Seoul Paik Hospital, Inje University for 15 years, in order to recollect these problems and draw out the resolutions.
Long-Term Therapy and Compliance
The core of the effective long-term therapy with antihypertensive agents is to improve the compliance of patients. The high compliance results from the interaction among patients, doctors and social conditions. Nessman et al. recommended the following as methods which could improve compliance. The first one was utilization of the educational materials. The second, education of health care officials. The third, home visiting. The fourth, home care. The fifth, measurement of blood pressure at home.
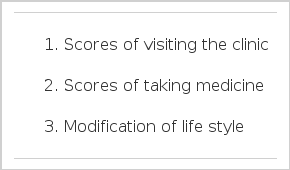
The measurement of compliance can be done by several methods. In our clinic, it has mainly been measured in terms of the scores of visiting the clinic. In other clinics, it has been measured in terms of the scores of taking medicine3). But the modification of the life style should be considered in measuring compliance. (Table 1)
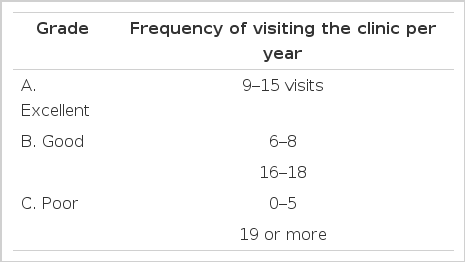
The classification of compliance depends on investigators. The author adopted the system which classified excellent, good and poor according to the frequency of visiting the clinic every month per year. The authors reported several papers which suggested methods for improving compliance. (Table 2)
We recruited 400 patients who visited the hypertension clinic for the first time, received the baseline study and were followed-up more than once after medication. The first 100 patients were treated as usual4). The second 100 patients were given positive intervention by physicians5). The effect of extended insurance coverage was observed in the third 100 patients6). The additive effect of positive intervention by physicians and extended insurance coverage was observed in the last 100 patients7). (Table 3) On the other hand, we recruited 400 patients who were followed for from more than 1 year to 15 years and divided them into 2 groups ; the drop-out group and the non-drop-out group. We checked the scores of visiting the clinic, background and frequency of complications of each group and compared them with each other. We also checked compliance and the duration of visiting the clinic of all patients. We analyzed the relationship between the frequency of use of the first-line antihypertensive agents and compliance.
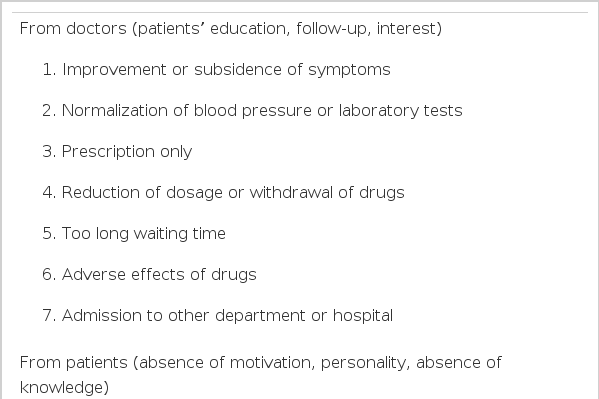
The drop-out rates at the end of 1 year of each group were 63%, 55%, 65% and 52% respectively. The mean rate of all patients was 59 %. (Table 4) The reasons for drop-out came from doctors in 51%, patients in 33% and social systems in 16%. (Fig. 1) The reasons from doctors were 1) improvement or subsidence of symptoms, 2) normalization of blood pressure or the laboratory tests, 3) drop-out due to prescription only, 4) drop-out after reduction of the dosage or withdrawal of drugs, 5) too long waiting time, 6) adverse effects of drugs and 7) admission to another department or another hospital. The reasons from patients were 1) consultation from another department 2) other more serious diseases, for example, neuralgia, 3) needing only medical certificates, 4) overseas travel or long-term business travel, 5) movement of residence, 6) concomitant medication and 7) medical personnel in the family. The reasons from the social system were 1) limitation of insurance coverage, 2) disqualification of the insured, 3) too expensive medical charge, 4) fear from long-term use of drugs, 5) favor for other drugs or doctors and 6) influence of advertisements. (Table 5)
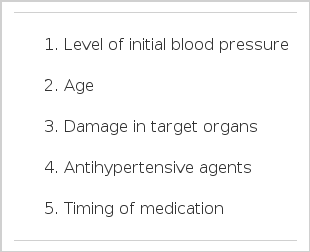
Compliance was improved by positive intervention by physicians but there was no influence from extended insurance coverage. Monotherapy of an antihypertensive agent resulted in better compliance than combination therapy. Compliance was good in cases with complications and high diastolic blood pressure. Compliance was in proportion to the level of initial blood pressure. In the early period of treatment, compliance was good in female patients but it was bad in younger aged group. Compliance was good in the group which had damage in the target organs. Beta blocker, diuretics and alpha blocker had better compliance in that order. (Table 6)
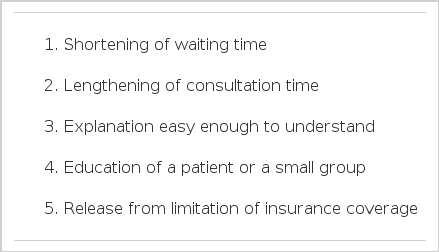
To improve compliance, positive intervention from the medical side, such as extension of the consultation time, shortening of waiting time, explanation easy enough to understand, public relations and education etc., is necessary. Particularly, special interest should be given to young, asymptomatic patients with mild hypertension and the policies of health officials, such as release from limitation of insurance coverage must be changed as soon as possible. (Table 7)
Long-Term Antihypertensive Therapy and Serum Lipids
The conclusion of recent epidemiologic studies was that the mortality of coronary artery disease was not reduced inspite of treatment of hypertension. One of the reasons was deterioration of serum lipid profile by antihypertensive agents. According to the report of MRFIT8), the mortality of coronary artery disease was 4 times higher in 12,866 patients treated with diuretics than that in the control group, and the overall mortality was also higher in the treatment group9).
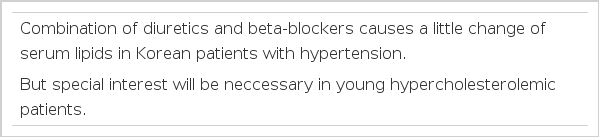
Hypercholesterolemia induced by thiazide was reported10) and an increase of total cholesterol and a decrease of HDL-cholesterol by beta-blocker was also reported11). But the incidence of coronary artery disease is low and the incidence of cerebrovascular attack is high in Korea, and the dosage of diuretics is usually low here in Korea. So the impact of diuretics may be different from western countries12–16).
Acebutolol 400 mg and hydrochlorthiazide 25 mg, which were divided 2 times a day, were given to 28 patients for 24 weeks. Blood pressure, adverse effects and serum lipids were monitored before medication, 6, 12 and 24 weeks after medication13). The effect of combination therapy with prazosin was also evaluated.
The change of total cholesterol was +6% (5% increase in average) and the change of triglyceride was +7%. They were not significant statistically. That is to say, short-term (12 weeks) medication deteriorated the level of total cholesterol, triglyceride and HDL-cholesterol a little bit. The levels of total cholesterol and triglyceride were normalized after long-term (24 weeks) medication but the level of HDL-cholesterol was kept low. (Table 8)
At the same time, the frequency of using antihypertensive agents as the first-line drug was examined annually. The frequency of beta-blocker decreased transiently in 1990 but it increased again in 1993. The frequency of diuretics and Ca channel blocker increased markedly. The overall frequency showed that the major 3 antihypertensive agents were Ca channel blocker, diuretics and alpha-blocker. (Fig. 2) The cross-study at the end of 1992 showed that the first-line antihypertensive agents were Ca channel blocker, beta-blocker and diuretics in the order of frequency, and the major 3 antihypertensive agents among all agents, without consideration of the first-line drug, were alpha-blocker, Ca channel blocker and diuretics. (Fig. 3)
Trend of use of antihypertensive agents.
A: alpha-blockers
B: beta-blockers
C: calcium antagonists
D: diuretics
E: converting enzyme inhibitors
AB: alpha-blocker plus beta-blocker
BD: beta-blocker plus diuretics
Combination therapy with diuretics and beta-blocker caused a little change of the serum lipids in Korean patients with hypertension. But a periodic monitoring of the serum lipids should be done in patients who need long-term medication or patients with hypercholesterolemia. (Table 9)
Initiation of Antihypertensive Agents and Evaluation of Drug Efficacy by Ambulatory Blood Pressure Monitoring
The initiation of antihypertensive therapy should be considered thoughtfully because it would be continued life long. When diastolic blood pressure did not decrease lower than 100 mmHg, inspite of modification of the life style, or when the arteriosclerotic change of the retina is higher than the 2nd degree, or when proteinuria is present, antihypertensive therapy can be started. But casual blood pressure monitoring does not differentiate white coat hypertension which occupies 20–30% of mild degree hypertension from true hypertension17,18). More than 70% of patients with essential hypertension belongs to the mild degree.
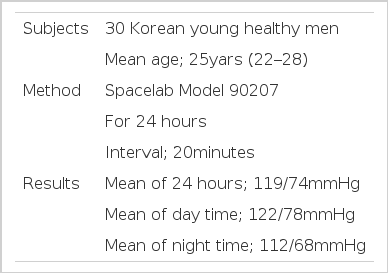
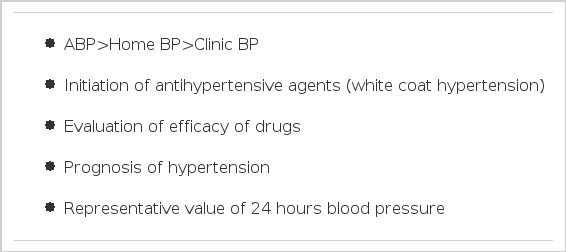
Ambulatory blood pressure monitoring, which can measure blood pressure non-invasively, intermittently and indirectly, should be considered in diagnosing hypertension. In addition, ambulatory blood pressure monitoring is useful in screening pheochromocytoma and malignant hypertension. In respect of treatment, ambulatory blood pressure monitoring is helpful in evaluating the efficacy of antihypertensive agents and in making decisions in initiation of medication and reduction of dosage or withdrawal of antihypertensive agents19). (Table 10)
There is no agreement on the normal value of ambulatory blood pressure monitoring yet. The author suggested 119/74 mmHg as the normal value of Korean young men (the 3rd bdecade) tentatively 20). (Table 11) Pickering in United States suggested 114/77 mmHg Staessen in Germany 118/71 mmHg, Imai in Japan 119/68 mmHg, and O’Brien in England 123/71 mmHg, respectively. In evaluating the efficacy of drugs, there is a considerable difference between measurement of casual blood pressure and ambulatory blood pressure monitoring21,22). Particularly, ambulatory blood pressure monitoring is essential to evaluating the reduction of blood pressure at night time.
But ambulatory blood pressure monitoring causes inconvenience for patients and gives patients a burden in time and money, so it must be used carefully. In order to resolve these problems, we tried to find the representative value of the mean ambulatory blood pressure for 24 hours. The mean ambulatory blood pressure could be replaced by the mean of blood pressures, measured several times for 2 hours in the morning by ambulatory blood pressure monitoring or the mean of blood pressures, measured 3 times with 15 minute intervals at 8o’clock in the morning with a usual sphygnomanometer. (Fig. 4) The reliability of the casual blood pressure, which was used as a standard in the large-scale epidemiological study or in the clinics was less than that of blood pressure at home and much less than that of ambulatory blood pressure.
It is known that the reliability of ambulatory blood pressure is great in evaluating the prognosis of hypertension so ambulatory blood pressure monitoring should be used more widely. Ambulatory blood pressure monitoring will be a strong weapon in deciding reduction of dosage or withdrawal of antihypertensive agents. (Table 12)
Complications During Long-term Antihypertensive Therapy
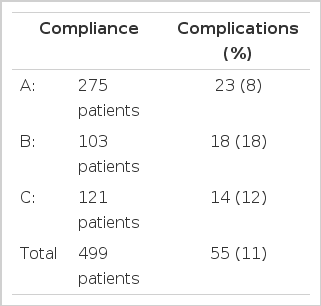
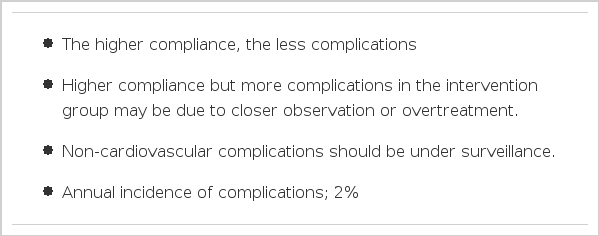
The ultimate goal of antihypertensive therapy is to prevent development or progression of cardiovascular complications by maintaining normal blood pressure. But non-cardiovascular complications, such as malignant tumors and depression, should be under surveillance during a long-term follow-up. The author observed 55 complicated cases in 499 patients with hypertension. They were followed for 5.1 years on average. Cerebrovascular accidents and coronary artery diseases were dominantly frequent. (Fig. 5)

Frequency of complications in each disease group.
CVA: cerebrovascular accident
CAD: coronary artery disease
RF: renal failure
RH: retinal hemorrhage
HF: heart failure
Seki et al. reported the annual incidence of complications of different age groups at the first examination in 1000 patients with hypertension23). Overall incidence of malignant tumors was 6.8; cerebrovascular accident; 15.2, myocardial infarction (including angina), 7.1 and heart failure, 6.6. It is supposed that the patients who are more compliant have less chance of complications. The data of the author showed the same trend. Among the patient group who had excellent compliance, the incidence of complications was 8%. But it was 12% among those who had poor compliance. (Table 13)
Sudden decrease of blood pressure might cause cerebrovascular accidents, such as cerebral infarction or cerebral thrombosis. Marked decrease of blood pressure, within 3 weeks before attack, was found in the cases of cerebral infarction or sudden decrease, as much as 30–70 mmHg, was found in the cases of cerebral thrombosis. Even mild decrease of blood pressure might cause the symptoms of cerebral ischemia in patients with stenosis in the intracerebral arteries.
The blood pressure within 7 days before attack was 14/4 mmHg lower than the usual blood pressure in the cases of myocardial infarction24). Even mild decrease of blood pressure could provoke myocardial infarction in patients with severe coronary artery stenosis. These are the reasons why so called J curve hypothesis is insisted on.
On the data of the author, the annual incidence of complications in the usual treatment group was 19 out of every 1000 patient and that in the intervention group was 22. The reason why the annual incidence of complications was higher in the intervention group is uncertain. But I speculate that it may result from closer observation or overtreatment in the intervention group. (Table 14)
Withdrawal or Reduction of Dosage of Antihypertensive Agents
If proper blood pressure could be maintained for 6–12 months, the dosage of antihypertensive agents can be reduced. After that, withdrawal of antihypertensive agents can be tried. The success rate was 5–10%. It has many advantages, such as reduction of the adverse effects of antihypertensive agents, lowering of economic burden of patients and improvement of the quality of the life of patients, above all.
But if it fails, medication should be re-started during the short period and the compliance of patients will be worsened. So the clinical parameters which can predict the success are necessary. (Table 15, 16)
According to many reports, the success rate of withdrawal was high in patients with hypertension of early stage, mild hyper-tension, low blood pressure before treatment and minor changes of ECG. The author evaluated the possibility of withdrawal in 34 patients and concluded that the duration of withdrawal was longer in patients of early normalization of blood pressure, with low mean arterial pressure before treatment, and patients in whom early trial of withdrawal was possible. The presence or absence of complications at the first examination did not have any relationship with the duration of withdrawal. The rate of re-medication was 53%.
The patient in whom blood pressure was normalized within 3 months after medication is supposed to be a candidate for withdrawal. In the case of re-elevation of blood pressure, the dosage of drugs could be reduced again 6 months after medication and withdrawal of drugs could be re-tried 12–18 months after medication. Withdrawal could be maintained for 9–18 months25). (Table 17)
It will be a message of salvation that reduction of dosage or withdrawal of drugs is possible among patients with hypertension which calls for life-long treatment. Physicians should recommend patients’ participation in the long-term antihypertensive treatment more actively.
CONCLUSIONS
On the way of life-long antihypertensive treatment, there are many obstacles which were described above. They could be removed by the efforts of patients as well as physicians.
This report has some limitation because it is based on the data of only one hypertension clinic. Nation-wide epidemiological study on hypertension is necessary. The program of management of long-term or short-term and the efficient measures should be plotted on the precise understanding of the current situations of this country.
The incidence of hypertension is higher than that of malignancy, hepatitis or diabetes. The economic burden due to complications or sequelae of hypertension is very heavy. All medical personnel, associated social groups and health care officials should make their best efforts to prevent and treat hypertension, which is the most prevalent disease in this country.
Notes
Presented at the 45th (October 1993) annual meeting of Korean Society of Internal Medicine